Abstract
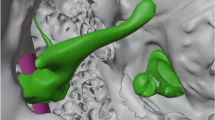
Functional outcomes and complications in otosclerosis surgery are governed by the surgeon’s experience. Thus, teaching the procedure to residents to guide them through the learning process as quickly as possible is challenging. Artificial 3D-printed temporal bones are replacing cadaver specimens in many institutions to learn mastoidectomy, but these are not suitable for middle ear surgery training. The goal of this work was to adapt such an artificial temporal bone to aid the teaching of otosclerosis surgery and to evaluate this tool. We have modified a commercially available 3D-printed temporal bone by replacing the incus and stapes of the model with in-house 3D-printed ossicles. The incus could be attached to a 6-axis force sensor. The stapes footplate was fenestrated and attached to a 1-axis force sensor. Six junior surgeons (residents) and seven senior surgeons (fellows or consultants) were enrolled to perform piston prosthesis placement and crimping as performed during otosclerosis surgery. The time required to perform the tasks and the forces applied to the incus and stapes were collected and analyzed. No statistically significant differences were observed between the junior and senior groups for time taken to perform the tasks and the forces applied to the incus during crimping and placement of the prosthesis. However, significantly lower forces were applied to the stapes by the senior surgeons in comparison with the junior surgeons during prosthesis placement (junior vs senior group, 328 ± 202.9 vs 80 ± 99.6 mN, p = 0.008) and during prosthesis crimping (junior vs senior group, 565 ± 233 vs 66 ± 48.6 mN, p = 0.02). We have described a new teaching tool for otosclerosis surgery based on the modification of a 3D-printed temporal bone to implement force sensors on the incus and stapes. This tool could be used as a training tool to help the residents to self-evaluate their progress with recording of objective measurements.






Similar content being viewed by others
References
Caldart AU, Terruel I, Enge DJ Jr, Kurogi AS, Buschle M, Mocellin M (2007) Stapes surgery in residency: the UFPR clinical hospital experience. Braz J Otorhinolaryngol 73(5):647–653
Lial PI, Soares VY, Viana LM, Sampaio AL, Oliveira CA, Bahmad FJ (2013) Stapedotomy in a residency training program. Int Tinnitus J 18(2):163–167
Kursten R, Schneider B, Zrunek M (1994) Long-term results after stapedectomy versus stapedotomy. Am J Otol 15(6):804–806
Perkins RC (1980) Laser stepedotomy for otosclerosis. Laryngoscope 90(2):228–240
Nguyen Y, Bozorg Grayeli A, Belazzougui R, Rodriguez M, Bouccara D, Smail M, Sterkers O (2008) Diode laser in otosclerosis surgery: first clinical results. Otol Neurotol 29(4):441–446
Nguyen Y, Miroir M, Kazmitcheff G, Ferrary E, Sterkers O, Grayeli AB (2011) From conception to application of a tele-operated assistance robot for middle ear surgery. Surg Innov 19(3):241–251
Kerr B, O’Leary JP (1999) The training of the surgeon: Dr. Halsted’s greatest legacy. Am Surg 65(11):1101–1102
Levenson MJ (1999) Methods of teaching stapedectomy. Laryngoscope 109(11):1731–1739
George AP, De R (2010) Review of temporal bone dissection teaching: how it was, is and will be. J Laryngol Otol 124(2):119–125
Scott A, De R, Sadek SA, Garrido MC, Courteney-Harris RG (2001) Temporal bone dissection: a possible route for prion transmission? J Laryngol Otol 115(5):374–375
Bakhos D, Velut S, Robier A, Al zahrani M, Lescanne E (2010) Three-dimensional modeling of the temporal bone for surgical training. Otol Neurotol 31(2):328–334
Cordero A, Benitez S, Reyes P, Vaca M, Polo R, Perez C, Alonso A, Cobeta I (2015) Ovine ear model for fully endoscopic stapedectomy training. Eur Arch Otorhinolaryngol 272(9):2167–2174
Sorensen MS, Mosegaard J, Trier P (2009) The visible ear simulator: a public PC application for GPU-accelerated haptic 3D simulation of ear surgery based on the visible ear data. Otol Neurotol 30(4):484–487
Roosli C, Sim JH, Mockel H, Mokosch M, Probst R (2013) An artificial temporal bone as a training tool for cochlear implantation. Otol Neurotol 34(6):1048–1051
Kazmitcheff G, Miroir M, Nguyen Y, Ferrary E, Sterkers O, Cotin S, Duriez C, Grayeli AB (2014) Validation method of a middle ear mechanical model to develop a surgical simulator. Audiol Neurootol 19(2):73–84
Bergin M, Sheedy M, Ross P, Wylie G, Bird P (2014) Measuring the forces of middle ear surgery; evaluating a novel force-detection instrument. Otol Neurotol 35(2):e77–e83
Rothbaum DL, Roy J, Hager GD, Taylor RH, Whitcomb LL, Francis HW, Niparko JK (2003) Task performance in stapedotomy: comparison between surgeons of different experience levels. Otolaryngol Head Neck Surg 128(1):71–77
Yung MW, Oates J, Vowler SL (2006) The learning curve in stapes surgery and its implication to training. Laryngoscope 116(1):67–71
Sergi B, Paludetti G (2016) Can the learning curve in stapes surgery predict future functional outcome? Acta Otorhinolaryngol Ital 36(2):135–138
Mathews SB, Hetzler DG, Hilsinger RL Jr (1997) Incus and stapes footplate simulator. Laryngoscope 107(12 Pt 1):1614–1616
Monfared A, Mitteramskogler G, Gruber S, Salisbury JK Jr, Stampfl J, Blevins NH (2012) High-fidelity, inexpensive surgical middle ear simulator. Otol Neurotol 33(9):1573–1577
Owa AO, Gbejuade HO, Giddings C (2003) A middle-ear simulator for practicing prosthesis placement for otosclerosis surgery using ward-based materials. J Laryngol Otol 117(6):490–492
Mills R, Lee P (2003) Surgical skills training in middle-ear surgery. J Laryngol Otol 117(3):159–163
Murrant NJ, Gatland DJ (1989) Temporal bone laboratory training for stapedectomy. J Laryngol Otol 103(9):833–834
Linke R, Leichtle A, Sheikh F, Schmidt C, Frenzel H, Graefe H, Wollenberg B, Meyer JE (2013) Assessment of skills using a virtual reality temporal bone surgery simulator. Acta Otorhinolaryngol Ital 33(4):273–281
Kazmitcheff G, Nguyen Y, Miroir M, Pean F, Ferrary E, Cotin S, Sterkers O, Duriez C (2014) Middle-ear microsurgery simulation to improve new robotic procedures. Biomed Res Int 2014:891742
Murbe D, Huttenbrink KB, Zahnert T, Vogel U, Tassabehji M, Kuhlisch E, Hofmann G (2001) Tremor in otosurgery: influence of physical strain on hand steadiness. Otol Neurotol 22(5):672–677
Ovari A, Nemenyi D, Just T, Schuldt T, Buhr A, Mlynski R, Csokay A, Pau HW, Valalik I (2016) Positioning Accuracy in Otosurgery Measured with Optical Tracking. PLoS One 11(3):e0152623
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and animal rights statement
This article does not contain any studies with human participants or animals performed by any of the authors. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors indicate no potential conflict of interest. The authors would like to thank Armand Czaplinski for his assistance with the drawing of the 3D models, the modified incus, and stapes used in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 3 (MP4 79771 kb)
Rights and permissions
About this article
Cite this article
Nguyen, Y., Mamelle, E., De Seta, D. et al. Modifications to a 3D-printed temporal bone model for augmented stapes fixation surgery teaching. Eur Arch Otorhinolaryngol 274, 2733–2739 (2017). https://doi.org/10.1007/s00405-017-4572-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4572-1