Abstract
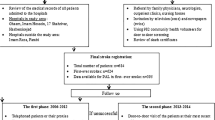
Physical activity prevents stroke and is associated with less severe strokes. The neuroprotective effect in patients treated with intravenous (i.v.) recombinant tissue plasminogen activator (rt-PA), remains uncertain. We aimed at evaluating the relationship between previous physical activity and outcomes in stroke patients treated with i.v. rt-PA. OPHELIE-SPORT was a prospective observational multicenter study conducted in French and Japanese stroke patients treated with i.v. rt-PA. We evaluated the presence, weekly duration (<2, 2–5, >5 h) and intensity (light, moderate, heavy) of previous leisure-time physical activity according to standardized criteria. The primary end-point was an excellent outcome [modified Rankin Scale (mRS) 0–1 or similar to the pre-stroke mRS] after 3 months. Secondary end-points were good outcome (mRS 0–2 or similar to the pre-stroke mRS), and death. Of 519 patients, 74 (14.3 %) had regular physical activity before stroke. They were 14 years younger (p < 0.001), treated 25 min earlier (p = 0.004) and more likely to be men, free of pre-stroke handicap (mRS = 0), atrial fibrillation, arterial hypertension, and diabetes mellitus. National Institutes of Health Stroke Scale scores, at baseline (p = 0.183) and 24 h later (p = 0.203), did not differ between patients with and without physical activity. After adjustment on confounders, there was no association between previous leisure-time physical activity and outcome. Outcomes 3 months after treatment of cerebral ischaemia with i.v. rt-PA are not influenced by previous physical activity.

Similar content being viewed by others
References
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. New Engl J Med 333:1581–1587
Sandercock P, Wardlaw JM, Lindley RI et al (2012) The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 379:2352–2363
Ding Y-H, Young CN, Luan X et al (2005) Exercise preconditioning ameliorates inflammatory injury in ischemic rats during reperfusion. Acta Neuropathol 109:237–246
Hayes K, Sprague S, Guo M et al (2008) Forced, not voluntary, exercise effectively induces neuroprotection in stroke. Acta Neuropathol 115:289–296
Gertz K, Priller J, Kronenberg G et al (2006) Physical activity improves long-term stroke outcome via endothelial nitric oxide synthase-dependent augmentation of neovascularization and cerebral blood flow. Circ Res 99:1132–1140
Ding Y, Li J, Luan X et al (2004) Exercise pre-conditioning reduces brain damage in ischemic rats that may be associated with regional angiogenesis and cellular overexpression of neurotrophin. Neuroscience 124:583–591
Deplanque D, Masse I, Lefebvre C et al (2006) Prior TIA, lipid-lowering drug use, and physical activity decrease ischemic stroke severity. Neurology 67:1403–1410
Stroud N, Mazwi TML, Case LD et al (2009) Prestroke physical activity and early functional status after stroke. J Neurol Neurosurg Psychiatr 80:1019–1022
Curry A, Guo M, Patel R et al (2010) Exercise pre-conditioning reduces brain inflammation in stroke via tumor necrosis factor-alpha, extracellular signal-regulated kinase 1/2 and matrix metalloproteinase-9 activity. Neurol Res 32:756–762
Ding Y-H, Mrizek M, Lai Q et al (2006) Exercise preconditioning reduces brain damage and inhibits TNF-alpha receptor expression after hypoxia/reoxygenation: an in vivo and in vitro study. Curr Neurovasc Res 3:263–271
Guo M, Cox B, Mahale S et al (2008) Pre-ischemic exercise reduces matrix metalloproteinase-9 expression and ameliorates blood-brain barrier dysfunction in stroke. Neuroscience 151:340–351
Guo M, Lin V, Davis W et al (2008) Preischemic induction of TNF-alpha by physical exercise reduces blood-brain barrier dysfunction in stroke. J Cer Blood flow Metab 28:1422–1430
Endres M, Gertz K, Lindauer U et al (2003) Mechanisms of stroke protection by physical activity. Ann Neurol 54:582–590
Zwagerman N, Sprague S, Davis MD et al (2010) Pre-ischemic exercise preserves cerebral blood flow during reperfusion in stroke. Neurol Res 32:523–529
Ding Y-H, Luan X-D, Li J et al (2004) Exercise-induced overexpression of angiogenic factors and reduction of ischemia/reperfusion injury in stroke. Curr Neurovasc Res 1:411–420
Liebelt B, Papapetrou P, Ali A et al (2010) Exercise preconditioning reduces neuronal apoptosis in stroke by up-regulating heat shock protein-70 (heat shock protein-72) and extracellular-signal-regulated-kinase 1/2. Neuroscience 166:1091–1100
Chaudhry K, Rogers R, Guo M et al (2010) Matrix metalloproteinase-9 (MMP-9) expression and extracellular signal-regulated kinase 1 and 2 (ERK1/2) activation in exercise-reduced neuronal apoptosis after stroke. Neurosci Lett 474:109–114
Jia J, Hu Y-S, Wu Y et al (2009) Pre-ischemic treadmill training affects glutamate and gamma aminobutyric acid levels in the striatal dialysate of a rat model of cerebral ischemia. Life Sci 84:505–511
Yang X, He Z, Zhang Q et al (2012) Pre-ischemic treadmill training for prevention of ischemic brain injury via regulation of glutamate and its transporter GLT-1. Int J Mol Sci 13:9447–9459
Ricciardi AC, López-Cancio E, Pérez de la Ossa N et al (2014) Prestroke physical activity is associated with good functional outcome and arterial recanalization after stroke due to a large vessel occlusion. Cerebrovasc Dis 37:304–311
Rist PM, Lee I-M, Kase CS et al (2011) Physical activity and functional outcomes from cerebral vascular events in men. Stroke 42:3352–3356
Murao K, Leys D, Jacquin A et al (2014) Thrombolytic therapy for stroke in patients with preexisting cognitive impairment. Neurology 82:2048–2054
Kamouchi M, Matsuki T, Hata J et al (2011) Prestroke glycemic control is associated with the functional outcome in acute ischemic stroke: the Fukuoka Stroke Registry. Stroke 42:2788–2794
The European Stroke Organisation (ESO) Executive Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507 (see update at http://www.eso-stroke.org)
Shinohara Y, Yamaguchi T (2008) Outline of the Japanese guidelines for the management of stroke 2004 and subsequent revision. Int J Stroke 3:55–62
Minematsu K, Toyoda K, Hirano T et al (2013) Guidelines for the intravenous application of recombinant tissue-type plasminogen activator (alteplase), the second edition, October 2012: a guideline from the Japan Stroke Society. J Stroke Cerebrovasc 22:571–600
Lyden P, Brott T, Tilley B et al (1994) Improved reliability of the NIH Stroke Scale using video training. NINDS TPA Stroke Study Group. Stroke 25:2220–2226
Van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Janssen PM, Visser NA, Mees SM et al (2010) Comparison of telephone and face-to-face assessment of the modified Rankin Scale. Cerebrovasc Dis 29:137–139
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Sacco RL, Gan R, Boden-Albala B et al (1998) Leisure-time physical activity and ischemic stroke risk: the Northern Manhattan Stroke Study. Stroke 29:380–387
Krarup L-H, Truelsen T, Pedersen A et al (2007) Level of physical activity in the week preceding an ischemic stroke. Cerebrovasc Dis 24:296–300
Minematsu K, Okada Y et al (2010) Thrombolysis with 0.6 mg/kg intravenous alteplase for acute ischemic stroke in routine clinical practice: the Japan post-Marketing Alteplase Registration Study (J-MARS). Stroke 41:1984–1989
Acknowledgments
We are grateful to contributors listed below.
Participating centers and contributors are listed. The number of patients recruited per center is given in parentheses.
Lille, France (241) Didier Leys (PI), Charlotte Cordonnier, Hilde Hénon, Marie Bodenant, Nelly Dequatre, Solène Moulin, Costanza Rossi, Dominique Deplanque, Anne-Marie Mendyk, Valentin Vergriete.
Bordeaux, France (166) Igor Sibon (PI), Mathilde Poli, Sharmila Sagnier.
Rennes, France (57) Thomas Ronzière (PI), Veronica Lassalle, Jean François Pinel, Stéphane Vannier, Francoise Kestens.
National Hospital Organization Kyushu Medical Center, Japan (19) Yasushi Okada (PI), Masahiro Yasaka, Yoshinobu Wakisaka, Kei Murao.
Japanese Red Cross Fukuoka Hospital, Japan (15) Kenichirou Fujii.
Amiens, France (10) Olivier Godefroy (PI), Jean Marc Bugnicourt, Sandrine Canaple, Chantal Lamy.
Kawasaki Medical School, Japan (5) Kazumi Kimura.
Steel Memorial Yawata Hospital, Japan (3) Shigeru Fujimoto.
Kyushu Rosai Hospital, Japan (3) Shuji Arakawa.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Study funding
University Lille 2 (EA 1046), Lille University hospital, ADRINORD, SSHN grant from the French government to Dr. Murao, French Ministry of Health (PHRC STROKAVENIR Network), INSERM and La Revue Neurologique grant to Dr. Murao. Alicante had made available the eCRF for the French part of the study.
Conflicts of interest
Dr. Amélie Decourcelle reports no disclosures. Dr. Solène Moulin reports no disclosures. Dr. Igor Sibon reports no disclosures. Dr. Kei Murao reports no disclosures. Dr. Thomas Ronzière reports grants from Boehringer-Ingelheim. Dr. Olivier Godefroy had partnership with Novartis and Pharnext for trials, speaker at symposia and advisory board meetings. Dr. Mathilde Poli reports no disclosures. Dr. Charlotte Cordonnier had partnership with Boehringer-Ingelheim for trials and speaker at symposia, fees for which were paid towards research at ADRINORD (Association pour le Développement de la Recherche et de l’Innovation dans le Nord-Pas de Calais). Dr. Sharmila Sagnier reports no disclosures. Dr. Veronica Lassalle reports no disclosures. Dr. Yasushi Okada reports no disclosures. Dr. Jean-Louis Mas had partnership with Boehringer-Ingelheim for trials, speaker at symposia and advisory board meetings. Dr. Régis Bordet reports no disclosures. Dr. Didier Leys had partnership with Boehringer-Ingelheim for trials, speaker at symposia and advisory board meetings, fees for which were paid towards research at ADRINORD (Association pour le Développement de la Recherche et de l’Innovation dans le Nord-Pas de Calais).
Ethical standard
The study has been approved by the appropriate ethical committees in France and in Japan, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons, or their close relatives, gave their informed consent prior to their inclusion in the study.
Additional information
On behalf of the OPHELIE-SPORT investigators.
On behalf of the STROKAVENIR network.
OPHELIE-SPORT investigators are listed in Acknowledgments.
Rights and permissions
About this article
Cite this article
Decourcelle, A., Moulin, S., Sibon, I. et al. Influence of previous physical activity on the outcome of patients treated by thrombolytic therapy for stroke. J Neurol 262, 2513–2519 (2015). https://doi.org/10.1007/s00415-015-7875-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7875-4