Abstract
Lactoferrin (LF) has in vitro antiviral activity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This study aimed to determine the effect of bovine lactoferrin (bLF) in the prevention of SARS-CoV-2 infection in health care personnel. A randomized, double-blinded, placebo-controlled clinical trial was conducted in two tertiary hospitals that provide care to patients with SARS-CoV-2 infection in Lima, Peru. Daily supplementation with 600 mg of enteral bLF versus placebo for 90 days was compared. Participants were weekly screened for symptoms suggestive of SARS-CoV-2 infection and molecular testing was performed on suspected episodes. A serological test was obtained from all participants at the end of the intervention. The main outcome included symptomatic and asymptomatic cases. A sub-analysis explored the time to symptomatic infection. Secondary outcomes were the severity, frequency, and duration of symptomatic infection. The study was prematurely cancelled due to the availability of vaccines against SARS-CoV-2 in Peru. 209 participants were enrolled and randomized, 104 received bLF and 105 placebo. SARS-CoV-2 infection occurred in 11 (10.6%) participants assigned to bLF and in 9 (8.6%) participants assigned to placebo without significant differences (Incidence Rate Ratio = 1.23, 95%CI 0.51–3.06, p-value = 0.64). There was no significant effect of bLF on time to symptomatic infection (Hazard Ratio = 1.61, 95%CI 0.62–4.19, p-value = 0.3). There were no significant differences in secondary outcomes. A significant effect of bLF in preventing SARS-CoV-2 infection was not proven. Further studies are needed to assess the effect of bLF supplementation on SARS-CoV-2 infection.
Clinical trial registration ClinicalTrials.gov Identifier: NCT04526821, https://clinicaltrials.gov/ct2/show/NCT04526821?term=LACTOFERRIN&cond=COVID-19&cntry=PE&city=Lima&draw=2&rank=1.
Similar content being viewed by others
Introduction
The current pandemic by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has led to more than 200 million COVID-19 cases and around 4.3 million deaths worldwide until August 14th, 2021 (COVID-19 Map—Johns Hopkins Coronavirus Resource Center 2021). Despite the current availability of some vaccines, access to vaccines is limited, especially in low and middle-income countries and the long-term immunity is not completely understood (Figueroa et al. 2021); therefore, interventions are needed to prevent COVID-19. Health care workers are at higher risk of developing COVID-19 and transmitting it to their households (Shah et al. 2020). Therefore, it is fundamental to develop interventions to prevent COVID-19 in this key population.
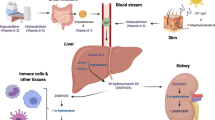
Lactoferrin (LF) is an iron-binding protein found in most mammal’s exocrine secretions. LF has several mechanisms to protect against viral infections; it improves the immune system by activating Natural Killer cells and promotes Interferon production (Legrand 2016). LF has demonstrated in vitro activity against enveloped and non-enveloped viruses preventing their entry to target human cells by binding to heparan sulfate receptors or by interacting with other viral particles during the early stages of infection (Berlutti et al. 2006; Beljaars et al. 2004; Drobni et al. 2004; Marchetti et al. 2004; Superti et al. 2001; Ishikawa et al. 2013; Di Biase et al. 2003). Some clinical studies have described positive effects of LF against upper respiratory tract infections such as a decrease in the incidence of upper respiratory tract infections and a decrease in the incidence and the duration of symptoms of common colds (Chen et al. 2016; Oda et al. 2020; Vitetta et al.2013).
Regarding SARS-CoV-2 infection, in vitro studies suggest that LF can be beneficial by inhibiting the fusion of spike proteins with the angiotensin-converting enzyme 2 (Lang et al. 2011). Furthermore, the uncontrolled inflammatory response of some COVID-19 patients alters iron homeostasis and leads to poor prognosis, which could be improved by the iron-binding properties of LF. Preliminary studies in humans describe a 150-fold increase in LF production among COVID-19 patients compared to non-infected controls, which suggests that LF might play an important role in the immune response against SARS-CoV-2 (Reghunathan et al. 2005). A prospective observational study in Spain reported a decrease in COVID-19 symptoms after supplementation with liposomal LF; however, there was no control group in this study (Serrano et al. 2020).
The evidence of in vitro and observational studies is encouraging; however, no results from randomized, placebo-controlled clinical trials have been reported (Chang et al. 2020). The present trial (LF-COVID) aims to determine the effect of bovine LF (bLF) in the prevention of symptomatic or asymptomatic SARS-CoV-2 infection in hospital workers from two tertiary health care centers providing care to SARS-CoV-2 infected patients in Lima, Peru.
Methods
Study design and ethical approval
This study was a randomized, double-blind, placebo-controlled trial in two general/tertiary hospitals [Hospital Nacional Cayetano Heredia (HCH) and Hospital Nacional Arzobispo Loayza (HNAL)] that provide care to COVID-19 patients in Lima Peru. The study was approved by the ethics committee of Universidad Peruana Cayetano Heredia, by each hospital, and by the Peruvian regulatory institutions. Written informed consent was obtained from all patients. The protocol is available online (ClinicalTrials.gov: NCT04526821).
Participants
Eligible participants were hospital workers > 18 years old without self-reported symptoms suggestive of SARS-CoV-2 infection (cough, fever, dyspnea, rhinorrhea) at enrollment. Exclusion criteria were a self-reported previous diagnosis of SARS-CoV-2 infection (defined as a positive RT-PCR alone or a positive antibody test with presence of suggestive symptoms of SARS-CoV-2 infection), untreated arterial hypertension or type 2 diabetes mellitus, BMI > 35, corticosteroids or immunosuppressors chronic treatment, participating in another clinical trial, a personal history of allergy to cow’s milk protein and a positive IgM, IgG, or RT-PCR for SARS-CoV2 at enrolment. The use of any other supplement to prevent SARS-CoV-2 infection, including ivermectin or chlorine dioxide, was not permitted. Study recruitment was conducted from October 2020 to February 2021. At the beginning of the study, there were no vaccines for SARS-CoV-2 available in Peru.
Randomization and masking
Participants were randomly assigned to bLF or placebo (1:1) after serological and molecular screening tests (both tests had to be negative). The randomization list was performed in random blocks of 4 by an independent statistician (not the researchers). There were 6 randomization groups stratified by the 2 participating hospitals and 3 professions groups (doctors, nursing staff, and technical nursing staff). Obstetricians were included in the pool of nursing staff and biologists, medical technologists, and cleaning and security staff were included in the technical nursing staff group due to similar exposure to SARS-CoV-2.
Bovine lactoferrin or placebo chewable tablets had the same color, size, and taste and were delivered to the participants in identical pouches for masking, according to the sequential order of the randomization list. An independent pharmacist did the treatment assignment; clinical, research, statistician staff, and participants were blinded until the end of the study analysis.
Procedures and interventions
We compared twice-daily supplementation with bLF versus placebo (maltodextrin), both were provided by Morinaga Milk Industry Co from Japan. For 90 days enteral bLF or placebo 600 mg/day was self-administered, participants chewed three 100 mg chewable tablets before breakfast and 3 after dinner and the residues were swallowed with water. The dose of 600 mg/day of lactoferrin was chosen based on previous studies that used between 400 and 600 mg/day of bLF for prevention of respiratory infections (Oda et al. 2020; Vitetta et al. 2013). Doses of bLF between 200 mg/day to 1.5 g/day have been previously used without describing any severe side-effect (Berthon et al. 2022). The LF chewable tablets were of 250 mg and composed of 100 mg of bLF and other ingredients (reduced maltose, dietary fiber—indigestible dextrin, maltodextrin and rapeseed hydrogenated oil) (Online Appendix 1). Pouches of 90 chewable tablets were delivered every 15 days in the follow-up visits. During these visits, evaluation of SARS-CoV-2 suggestive symptoms (fever, fatigue, nonproductive cough, anorexia, myalgia, dyspnea, productive cough, taste and smell disorders, headache, rhinorrhea, nausea, diarrhea, and abdominal pain), data about exposure to SARS-CoV-2, and compliance data were collected. The symptomatic SARS-CoV-2 infection surveillance was also assessed by weekly evaluation of SARS-CoV-2 suggestive symptoms through phone calls. When participants reported symptoms, they were evaluated by two medical doctors simultaneously. They classified the symptomatic episode as suggestive of SARS-CoV-2 infection or not (defined by the Infectious Diseases Society of America Guidelines on the Diagnosis of COVID-19) (Hanson et al. 2020) and decided whether the episode required a RT-PCR for confirmation. Participants with any symptom suggestive of SARS-CoV-2 infection considered as a close contact of a COVID-19 positive patient in the previous 2 weeks also underwent RT-PCR. We followed up the participants with positive RT-PCR every 3 days until all the symptoms have completely disappeared for 3 consecutive days. During this follow-up, the start and end date of the symptoms was recorded by the clinical staff. Asymptomatic SARS-CoV-2 infection was assessed by an antibody test performed at the end of the intervention (day 90) in patients who did not have a positive RT-PCR during follow-up.
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at Cayetano Heredia University (Harris et al. 2009; 2019). Virological and serological testing was done at the Instituto de Medicina Tropical “Alexander Von Humboldt” using quantitative real-time RT-PCR and chemiluminescence IgM/IgG antibodies test (BioMérieux, Marcy-l’Etoile, France).
Outcomes
SARS-CoV-2 infection was the primary composite outcome, which consisted of either (1) symptomatic SARS-CoV-2 infection confirmed by RT-PCR at the time of symptoms or (2) asymptomatic SARS-CoV-2 infection, defined as having a positive antibody (IgM and/or IgG) test at the end of the study without having symptoms during the follow-up period. A sub-analysis was conducted to analyze the time to symptomatic SARS-CoV-2 infection. The secondary outcomes were (1) severity of SARS-CoV-2 infection defined as asymptomatic, mild, moderate, or severe as categorized by the WHO (2021); (2) presence of symptoms of SARS-CoV-2 infection; and (3) duration of the symptoms in confirmed SARS-CoV-2 infections. All secondary outcomes were collected by participants’ follow-up every 3 days until symptoms resolved for 3 consecutive days.
Sample size and statistical methods
Assuming 20% confirmed SARS-CoV-2 infections in the placebo groups, based on international reports, and a 5% attrition rate, 168 participants were needed in each group to detect a 55% decrease in the COVID-19 cases (alpha = 0.05; power = 0.80). The study was interrupted on February 10th 2021 due to the arrival and distribution of the COVID-19 vaccine to hospital workers in Peru when we had 209 patients enrolled.
Treatment groups were compared concerning the baseline demographic information of the participants using Fisher’s exact with a significance level of 0.05. We did all analyses on an intention-to-treat (ITT) basis with no correction for multiplicity for prespecified secondary outcomes. Thus, caution is recommended with secondary outcomes that were reported as point estimates and 95% Confidence Interval (95%CI). To assure randomization balance to obtain an unbiased estimate of the causal effect of the treatment, double-robust (DR) estimation was performed by using Inverse Probability of Treatment Weighting (IPTW). IPTW generates a single pseudo-population in which the balance of pre-treatment covariates is similarly based on the construction of Propensity Scores (PS).
PS were generated using logistic regression modelling based on age, sex, comorbidity, BMI, smoker, hospital, profession, working in another place, principal work area, hours working, hours working in COVID-19 areas, and transportation covariates. IPTW was calculated by the inverse of the PS of receiving the treatment that a patient indeed received.
DR-Poisson regression with robust standard errors was used to calculate Incidence Rate Ratios (IRR) of SARS-CoV-2 infection at the end of the study. In addition, a Kaplan–Meier cumulative incidence curve was used to describe the incidence of symptomatic SARS-CoV-2 infection over time (90-day period) and compared between the two treatment groups with the stratified log-rank test. A DR-Cox proportional-hazards model was used to estimate the hazard ratio (HR) (for bLF versus placebo) and 95% CI. In this analysis, data on patients who survived (no SARS-CoV-2 infection) the entire follow-up period were censored at the last follow-up date or day 100, whichever occurred first. For secondary endpoints, we use the Fisher exact test for categorical variables (severity of episode and frequency of symptoms) and the Wilcoxon test for continuous (skewed) variables (duration of episode and symptoms). All analyses were performed with the use of R v.4.0.1 [R: A language and environment for statistical computing, R Core Team, R Foundation for Statistical Computing, Vienna, Austria (2021) http://www.R-project.org/].
Results
Participants
Of 764 hospital workers invited to participate, 209 (27%) were enrolled and randomized, 104 allocated to receive bLF, and 105 allocated to receive placebo (Fig. 1). The median age was 37 (IQR 31–50); 158 (75.6%) were females. Sixty-four (31%) were doctors, 75 (36%) nurses or obstetricians, and 70 (33%) other professions. There were 111 hospital workers (53%) from HCH and 98 (47%) HNAL. Most baseline characteristics were comparable between the groups (Table 1), but there was a significant difference between both groups in the distribution of sex and hospital work area. The median of total days in observation was 63 days (IQR 31–86). Treatment compliance median was the same in both groups (93%) (Table 2).
Primary outcome
During the 90 days of intervention, 109 patients reported symptoms (62 in the bLF group vs 47 in the placebo group). In 45 of them, COVID-19 was suspected (26 in the bLF group vs 19 in the placebo group). Among the 45 COVID-19 suspected cases, 18 had a positive RT-PCR test for COVID-19 (11 in the bLF group vs 7 in the placebo group) and symptomatic SARS-CoV-2 infection was confirmed. Follow-up characteristics were comparable between the groups (Table 2).
Overall, there were 20 SARS-CoV-2 infections confirmed (18 were symptomatic infections and 2 asymptomatic). The primary composite outcome occurred in 11 (10.6%) participants in the bLF group and 9 (8.6%) participants in the placebo group. There was no significant effect of bLF on the primary composite outcome, Incidence Rate Ratio (IRR) 1.23 (95%CI 0.51–3.06, p-value = 0.64). A Kaplan–Meier cumulative incidence curve for symptomatic SARS-CoV-2 infection comparing bLF and placebo is shown in Fig. 2. There was no significant effect of bLF on time to symptomatic SARS-CoV-2 infections, Hazard Ratio (HR) 1.61 (95%CI 0.62–4.19, p-value = 0.3).
Time to event of symptomatic SARS-CoV-2 infection by treatment group. Red line: lactoferrin; grey line: placebo; red shadow: lactoferrin 95% confidence interval; grey shadow: placebo 95% confidence intervals. *Symptomatic SARS-CoV-2 infection were those that tested positive on reverse-transcriptase–polymerase-chain-reaction (RT-PCR)
Secondary outcomes
There were no significant differences in secondary outcomes (severity of SARS-CoV-2 infection, presence, and duration of symptoms). Regarding the severity of SARS-CoV-2 infection, in the placebo group, 2 (22.2%) participants had an asymptomatic SARS-CoV-2 infection and in 7 (77.8%) the symptomatic episode was categorized as mild. In the bLF group, all 11 confirmed SARS-CoV-2 infections were symptomatic and categorized as mild. There were no moderate or severe SARS-CoV-2 infections. There was no difference between the severity of SARS-CoV-2 infection between groups (p-value = 0.369).
Duration and prevalence of secondary outcomes are shown in Table 3. The most common symptoms among the 18 symptomatic SARS-CoV-2 infections were: cough in 11 participants (61%), nasal secretion in 10 (56%), headache in 8 (44%), and sore throat in 8 (44%). The proportion of patients who developed fever during the study period and the duration of fever were slightly lower t in bLF than in the placebo group, but not significant different (Table 3).
Regarding the duration of the SARS-CoV-2 symptomatic infections, there was no evidence of a difference between the bLF group (median days = 13, IQR 9.5–18.5) and the placebo group (median days = 10, IQR 6.5–13; p-value = 0.146).
We have followed closely all symptoms developed during the intervention. The numbers of subjects with adverse events were 49 in the bLF group and 32 in the placebo group. We found no differences among treatment groups (Table 4). None had a causal relationship with the intervention.
Discussion
This clinical trial was not able to demonstrate a protective effect of bLF supplementation against SARS-CoV-2 infection. Despite the small sample size, bLF was noticed as safe and well-tolerated.
In this study, bLF did not have an effect on COVID-19 incidence. Some previous studies have described the protective effects of LF against other viral infections. Among 260 infants aged 4–6 months LF decreased the incidence of upper respiratory (Chen et al. 2016) infections and in one study the combination of LF and milk serum protein with immunoglobulins decreased the incidence of common colds (Vitetta et al. 2013). Despite the evidence of a protective effect of bLF on other viral respiratory tract infections and the in vitro evidence of the inhibitory effect of LF on SARS-CoV-2 entry to target cells, this study failed to demonstrate a protective effect of LF against SARS-CoV-2 infection. This may be due to differences in the mechanism of action of bLF from the in vitro studies to the in vivo settings, however, the small sample size of this study limits the conclusions of the effect of bLF on SARS-CoV-2 infection.
Regarding the severity of SARS-CoV-2 infection, there were no severe infections and bLF did not have an effect on the severity of SARS-CoV-2 infections. At the study start, only people aged < 60 years, with a BMI < 30 and who did not have any uncompensated medical conditions (such as coronary heart disease, high blood tension and diabetes) were allowed to work at the hospital, thus were the only included in this study. This could limit the generalizability of our findings to the general population, since considering that these populations are less likely to develop severe COVID-19 disease, further studies should aim to include participants at higher risk of worse outcomes.
Furthermore, regarding the presence and duration of symptoms, LF decreased the duration of symptoms of cold in a clinical trial of 310 healthy adults in Japan at a dose of 600 mg/day LF (Oda et al. 2020). This study failed to demonstrate an effect of bLF supplementation on the presence and duration of symptoms. However, the sample size was not calculated for these secondary outcomes and further studies should aim to understand the effect of LF on the actual infection rather than as a preventive measure.
This study should be interpreted in light of its limitations. First, the early stop of the trial decreased the study sample size limiting its power; therefore, this study cannot provide definite evidence. Second, one in-vitro study reported that some bacteria present in the upper gastrointestinal tract have proteases that can degrade LF (Alugupalli and Kalfas 1996). This can limit the assumption of a systemic effect of bLF supplementation on COVID-19 prevention, which was the research question for this study. However, even when degradated, the active metabolits of bLF have antimicrobial properties which can be part of the mechanism of action against SARS-CoV-2 infection (Lizzi et al. 2016). It is essential that further studies, exploring the effect of bLF on SARS-CoV-2 infection assess the pharmacodynamics and pharmacokinetics of chewable tablets bLF supplementation and its metabolites to understand the possible action that this supplement may have on SARS-CoV-2 infection. Third, misclassification bias is possible because of the definition of suspected COVID-19 symptomatic cases and the criteria used for RT-PCR testing. However, since the physicians were blinded to the intervention arm and used a standardized criteria for diganosis, this could have possibly led to non-differential misclassification. Also, the fact that the same two physicians evaluated all participants simultaneously can reduce misclassification bias in this study.Fourth, compliance to treatment was self-reported, which could lead to measurement bias and could be a major unmeasured confounder since this could be affected by recall and acceptability bias (since participants may overestimate their compliance to the intervention). However, it improves the pragmaticism of the treatment effect. Fuerthermore, there were some differences in the baseline characteristics (sex and hospital working area), which could have arisen given the small sample size, but these differences could have also influenced the results. Finally, this study did not explore the effect of bLF supplementation in the inflammatory and immune response to SARS-CoV-2 infection, but only focused on its main outcomes (incidence of SARS-CoV-2 infection, presence and duration of symptoms). Future studies should aim to understand if the supplementation of bLF could have regulatory properties in the immune response against SARS-CoV-2 infection.
To our knowledge, this is the first clinical trial that explored the effects of bLF on SARS-CoV-2 infection. This trial was not able to show significant effects of bLF on SARS-CoV-2 infection incidence, severity and symptoms. Further studies with a larger sample size should be conducted to reach valid conclusions.
References
Alugupalli KR, Kalfas S (1996) Degradation of lactoferrin by periodontitis-associated bacteria. FEMS Microbiol Lett 145(2):209–214. https://doi.org/10.1111/j.1574-6968.1996.tb08579.x
Beljaars L, Van Der Strate BWA, Bakker HI, Reker-Smit C, Van Loenen-Weemaes AM, Wiegmans FC et al (2004) Inhibition of cytomegalovirus infection by lactoferrin in vitro and in vivo. Antivir Res 63(3):197–208
Berlutti F, Schippa S, Morea C, Sarli S, Perfetto B, Donnarumma G et al (2006) Lactoferrin downregulates pro-inflammatory cytokines upexpressed in intestinal epithelial cells infected with invasive or noninvasive Escherichia coli strains. Biochem Cell Biol 84:351–7
Berthon BS, Williams LM, Williams EJ, Wood LG (2022) Effect of lactoferrin supplementation on inflammation, immune function, and prevention of respiratory tract infections in humans: a systematic review and meta-analysis. Adv Nutr. https://doi.org/10.1093/advances/nmac047
Chang R, Ng TB, Sun WZ (2020) Lactoferrin as potential preventative and adjunct treatment for COVID-19. Int J Antimicrob Agents 56(3):106118
Chen K, Chai L, Li H, Zhang Y, Xie HM, Shang J et al (2016) Effect of bovine lactoferrin from iron-fortified formulas on diarrhea and respiratory tract infections of weaned infants in a randomized controlled trial. Nutrition 32(2):222–227
COVID-19 Map—Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Accessed 2 May 2021
Di Biase AM, Pietrantoni A, Tinari A, Siciliano R, Valenti P, Antonini G et al (2003) Heparin-interacting sites of bovine lactoferrin are involved in anti-adenovirus activity. J Med Virol 69(4):495–502
Drobni P, Näslund J, Evander M (2004) Lactoferrin inhibits human papillomavirus binding and uptake in vitro. Antivir Res 64(1):63–68
Figueroa JP, Bottazzi ME, Hotez P, Batista C, Ergonul O, Gilbert S et al (2021) Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet 397:562–564
Hanson KE, Caliendo AM, Arias CA, Englund JA, Lee MJ, Loeb M et al (2020) Infectious Diseases Society of America guidelines on the diagnosis of COVID-19. www.idsociety.org/COVID19guidelines/dx. Accessed 29 June 2021
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Ishikawa H, Awano N, Fukui T, Sasaki H, Kyuwa S (2013) The protective effects of lactoferrin against murine norovirus infection through inhibition of both viral attachment and replication. Biochem Biophys Res Commun 434(4):791–796
Lang J, Yang N, Deng J, Liu K, Yang P, Zhang G et al (2011) Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLoS ONE 6(8):23710
Legrand D (2016) Overview of lactoferrin as a natural immune modulator. J Pediatr 173:S10–S15
Lizzi AR, Carnicelli V, Clarkson MM et al (2016) Bovine lactoferrin and its tryptic peptides: antibacterial activity against different species. Appl Biochem Microbiol 52:435–440. https://doi.org/10.1134/S0003683816040116
Marchetti M, Trybala E, Superti F, Johansson M, Bergström T (2004) Inhibition of herpes simplex virus infection by lactoferrin is dependent on interference with the virus binding to glycosaminoglycans. Virology 318(1):405–413
Oda H, Wakabayashi H, Tanaka M, Yamauchi K, Sugita C, Yoshida H et al (2020) Effects of lactoferrin on infectious diseases in Japanese summer: a randomized, double-blinded, placebo-controlled trial. J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2020.02.010
Reghunathan R, Jayapal M, Hsu LY, Chng HH, Tai D, Leung BP et al (2005) Expression profile of immune response genes in patients with severe acute respiratory syndrome. BMC Immunol 6(1):1–11
Serrano G, Kochergina I, Albors A, Diaz E, Oroval M, Hueso G et al (2020) Liposomal lactoferrin as potential preventative and cure for COVID-19. Int J Res Health Sci 8(1):08–15
Shah ASV, Wood R, Gribben C, Caldwell D, Bishop J, Weir A et al (2020) Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study. BMJ. https://doi.org/10.1136/bmj.m3582
Superti F, Siciliano R, Rega B, Giansanti F, Valenti P, Antonini G (2001) Involvement of bovine lactoferrin metal saturation, sialic acid and protein fragments in the inhibition of rotavirus infection. Biochim Biophys Acta 1528(2–3):107–115
Vitetta L, Coulson S, Beck SL, Gramotnev H, Du S, Lewis S (2013) The clinical efficacy of a bovine lactoferrin/whey protein Ig-rich fraction (Lf/IgF) for the common cold: a double blind randomized study. Complement Ther Med 21(3):164–171
World Health Organization (WHO) (2021) COVID-19 clinical management: living guidance. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1. Accessed 16 May 2021
Funding
This work was supported by Morinaga Milk Company, Japan; Morinaga Foundation For Health and Nutrition. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Navarro, R., Paredes, J.L., Tucto, L. et al. Bovine lactoferrin for the prevention of COVID-19 infection in health care personnel: a double-blinded randomized clinical trial (LF-COVID). Biometals 36, 463–472 (2023). https://doi.org/10.1007/s10534-022-00477-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10534-022-00477-3