Abstract
Objective
The aim was to investigate oxidative stress indicators in the blood of women with PCOS without and with metabolic syndrome (MS) and their dependency on lipids, comparing with healthy women. To our knowledge, this is the first study on this topic.
Methods
This was a cross-sectional study, and blood tests performed were double-blind. Within 3 months, 205 PCOS patients, from whom 55 also had MS, and 65 healthy women (control) were recruited. Malondialdehyde (MDA) was assessed as an important oxidative indicator, and superoxide dismutase (SOD), total antioxidant activity (TAA), vitamin C (VC), vitamin E (VE) and retinol (RET) as antioxidative indicators. Their correlation with features of MS was analyzed including their dependency on lipid pattern.
Results
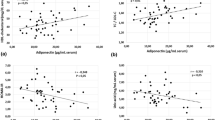
SOD, TAA, VE and RET in the PCOS group and PCOS + MS group were lower and MDA higher than in the control group (p < 0.05). SOD, VE and RET were the lowest in PCOS + MS group (p < 0.05). Thus, patients in this group had the highest oxidative stress levels but the lowest antioxidative capacity. SOD and TAA significantly decreased with increase of triglycerides (TG) and LDL-C in the PCOS + MS group (p < 0.05), but without dependency on HDL-C. Stepwise multiple linear regression analysis confirmed the different expression of oxidative stress in the three groups and decrease of SOD from control to PCOS group to PCOS + MS group, being associated with an increase of TG.
Conclusions
MS can accelerate the oxidative stress process in patients with PCOS and decrease the antioxidative capacity. The decreased antioxidant capacity in PCOS with MS is related to increased TG and LDL-C.

Similar content being viewed by others
References
Escobar-Morreale HF (2018) Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol 14:270–284
Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R (2016) Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril 106:6–15
Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ, International PCOS Network (2018) Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril 110:364–379
Ruan X, Song J, Gu M, Wang L, Wang H, Mueck AO (2018) Effect of Diane-35, alone or in combination with orlistat or metformin in Chinese polycystic ovary syndrome patients. Arch Gynecol Obstet 297:1557–1563
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285:2486–2497
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ (2015) Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 313:1973–1974
Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK (2011) Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 34:1323–1328
Kim HJ, Kim Y, Cho Y, Jun B, Oh KW (2014) Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998–2012. Int J Cardiol 174:64–72
Prasad DS, Kabir Z, Dash AK, Das BC (2012) Prevalence and risk factors for metabolic syndrome in Asian Indians: a community study from urban Eastern India. J Cardiovasc Dis Res 3:204–211
Caserta D, Adducchio G, Picchia S, Ralli E, Matteucci E, Moscarini M (2014) Metabolic syndrome and polycystic ovary syndrome: an intriguing overlapping. Gynecol Endocrinol 30:397–402
Moran LJ, Misso ML, Wild RA, Norman RJ (2010) Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update 16:347–363
Turrens JF (2003) Mitochondrial formation of reactive oxygen species. J Physiol 552:335–344
Murri M, Luque-Ramirez M, Insenser M, Ojeda-Ojeda M, Escobar-Morreale HF (2013) Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): a systematic review and meta-analysis. Hum Reprod Update 19:268–288
Insenser M, Montes-Nieto R, Murri M, Escobar-Morreale HF (2013) Proteomic and metabolomic approaches to the study of polycystic ovary syndrome. Mol Cell Endocrinol 370:65–77
Papalou O, Victor VM, Diamanti-Kandarakis E (2016) Oxidative stress in polycystic ovary syndrome. Curr Pharm Des 22:2709–2722
Carmina E, Dewailly D, Escobar-Morreale HF, Kelestimur F, Moran C, Oberfield S, Witchel SF, Azziz R (2017) Non-classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency revisited: an update with a special focus on adolescent and adult women. Hum Reprod Update 23:580–599
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SCJ, Spertus JA, Costa F (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112:2735–2752
Rocha MP, Marcondes JAM, Barcellos CRG, Hayashida SAY, Curi DDG, da Fonseca AM, Bagnoli VR, Baracat EC (2011) Dyslipidemia in women with polycystic ovary syndrome: incidence, pattern and predictors. Gynecol Endocrinol 27:814–819
Ruan X, Li M, Mueck AO (2018) Why does Polycystic Ovary Syndrome (PCOS) need long-term management? Curr Pharm Des 24:4685–4692
Mujica LS, Bridi A, Méa RD, Rissi VB, Guarda N, Moresco RN, Premaor MO, Antoniazzi AQ, Gonçalves PBD, Comim FV (2018) Oxidative stress and metabolic markers in pre- and postnatal polycystic ovary syndrome rat protocols. J Inflamm Res 11:193–202
Gonzalez F, Rote NS, Minium J, Kirwan JP (2006) Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J Clin Endocrinol Metab 91:336–340
Seleem AK, El Refaeey AA, Shaalan D, Sherbiny Y, Badawy A (2014) Superoxide dismutase in polycystic ovary syndrome patients undergoing intracytoplasmic sperm injection. J Assist Reprod Genet 31:499–504
Moti M, Amini L, Mirhoseini Ardakani SS, Kamalzadeh S, Masoomikarimi M, Jafarisani M (2015) Oxidative stress and anti-oxidant defense system in Iranian women with polycystic ovary syndrome. Iran J Reprod Med 13:373–378
Rodrigues JK, Dib LA, Ferriani RA, Jordao Junior AA, Navarro PADA (2010) Serum markers of oxidative stress and assisted reproduction procedures results in infertile patients with polycystic ovary syndrome and controls. Rev Bras Ginecol Obstet 32:118–125
Kurdoglu Z, Ozkol H, Tuluce Y, Koyuncu I (2012) Oxidative status and its relation with insulin resistance in young non-obese women with polycystic ovary syndrome. J Endocrinol Invest 35:317–321
Stocker R, Keaney JFJ (2004) Role of oxidative modifications in atherosclerosis. Physiol Rev 84:1381–1478
Sahaf B, Heydari K, Herzenberg LA, Herzenberg LA (2005) The extracellular microenvironment plays a key role in regulating the redox status of cell surface proteins in HIV-infected subjects. Arch Biochem Biophys 434:26–32
Vendemiale G, Guerrieri F, Grattagliano I, Didonna D, Muolo L, Altomare E (1995) Mitochondrial oxidative phosphorylation and intracellular glutathione compartmentation during rat liver regeneration. Hepatology 21:1450–1454
Zhang R, Liu H, Bai H, Zhang Y, Liu Q, Guan L, Fan P (2017) Oxidative stress status in Chinese women with different clinical phenotypes of polycystic ovary syndrome. Clin Endocrinol 86:88–96
Zhang J, Zhang Y, Liu H, Bai H, Wang Y, Jiang C, Fan P (2015) Antioxidant properties of high-density lipoproteins are impaired in women with polycystic ovary syndrome. Fertil Steril 103:1346–1354
Morelli NR, Scavuzzi BM, Miglioranza LHDS, Lozovoy MAB, Simão ANC, Dichi I (2018) Metabolic syndrome components are associated with oxidative stress in overweight and obese patients. Arch Endocrinol Metab 62:309–318
Macut D, BjekićMacut J, Savić-Radojević A (2013) Dyslipidemia and oxidative stress in pcos. Front Horm Res 40:51–63
Acknowledgements
The authors especially thank Prof. Xingming Li of the Capital Medical University (Beijing, China) for his assistance in statistical analysis of the data.
Funding
This study was supposed by Beijing Municipal Science & Technology Commission (Z161100000516143), Capital’s Funds for Health Improvement and Research (2016-2-2113), Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (XMLX201710), Beijing Municipality Health Technology High-level Talent (2014-2-016), Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20181401).
Author information
Authors and Affiliations
Contributions
HW: conceptualization: equal, data curation: lead, writing—original draft: lead; XR: conceptualization: lead, data curation: lead, funding acquisition: lead, project administration: lead, supervision: lead, writing—review and editing: lead; YL: data curation: equal; JC: data curation: supporting; AOM: conceptualization: equal, methodology: supporting, supervision: equal, writing—review and editing: lead.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, H., Ruan, X., Li, Y. et al. Oxidative stress indicators in Chinese women with PCOS and correlation with features of metabolic syndrome and dependency on lipid patterns. Arch Gynecol Obstet 300, 1413–1421 (2019). https://doi.org/10.1007/s00404-019-05305-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05305-7