Abstract
Aims/hypothesis
To investigate clinical and sociodemographic predictors of birthweight in singletons born to women with type 1 or type 2 diabetes.
Methods
Normally formed singleton live births and intrapartum stillbirths, born to women with pre-conception diabetes during 1996–2008, were identified from the population-based Northern Diabetes in Pregnancy Survey (n = 1,505). Associations between potential predictors and birthweight were analysed by multiple regression.
Results
Potentially modifiable independent predictors of increase in birthweight were pre-pregnancy care (adjusted regression coefficient [b] = 87.1 g; 95% CI 12.9, 161.3), increasing third-trimester HbA1c ≤7% (53 mmol/mol) (b = 310.5 g per 1% [11 mmol/mol]; 95% CI 246.3, 374.7) and increasing maternal BMI (b = 9.5 g per 1 kg/m2; 95% CI 3.5, 15.5). Smoking during pregnancy (b = −145.1 g; 95% CI −231.4, −58.8), later gestation at first antenatal visit (b = −15.0 g; 95% CI −26.9, −3.0) and higher peri-conception HbA1c (b = −48.2 g; 95% CI −68.8, −27.6) were independently associated with birthweight reduction. Pre-pregnancy nephropathy (b = −282.7 g; 95% CI −461.8, −103.6) and retinopathy (b = −175.5 g; 95% CI −269.9, −81.0) were independent non-modifiable predictors of reduced birthweight, while greater maternal height was a non-modifiable predictor of increasing birthweight (b = 17.8 g; 95% CI 12.3, 23.2). Other predictors of birthweight increase were male sex, multiparity and increasing gestational age at delivery. Type or duration of diabetes, socioeconomic status and ethnicity were not associated with continuous birthweight.
Conclusions/interpretation
Poor glycaemic control before and throughout pregnancy is associated with abnormal fetal growth, with increasing peri-conception HbA1c predicting weight reduction and increasing third-trimester HbA1c predicting increased birthweight. Women with microvascular complications of diabetes may require increased surveillance to detect fetal growth restriction.
Similar content being viewed by others
Introduction
Women with type 1 and type 2 diabetes have a much higher risk of serious adverse pregnancy outcomes, such as stillbirth, major congenital anomalies, neonatal morbidity and mortality [1–4]. Maternal diabetes is also associated with a higher risk of aberrant fetal growth. About 50% of infants born to mothers with pre-conception diabetes are reported to be macrosomic or large for gestational age (LGA), although there is overlap in the definition of both of these terms (usually defined as birthweight >90th centile for gestational age) [5–8]. Small for gestational age (SGA) is less often associated with maternal diabetes per se, but has been reported in association with severe vascular complications [9, 10] and can result in higher neonatal morbidity and mortality. Both birthweight extremes in offspring of mothers with diabetes are associated with a higher risk of complications during the pregnancy, labour and neonatal period [2, 11] as well as with a potential increase in diseases in childhood and adulthood, including obesity, cardiovascular disease, diabetes and metabolic syndrome [12–15].
The increased risk of an LGA birth in women with diabetes is thought to be associated with poor glycaemic control, usually estimated by concentration of HbA1c before or during pregnancy [5, 11, 16, 17]. However, the evidence and the direction of the association, particularly in relation to pre- and post-conception glycaemic control, is inconsistent. Penney et al, for example, found a negative association between pre-conception HbA1c and standardised birthweight, but no associations at any trimester of pregnancy [16]. In contrast, Evers et al reported a positive association between risk of macrosomia and third-trimester HbA1c [5].
Less is known about the association between gestational glycaemic control and the risk of an SGA birth, and which windows of exposure are most important for increased risk of abnormal birthweight. Moreover, the extent to which other potential determinants of birthweight may modify the effect of glycaemia on fetal growth in women with diabetes has not been extensively investigated in population-based studies.
The aim of this study was to investigate the influence of sociodemographic and clinical factors, including peri-conception and antenatal HbA1c, on birthweight in normally formed singleton infants born to women with type 1 and type 2 diabetes, using the population-based Northern Diabetes in Pregnancy Survey (NorDIP).
Methods
Study population
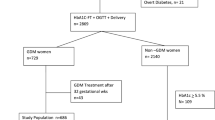
The North of England (UK) is a geographically distinct area with a population of around 3 million and 31,000 births per year. NorDIP collects details of all known pregnancies occurring in the region, irrespective of outcome, in women diagnosed with diabetes at least 6 months before the index pregnancy [18]. All maternity units within the region participate in the survey. Coordinators in each unit notify the survey of relevant pregnancies, and data collection is undertaken by unit clinicians. Pregnancies in women with gestational diabetes (i.e. hyperglycaemia first diagnosed during pregnancy) are not included. Various demographic and clinical variables are collected, including pre-conception and antenatal HbA1c (DCCT aligned since 2000).
This analysis included all normally formed singleton live births and intrapartum stillbirths born in the region between 01 January 1996 and 31 December 2008. Pregnancies resulting in antepartum stillbirth (n = 38), identified from the Northern Perinatal Morbidity and Mortality Survey (PMMS) [19], and/or complicated by major congenital anomaly (n = 129), identified from the Northern Congenital Abnormality Survey (NorCAS) [20], were excluded due to the known predominance of growth-retarded fetuses in these groups. All three databases are linked into a coordinated database in the Regional Maternity Survey Office (RMSO) (www.rmso.org.uk). The total number of registered singleton live and stillbirths for the North of England was obtained from the UK Office for National Statistics.
Definitions and statistical analysis
All NorDIP clinical and sociodemographic variables with a hypothesised influence on birthweight were examined: diabetes type, fetal sex, pre-pregnancy folate supplement usage, pre-pregnancy care, smoking during pregnancy, history of clinically diagnosed pre-pregnancy nephropathy, neuropathy or retinopathy, parity (primiparous vs multiparous) and maternal ethnicity (white vs non-white) were analysed as dichotomous variables. Macrosomia was defined as a birthweight of ≥4,000 g and low birthweight was defined as a birthweight of <2,500 g. Socioeconomic status was estimated from the Index of Multiple Deprivation (a UK area-based measure, derived from a mother’s residential postcode at delivery) and analysed in tertiles of rank [21]. Duration of diabetes, maternal age at delivery, maternal BMI at first antenatal visit, maternal height, gestational age at first antenatal visit and at delivery (based on reported estimated date of delivery calculated for the majority of women using ultrasound scan at 10–13 weeks’ gestation, or date of the last menstrual period [LMP], if no scan dating was available) and mean maternal HbA1c at three time points (peri-conception, second trimester and third trimester) were analysed as continuous variables. Peri-conception HbA1c was calculated as the closest measurement within 3 months before the date of the LMP (available for 49.5% of pregnancies) or mean first-trimester measurement (up to 14 weeks gestation) (valid 83.3%) for women with no pre-conception measure recorded. Peri-conception HbA1c (valid 86.7%) was chosen as a reasonable surrogate of pre-conception HbA1c, as first-trimester HbA1c was highly correlated with pre-conception HbA1c (Spearman correlation coefficient 0.75). The independent effects of pre-conception HbA1c and first-trimester HbA1c were, nevertheless, also examined in a sensitivity analysis on a subsample of participants with both measures.
The association between each variable and birthweight, as a continuous variable, was examined by multiple linear regression. The summary influence of each variable was estimated by constructing a series of simple models that included the variable of interest, alongside sex, parity and gestational age. The independent influence of each variable was estimated in a fully adjusted model, constructed using a backwards stepwise approach. Gestational age (centred to reduce collinearity) was modelled as a three-term polynomial, i.e. b 1 (gestational age − x̄) + b 2 (gestational age − x̄)2 + b 3 (gestational age − x̄)3 (see electronic supplementary material [ESM] Fig. 1). The shape of the association between each HbA1c variable and birthweight was explored by locally weighted scatterplot smoothing (LOWESS) and fitting fractional polynomials. As a nonlinear association between third-trimester HbA1c and birthweight was observed, it was modelled by piecewise linear regression, with a single knot at 7% (53 mmol/mol) (the choice of location being guided by LOWESS explorations), which divided the regression into two parts, ≤7% (53 mmol/mol) (61.7% of participants) and >7% (53 mmol/mol, 38.3%). The presence of heteroscedasticity was evaluated using the Cook–Weisberg test [22] and, when present, the Huber/White estimator [23] was used (further details in ESM Methods). The proportion of variation directly explained by each variable was estimated from the change in the coefficient of determination (ΔR 2) resulting from removing that variable from the adjusted model.
Separate analyses were performed to examine predictors of LGA and SGA births; LGA (birthweight ≥90th percentile) and SGA (<10th percentile) categories were created based on birthweight standardised for fetal sex, parity and gestational age using Scottish birth population standards [24]. ORs and associated 95% CIs for LGA and SGA were estimated for various predictors using multiple logistic regression; adjusted effects were estimated using a backwards stepwise approach. The probability of LGA for specific values of third-trimester HbA1c was estimated by taking marginal values of the adjusted model; corresponding 95% CIs were obtained using the delta method.
Potential interactions between the HbA1c variables and all other variables in each adjusted model were examined by the inclusion of cross-product terms.
SPSS for Windows 17.0 (IBM Corporation, NY, USA) was used for most of the statistical analyses. Confidence intervals for ΔR 2 were approximated by bootstrapping on 10,000 repeated samples, drawn with replacement, using Stata 11.1 (Statacorp, College Station, TX, USA). p < 0.05 was considered statistically significant.
Ethics approval and research governance
Newcastle Research Ethics Committee originally granted approval for NorDIP in 1993, and data are now obtained and held with informed consent.
Results
Of 389,789 singleton pregnancies resulting in non-malformed stillbirths and live births recorded during 1996–2008, 1,502 were singleton live births and three were intrapartum stillbirths in women with type 1 and type 2 diabetes; 1,495 of these were used for this analysis (10 cases had missing birthweight data).
Descriptive statistics for the study sample are shown in Tables 1 and 2. The median birthweight for offspring of women with diabetes was 3,450 g (interquartile range [IQR] = 2,990–3,918), and the median gestational age was 37.0 weeks (IQR = 36–38). The proportion of macrosomia was significantly higher in offspring of women with diabetes compared with the North of England background population (22.4% vs 12.1%, RR 1.9, 95% CI 1.7, 2.0) as was the proportion of low birthweight (10.7 vs 5.8%, RR 1.8, 95% CI 1.6, 2.1) (not shown in Tables 1 and 2). There were 50.4% LGA babies born to women with type 1 diabetes compared with 43.7% (p = 0.04) to women with type 2 diabetes (22% in our population).
Table 3 shows that increasing peri-conception HbA1c (p < 0.0001), later gestation at first antenatal visit (p = 0.01), increasing maternal age (p = 0.0001), pre-pregnancy retinopathy (p = 0.0003), pre-pregnancy nephropathy (p = 0.002) and smoking during pregnancy (p = 0.001) were all independently associated with lower birthweight. Conversely, increasing third-trimester HbA1c for values ≤7% (53 mmol/mol) (p < 0.0001), increasing maternal BMI (p = 0.002), pre-pregnancy care (p = 0.02), increasing maternal height (p < 0.0001), male sex (p = 0.0007) and multiparity (p < 0.0001) were independently associated with higher birthweight. Type or duration of diabetes, non-white ethnicity, pre-pregnancy neuropathy, second trimester HbA1c, third-trimester HbA1c for values >7% (53 mmol/mol), and area-based deprivation were not associated with birthweight after adjustment for other test variables.
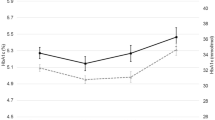
The model explained 46.9% (95% CI 40.5, 51.4) of the variation in birthweight. Third-trimester HbA1c explained 5.6% (95% CI 3.7, 7.8) of the variation, six times the contribution of peri-conception HbA1c (ΔR 2 = 0.9% [95% CI 0.3, 2.0]). The remaining potentially modifiable factors each explained 0.3–0.6% of the variation (Table 3, Fig. 1). The strongest predictor of birthweight was gestational age (as a cubic term), explaining 28.0% (95% CI 23.1, 33.8) of the total variation. Each of other non-modifiable factors (e.g. maternal height and age, parity, pre-pregnancy microvascular complications) explained between 0.2% and 2.4% of the variation in birthweight.
Percentage of variance (with 95% CIs) directly explained by each significant independent predictor of birthweight in the offspring of women with pre-conception diabetes born in the North of England during 1996–2008. White bars represent non-modifiable variables; black bars represent potentially modifiable variables
Two statistically significant interactions were observed for third-trimester HbA1c in the adjusted model of continuous birthweight. First, the effect of third-trimester HbA1c (for values ≤7% [53 mmol/mol]) decreased with increasing peri-conception HbA1c (p = 0.001). Second, the effect of third-trimester HbA1c (≤7% [53 mmol/mol]) increased with increasing BMI (p = 0.002) (furher details in ESM Results 1).
For offspring of women with diabetes, 81.8% were at or above the median weight of the reference population (≥50th percentile), 49.0% were LGA and 3.0% were SGA. Table 4 shows that increasing third-trimester HbA1c for values ≤7% (53 mmol/mol) (p < 0.0001) and increasing maternal height (p < 0.0001) were independently associated with increased odds of LGA, while increasing peri-conception HbA1c (p = 0.002), later gestation at first antenatal visit (p = 0.005), pre-pregnancy retinopathy (p = 0.0004), non-white ethnicity (p = 0.03) and smoking during pregnancy (p = 0.0001) were associated with reduced odds of LGA. Table 5 shows that with the increase in third-trimester HbA1c from 5.5% (36.6 mmol/mol) to 7.0% (53.0 mmol/mol), the modelled LGA rate increased sharply from 27.1% (95% CI 22.0, 32.2) to 64.1% (95% CI 59.1, 69.0), respectively, with negligible increase thereafter.
Later gestation at first antenatal visit (p = 0.01) and pre-pregnancy nephropathy (p = 0.003) were associated with higher odds of an SGA birth, while increasing maternal height (p = 0.01) and increasing third-trimester HbA1c for values ≤7% (53 mmol/mol) (p = 0.03) were associated with lower odds of an SGA birth (Table 4).
A sensitivity analysis found that most of the effect of peri-conception HbA1c on birthweight was attributed to pre-conception HbA1c (ESM Table 1, ESM Results 2).
Discussion
This large population-based cohort study describes the association between clinical and sociodemographic factors and birthweight in normally formed singletons born to women with pre-conception diabetes. The study demonstrates a complex association between glycaemia and birthweight; this relationship changed during pregnancy, such that increasing peri-conception HbA1c was associated with a reduction in birthweight, while increasing third-trimester HbA1c for values ≤7% (53 mmol/mol) was associated with an increase in birthweight. In addition to confirming that known determinants of birthweight in the general population (smoking during pregnancy, maternal height and BMI, parity) also apply to women with diabetes, we identified several additional specific predictors such as HbA1c concentrations and microvascular complications. Among the potentially modifiable predictors of birthweight, peri-conception and third-trimester HbA1c were the most important, while gestational age was the strongest birthweight predictor overall.
This study comprises one of the largest cohorts exploring the association between glycaemia at different stages of pregnancy in women with type 1 or type 2 diabetes and birthweight using data from a population-based survey, NorDIP, and is the only investigation to date to include such a comprehensive range of other clinical and sociodemographic explanatory variables. We also used data from two other linked regional surveys, NorCAS and PMMS, which allowed us to create a complete dataset of normally formed singleton pregnancies in women with diabetes. By excluding pregnancies affected by a major congenital anomaly (over 7% in this population [3]) and antepartum stillbirths, known to be associated with low birthweight, we avoided a potential bias of over-representation of SGA fetuses, which other similar studies might not have.
The birthweight distribution of the North of England birth population, both overall and among women with diabetes, is almost identical to the equivalent distribution in England and Wales [8] (ESM Fig. 2). Our results are therefore generalisable to the national population and are likely to be relevant to similar populations in other industrialised countries.
We analysed birthweight as both a continuous measure and the commonly used and clinically meaningful categorical measures LGA and SGA. Analysing LGA and SGA birthweights exclusively may have increased the risk of type II errors, due to reduced statistical power; however, including these alongside the continuous analyses allows for a more complete comparison with previous literature. As some researchers recommend using customised centiles to identify LGA and SGA births, we performed additional analyses using this approach but, because this further reduced the number of available participants and did not materially alter the results, these data are not shown.
Our measure of glycaemia was limited to HbA1c; this has excellent validity as an estimate of average blood glucose but does not provide information on glycaemic excursions, which may be an important driver for macrosomia [17, 25, 26]. Moreover, we did not have 100% completeness for peri-conception and trimester-specific HbA1c measurements. We used a composite measure of peri-conception HbA1c as a proxy for pre-conception HbA1c, due to the relatively high percentage of participants with missing pre-conception values. This potentially hinders comparisons with previous studies using pre-conception HbA1c. However, our sensitivity analysis found that most of the effect of peri-conception HbA1c on birthweight was attributed to pre-conception HbA1c, suggesting this was a reasonable surrogate measure in our population-based cohort.
We found that about half of births to women with diabetes were LGA, similar to other studies in women with diabetes reporting LGA rates ranging from 45% to 51% for populations of women with both type 1 and type 2 diabetes [7, 8] and from 47% to 62.5% for women with type 1 diabetes [5, 6, 25, 27].
We found a strong independent association between increasing third-trimester HbA1c for values ≤7% (53 mmol/mol) (about 62% of pregnancies) and higher birthweight (and a three-fold increase in LGA risk per 1% [11 mmol/mol] increase in HbA1c), but no significant association with HbA1c >7%. Second-trimester HbA1c, although being strongly correlated with third-trimester HbA1c, was a much weaker predictor of increase in birthweight and lost its effect after adjustment for third-trimester HbA1c. Although earlier studies have not explored the linearity of the association between third-trimester HbA1c and birthweight, there is some consistency in the literature reporting the positive association between third-trimester maternal hyperglycaemia and risk of LGA birthweight in women with pre-gestational and gestational diabetes [5, 28–30]. Evers et al found that of the five variables in their final predictive model (third-trimester HbA1c, absence of third-trimester severe hypoglycaemia, the use of insulin lispro (B28Lys,B29Pro human insulin), weight gain during pregnancy and non-smoking), third-trimester HbA1c (≤7% [53 mmol/mol] for 84% of women) was the most powerful predictor of LGA birthweight in women with type 1 diabetes, explaining 4.7% of the variance [5]. Third-trimester HbA1c was reported to be a significant predictor of LGA birthweight in a cohort of women with type 1, type 2 and gestational diabetes after adjustment for a number of confounders [30]. In a study of pregnancies complicated by gestational diabetes or impaired glucose tolerance, maternal fasting glycaemia during 32–35 weeks was the strongest predictor of accelerated growth in the late third trimester, whereas in the late second and early third trimester and at birth the dominant predictors were previous LGA or maternal obesity [29]. The Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) study reported that mild antenatal maternal hyperglycaemia in women without known diabetes is also associated with an increased risk of LGA [28]. However, a Scottish study did not find a significant correlation between third-trimester HbA1c and birthweight [16] in women with type 1 diabetes but they did not explore this association in a multivariable model. A Danish study reported a significant association between increased third-trimester HbA1c and risk of LGA birthweight in women with type 1 diabetes for women with higher BMI (>23 kg/m2) only [27]. Despite a general agreement that maternal late hyperglycaemia causing fetal hyperinsulinaemia is an important determinant of fetal macrosomia, there is some evidence that the contribution of maternal hyperglycaemia to the variance in LGA birthweight is relatively low, and high rates of LGA birthweight are reported despite apparently good glucose control measured by HbA1c [5, 31, 32]. This may be due to the failure of HbA1c to indicate variability in glycaemia and time spent at high glucose levels, which may be critically associated with fetal overgrowth [5, 17, 26, 33]. The lack of association with third-trimester HbA1c >7% (53 mmol/mol) in our study may also reflect the limitations of using HbA1c to measure hyperglycaemia during pregnancy. Measures of glycaemic variation using newer methods, such as continuous glucose monitoring, may contribute to better understanding of the relationship between hyperglycaemia and fetal macrosomia in the future [32]. In a randomised controlled trial, continuous glucose monitoring during pregnancy was associated with improved HbA1c levels at 32–36 weeks and a reduced rate of LGA births [17]. Daily glucose monitored during the second and third trimesters was a good predictor of birthweight in term pregnancies with type 1 diabetes; only infants of women with overall daily glucose values of ≤5.27 mmol/l had birthweight comparable with the control group [34].
The association between pre-conception blood glucose concentration and birthweight has been less studied, in particular with adjustment for covariates, as in our cohort. A Scottish study of 57 pregnancies of women with diabetes reported an increase in pre-conception and early first-trimester total HbA1c in a group with increased median standardised birthweight compared with the control group, while total HbA1c during later periods of pregnancy did not differ significantly between the groups [35]. A larger (203 singletons), more recent, Scottish study of women with type 1 diabetes reported a significant negative association between pre-pregnancy HbA1c and standardised birthweight, consistent with our findings for peri-conception HbA1c, but found no significant association between HbA1c and birthweight for any trimester of pregnancy [16]. Evers et al did not find an association with first-trimester HbA1c in an unadjusted analysis [5], similar to our unadjusted analysis result for peri-conception HbA1c. This may be explained by the direct association (of lower birthweight for increasing HbA1c) being masked by the indirect association (of higher birthweight for increasing HbA1c) acting through correlation with third-trimester HbA1c. The association between pre-conception and maximal maternal HbA1c during pregnancy and birthweight z-score was described as curvilinear in a recent study by Rackham et al [36]. However, that study involved pregnancies resulting in stillbirths or neonatal deaths only, and the number of cases was small. We found an association between increasing peri-conception HbA1c and reduction in birthweight when adjusted for confounders, in particular for ≤7% (≤53 mmol/mol) third-trimester HbA1c. We also identified a significant interaction between peri-conception and third-trimester HbA1c (≤7%) with the effect of increasing third-trimester HbA1c being greater among women with low peri-conception HbA1c than among women with high peri-conception HbA1c. We speculate that high glucose levels in early pregnancy may harm placental development and thus the capacity for fetal growth, such that the effect of hyperglycaemia in later pregnancy is permanently attenuated. The presence of microvascular disease, in particular in combination with first-trimester hyperglycaemia, can inhibit trophoblast proliferation, thereby reducing placental growth and impairing uteroplacental function, which may result in subsequent intrauterine growth restriction [10, 37]. In our study, microvascular complications (pre-pregnancy retinopathy and/or nephropathy) in women with diabetes were associated with lower birthweight. As there is some evidence that variation in birthweight may be at least partly determined by fetal growth within the first 12 weeks after conception [38], investigation of the association of peri-conception hyperglycaemia with early fetal growth is crucial for understanding the mechanisms of growth restriction or overgrowth in pregnancies of women with diabetes.
In addition to maternal hyperglycaemia, other factors, such as non-smoking, higher maternal height and BMI, found to be associated with higher birthweight in offspring of women with diabetes by previous studies [27, 30], were also independent significant predictors of increased birthweight in our study.
The apparently contradictory association between peri-conception hyperglycaemia and reduced birthweight and between late-pregnancy hyperglycaemia and increased birthweight may be explained by the effects of multiple factors, including maternal diabetes, on fetal growth mechanism during different periods of pregnancy. While in early pregnancy hyperglycaemia may lead to restricted fetal growth via reduction in trophoblast proliferation, later in pregnancy, fetal hyperglycaemia and hyperinsulinaemia lead to increased placental angiogenesis, increased and altered vascular endothelial-like growth factor and chorionic villous branching, which, in turn, lead to placental vascular dysfunction [39]. As a result, infants of mothers with diabetes may have an unhealthy body composition (increased body fat) even if they have appropriate birthweight for gestational age [40]. If hyperglycaemia-related growth in the third trimester is mostly associated with the deposition of adipose tissue, this might partly explain our finding of an increased association between third-trimester HbA1c and birthweight with increasing maternal BMI.
In conclusion, this study found a varying association between maternal blood glucose concentration and birthweight, with increasing peri-conception HbA1c being associated with lower birthweight and increasing third-trimester HbA1c ≤7% (53 mmol/mol) predicting higher birthweight. Peri-conception and third-trimester HbA1c were the two most important potentially modifiable predictors of birthweight, reinforcing the need for careful glucose control, beginning before conception. While glucose control remains a key focus of pre-conception and antenatal care for women with diabetes, other modifiable risk factors for adverse pregnancy outcome also need to be addressed, such as ensuring that women who smoke are supported to quit. Further, awareness of the potential for poor fetal growth, particularly in women with microvascular disease and sometimes co-existing with apparently normal fetal size, emphasises the need for careful antenatal assessment of fetal well-being. Future studies, using more sensitive measures of both glucose control and fetal growth and body composition, should explore critical windows for the effect of maternal blood glucose concentration on birthweight.
Abbreviations
- IQR:
-
Interquartile range
- LGA:
-
Large for gestational age
- LMP:
-
Last menstrual period
- LOWESS:
-
Locally weighted scatterplot smoothing
- NorCAS:
-
Northern Congenital Abnormality Survey
- NorDIP:
-
Northern Diabetes in Pregnancy Survey
- PMMS:
-
Perinatal Morbidity and Mortality Survey
- RMSO:
-
Regional Maternity Survey Office
- SGA:
-
Small for gestational age
References
Macintosh MC, Fleming KM, Bailey JA et al (2006) Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ 333:177–180
Meur S, Mann NP (2007) Infant outcomes following diabetic pregnancies. Paediatr Child Health 17:217–222
Bell R, Glinianaia SV, Tennant PW, Bilous RW, Rankin J (2012) Peri-conception hyperglycaemia and nephropathy are associated with risk of congenital anomaly in women with pre-existing diabetes: a population-based cohort study. Diabetologia 55:936–947
Evers IM, de Valk HW, Visser GH (2004) Risk of complications of pregnancy in women with type 1 diabetes: nationwide prospective study in the Netherlands. BMJ 328:915
Evers IM, de Valk HW, Mol BW, ter Braak EW, Visser GH (2002) Macrosomia despite good glycaemic control in type I diabetic pregnancy; results of a nationwide study in The Netherlands. Diabetologia 45:1484–1489
Persson M, Pasupathy D, Hanson U, Norman M (2011) Birth size distribution in 3,705 infants born to mothers with type 1 diabetes: a population-based study. Diabetes Care 34:1145–1149
Yang J, Cummings EA, O'Connell C, Jangaard K (2006) Fetal and neonatal outcomes of diabetic pregnancies. Obstet Gynecol 108:644–650
Confidential Enquiry into Maternal and Child Health (2005) Pregnancy in women with type 1 and type 2 diabetes in 2002–03, England, Wales and Northern Ireland. CEMACH, London
Reece EA, Leguizamon G, Homko C (1998) Pregnancy performance and outcomes associated with diabetic nephropathy. Am J Perinatol 15:413–421
Vambergue A, Fajardy I (2011) Consequences of gestational and pregestational diabetes on placental function and birth weight. World J Diabetes 2:196–203
Weindling AM (2009) Offspring of diabetic pregnancy: short-term outcomes. Semin Fetal Neonatal Med 14:111–118
Aerts L, van Assche FA (2003) Intra-uterine transmission of disease. Placenta 24:905–911
Boney CM, Verma A, Tucker R, Vohr BR (2005) Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 115:e290–296
Johnson RC, Schoeni RF (2011) Early-life origins of adult disease: national longitudinal population-based study of the United States. Am J Public Health 101:2317–2324
Hermann GM, Dallas LM, Haskell SE, Roghair RD (2010) Neonatal macrosomia is an independent risk factor for adult metabolic syndrome. Neonatology 98:238–244
Penney GC, Mair G, Pearson DW (2003) The relationship between birth weight and maternal glycated haemoglobin (HbA1c) concentration in pregnancies complicated by Type 1 diabetes. Diabet Med 20:162–166
Murphy HR, Rayman G, Lewis K et al (2008) Effectiveness of continuous glucose monitoring in pregnant women with diabetes: randomised clinical trial. BMJ 337:a1680
Bell R, Bailey K, Cresswell T, Hawthorne G, Critchley J, Lewis-Barned N (2008) Trends in prevalence and outcomes of pregnancy in women with pre-existing type I and type II diabetes. BJOG 115:445–452
Regional Maternity Survey Office (2009) In: Bradford C (ed) Regional Maternity Survey Office annual report 2009. RMSO and North East Public Health Observatory, Newcastle upon Tyne
Richmond S, Atkins J (2005) A population-based study of the prenatal diagnosis of congenital malformation over 16 years. BJOG 112:1349–1357
Noble M, McLennan D, Wilkinson K, Whitworth A, Barnes H, Dibben C (2008) The English indices of deprivation 2007. Department for Communities and Local Government, London
Cook RD, Weisberg S (1982) Residuals and influence in regression. Chapman and Hall, London
White H (1982) Maximum likelihood estimation of misspecified models. Econometrica 50:1–25
Bonellie S, Chalmers J, Gray R, Greer I, Jarvis S, Williams C (2008) Centile charts for birthweight for gestational age for Scottish singleton births. BMC Pregnancy Childbirth 8:5
Jensen DM, Damm P, Moelsted-Pedersen L et al (2004) Outcomes in type 1 diabetic pregnancies: a nationwide, population-based study. Diabetes Care 27:2819–2823
Kerssen A, Evers IM, de Valk HW, Visser GHA (2003) Poor glucose control in women with type 1 diabetes mellitus and 'safe' hemoglobin A1c values in the first trimester of pregnancy. J Matern Fetal Neonatal Med 13:309–313
Nielsen GL, Dethlefsen C, Moller M, Sorensen HT (2007) Maternal glycated haemoglobin, pre-gestational weight, pregnancy weight gain and risk of large-for-gestational-age babies: a Danish cohort study of 209 singleton type 1 diabetic pregnancies. Diabet Med 24:384–387
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002
Schaefer-Graf UM, Kjos SL, Kilavuz O et al (2003) Determinants of fetal growth at different periods of pregnancies complicated by gestational diabetes mellitus or impaired glucose tolerance. Diabetes Care 26:193–198
Sojo L, Garcia-Patterson A, Maria MA et al (2010) Are birth weight predictors in diabetic pregnancy the same in boys and girls? Eur J Obstet Gynecol Reprod Biol 153:32–37
Lepercq J, Taupin P, Dubois-Laforgue D et al (2001) Heterogeneity of fetal growth in type 1 diabetic pregnancy. Diabetes Metab 27:339–344
Kerssen A, de Valk HW, Visser GH (2007) Increased second trimester maternal glucose levels are related to extremely large-for-gestational-age infants in women with type 1 diabetes. Diabetes Care 30:1069–1074
Dalfra MG, Sartore G, Di Cianni G et al (2011) Glucose variability in diabetic pregnancy. Diabetes Technol Ther 13:853–859
Mello G, Parretti E, Mecacci F et al (2000) What degree of maternal metabolic control in women with type 1 diabetes is associated with normal body size and proportions in full-term infants? Diabetes Care 23:1494–1498
Gold AE, Reilly R, Little J, Walker JD (1998) The effect of glycemic control in the pre-conception period and early pregnancy on birth weight in women with IDDM. Diabetes Care 21:535–538
Rackham O, Paize F, Weindling AM (2009) Cause of death in infants of women with pregestational diabetes mellitus and the relationship with glycemic control. Postgrad Med 121:26–32
Weiss U, Cervar M, Puerstner P et al (2001) Hyperglycaemia in vitro alters the proliferation and mitochondrial activity of the choriocarcinoma cell lines BeWo, JAR and JEG-3 as models for human first-trimester trophoblast. Diabetologia 44:209–219
Bukowski R, Smith GC, Malone FD et al (2007) Fetal growth in early pregnancy and risk of delivering low birth weight infant: prospective cohort study. BMJ 334:836
Leach L (2011) Placental vascular dysfunction in diabetic pregnancies: intimations of fetal cardiovascular disease? Microcirculation 18:263–269
Catalano PM, Thomas A, Huston-Presley L, Amini SB (2003) Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol 189:1698–1704
Acknowledgements
We are grateful to all the district convenors and coordinators in the North of England for their continued collaboration and support of the NorDIP and NorCAS. We also thank the staff at the RMSO, Newcastle upon Tyne, UK, for their help in data tracing and checking.
Funding
The work was supported by Diabetes UK (BDA number: 10/0004019). NorCAS is funded by the UK Healthcare Quality Improvement Partnership. NorDIP and the PMMS are funded by the four Primary Care Trusts in North East England.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
RB and JR developed the study concept and supervised the research. SVG and PWGT analysed the data, and SVG wrote the first draft of the manuscript. SVG, PWGT, RWB, JR and RB contributed to the interpretation of the results and to the discussion, reviewed the manuscript and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 64 kb)
ESM Results 1
(PDF 31 kb)
ESM Results 2
(PDF 13 kb)
ESM Fig. 1
(PDF 56 kb)
ESM Fig. 2
(PDF 7 kb)
ESM Table
(PDF 40 kb)
Rights and permissions
About this article
Cite this article
Glinianaia, S.V., Tennant, P.W.G., Bilous, R.W. et al. HbA1c and birthweight in women with pre-conception type 1 and type 2 diabetes: a population-based cohort study. Diabetologia 55, 3193–3203 (2012). https://doi.org/10.1007/s00125-012-2721-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2721-z