Abstract
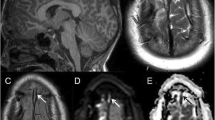
Sturge-Weber syndrome (SWS) is a congenital disorder characterized by a vascular birthmark and neurological abnormalities. Typical imaging findings using MRI or CT are superficial cerebral calcification, atrophy and leptomeningeal enhancement. We present a neonate diagnosed with SWS because of a port-wine stain. In the absence of neurological symptoms the first MRI was performed when he was 4 months old, and follow-up MRI studies were performed after his first seizure at the age of 12 months. MRI was performed using standard sequences before and after administration of IV gadolinium. A high-resolution T2*-weighted, rf-spoiled 3D gradient-echo sequence with first-order flow compensation in all three directions was used for additional venographic imaging [blood-oxygen-level-dependent (BOLD) venography]. The initial conventional MRI sequences did not demonstrate any abnormality, but BOLD venography identified leptomeningeal internal veins. Follow-up MRI after the first onset of seizures demonstrated strong leptomeningeal enhancement, while BOLD venography revealed pathological medullary and subependymal veins as well as deep venous structures. At this time there were the first signs of atrophy and CT showed marginal calcifications. This report demonstrates that high-resolution BOLD MR venography allows early diagnosis of venous anomalies in SWS, making early therapeutic intervention possible.



Similar content being viewed by others
References
Comi AM (2003) Pathophysiology of Sturge-Weber syndrome. J Child Neurol 18:509–516
Yu SM, Chang CP, Liao SQ, et al (2000) Cerebral blood flow and glucose metabolism in an infant with Sturge-Weber syndrome. Clin Nucl Med 25:217–218
Vogl TJ, Stemmler J, Bergmann C, et al (1993) MR and MR angiography of Sturge-Weber syndrome. AJNR 14:417–425
Reichenbach JR, Jonetz-Mentzel L, Fitzek C, et al (2001) High-resolution blood oxygen-level dependent MR venography (HRBV): a new technique. Neuroradiology 43:364–369
Reichenbach JR, Haacke EM (2001) High resolution BOLD venographic imaging: a window into brain function. NMR Biomed 14:453–467
Reichenbach JR, Venkatesan R, Schillinger DJ, et al (1997) Small vessels in the human brain: MR venography with deoxyhemoglobin as an intrinsic contrast agent. Radiology 204:272–277
Sujansky E, Conradi S (1995) Outcome of Sturge-Weber syndrome in 52 adults. Am J Med Genet 57:35–45
Arzimanoglou AA, Andermann F, Aicardi J, et al (2000) Sturge-Weber syndrome—indications and results of surgery in 20 patients. Neurology 55:1472–1479
Maria BL, Neufeld JA, Rosainz LC, et al (1998) Central nervous system structure and function in Sturge-Weber syndrome: evidence of neurologic and radiologic progression. J Child Neurol 13:606–618
Kossoff EH, Buck C, Freeman JM (2002) Outcomes of 32 hemispherectomies for Sturge-Weber syndrome worldwide. Neurology 59:1735–1738
Portilla P, Husson B, Lajaunias P, et al (2002) Sturge-Weber disease with repercussion on the prenatal development of the cerebral hemisphere. AJNR 23:490–492
Aylett SE, Neville BG, Cross JH, et al (1999) Sturge-Weber syndrome: cerebral haemodynamics during seizure activity. Dev Med Child Neurol 41:480–485
Adamsbaum C, Pinton F, Rolland Y, et al (1996) Accelerated myelination in early Sturge-Weber syndrome: MRI-SPECT correlations. Pediatr Radiol 26:759–762
Wasenko JJ, Rosenbloom SA, Duchesneau PM, et al (1990) Sturge-Weber syndrome: comparison of MR and CT characteristics. AJNR 11:131–134
Widdess-Walsh P, Friedman NR (2003) Left-sided nevus with contralateral leptomeningeal angiomatosis in a child with Sturge-Weber syndrome: a case report. J Child Neurol 18:304–305
Fischbein NJ, Barkovich AJ, Wu Y, et al (1998) Sturge-Weber syndrome with no leptomeningeal enhancement on MRI. Neuroradiology 40:177–180
Griffiths PD, Coley SC, Romanowski CA, et al (2003) Contrast-enhanced fluid-attenuated inversion recovery imaging for leptomeningeal disease in children. AJNR 24:719–723
Pfund Z, Kagawa K, Juhasz C, et al (2003) Quantitative analysis of gray- and white-matter volumes and glucose metabolism in Sturge-Weber syndrome. J Child Neurol 18:119–126
Lee JS, Asano E, Muzik O, et al (2001) Sturge-Weber syndrome: correlation between clinical course and FDG PET findings. Neurology 24:189–195
Griffiths PD, Blaser S, Boodram MB, et al (1996) Choroid plexus size in young children with Sturge-Weber syndrome. AJNR 17:175–180
Acknowledgements
This study was funded by the Deutsche Forschungsgemeinschaft (DFG) (Grant No. RE 1123/7–1) and the Nycomed Amersham Research Fellowship Grant (to J.R.R.) of the ECR 2002 Research and Education Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mentzel, HJ., Dieckmann, A., Fitzek, C. et al. Early diagnosis of cerebral involvement in Sturge-Weber syndrome using high-resolution BOLD MR venography. Pediatr Radiol 35, 85–90 (2005). https://doi.org/10.1007/s00247-004-1333-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-004-1333-2