Abstract
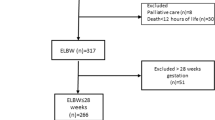
GEIDIS is a national-based research-net registry of patients with bronchopulmonary dysplasia (BPD) from public and private Spanish hospitals. It was created to provide data on the clinical characterization and follow-up of infants with BPD until adulthood. The purpose of this observational study was to analyze the characteristics and the impact of perinatal risk factors on BPD severity. The study included 1755 preterm patients diagnosed with BPD. Of the total sample, 90.6% (n = 1591) were less than 30 weeks of gestation. The median gestational age was 27.1 weeks (25.8–28.5) and median birth weight 885 g (740–1,070 g). A total of 52.5% (n = 922) were classified as mild (type 1), 25.3% (n = 444) were moderate (type 2), and 22.2% (n = 389) were severe BPD (type 3). In patients born at under 30 weeks’ gestation, most pre-and postnatal risk factors for type 2/3 BPD were associated with the length of exposure to mechanical ventilation (MV). Independent prenatal risk factors were male gender, oligohydramnios, and intrauterine growth restriction. Postnatal risk factors included the need for FiO2 of > 0.30 in the delivery room, nosocomial pneumonia, and the length of exposure to MV.
Conclusion: In this national-based research-net registry of BPD patients, the length of MV is the most important risk factor associated with type 2/3 BPD. Among type 3 BPD patients, those who required an FiO2 > .30 at 36 weeks’ postmenstrual age had a higher morbidity, during hospitalization and at discharge, compared to those with nasal positive pressure but FiO2 < .30.
What is Known: • BPD is a highly complex multifactorial disease associated with preterm birth. | |
What is New: • The length of exposure to mechanical ventilation is the most important postnatal risk factor associated to bronchopulmonary severity which modulate the effect of most pre and postnatal risk factors. • Among patients with BPD, the requirement for FiO2 >.30% at 36 weeks of postmenstrual age is associated with greater morbidity during hospitalization and at discharge. |

Similar content being viewed by others
Data availability
Data are available on the online GEIDIS registry platform.
Code availability
N/A.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- EN:
-
Enteral nutrition
- GA:
-
Gestational age
- GEIDIS:
-
Spanish Bronchopulmonary Dysplasia Research Group
- iNO:
-
Inhaled nitric oxide therapy
- IUGR:
-
Intrauterine growth restriction
- MV:
-
Mechanical ventilation
- NEC:
-
Necrotizing enterocolitis
- PDA:
-
Paten ductus arteriosus
- PMA:
-
Postmenstrual age
References
Owen LS et al (2017) The evolution of modern respiratory care for preterm infants. Lancet 389(10079):1649–1659
Stoll BJ et al (2015) Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314(10):1039–1051
Abman SH, Bancalari E, Jobe A (2017) The evolution of bronchopulmonary dysplasia after 50 years. Am J Respir Crit Care Med 195(4):421–424
Álvarez-Fuente M et al (2017) The economic impact of prematurity and bronchopulmonary dysplasia. Eur J Pediatr 176(12):1587–1593
SEN1500 (2016) Análisis de los datos de morbimortalidad año
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729
Hernandez LA et al (1985) Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. J Appl Physiol 66(5):2364–2368
Jobe AH (2015) Animal models, learning lessons to prevent and treat neonatal chronic lung disease. Front Med (Lausanne) 2:49
Philip AG (1975) Oxygen plus pressure plus time: the etiology of bronchopulmonary dysplasia. Pediatrics 55(1):44–50
Dreyfuss D et al (1988) High inflation pressure pulmonary edema: respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 137(5):1159–1164
Isayama T et al (2012) Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics 130(4):e957–e965
Stoll BJ et al (2010) Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126(3):443–456
Klinger G et al (2013) Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol 208(2):115.e1–9
Dargaville PA et al (2016) Incidence and outcome of CPAP failure in preterm infants. Pediatrics 138(1):15
Fuchs H et al (2011) Predictors of early nasal CPAP failure and effects of various intubation criteria on the rate of mechanical ventilation in preterm infants of <29 weeks gestational age. Arch Dis Child Fetal Neonatal Ed 96(5):F343–F347
Bancalari E, Jain D (2018) Bronchopulmonary dysplasia: can we agree on a definition? Am J Perinatol 35(6):537–540
Hines D et al (2017) Scoping review shows wide variation in the definitions of bronchopulmonary dysplasia in preterm infants and calls for a consensus. Acta Paediatr 106(3):366–374
Ibrahim J, Bhandari V (2018) The definition of bronchopulmonary dysplasia: an evolving dilemma. Pediatr Res 84(5):586–588
Jobe AH, Steinhorn R (2017) Can we define bronchopulmonary dysplasia? J Pediatr 188:19–23
Kinsella JP, Greenough A, Abman SH (2006) Bronchopulmonary dysplasia. Lancet 367(9520):1421–1431
Ronkainen E et al (2015) New BPD predicts lung function at school age: follow-up study and meta-analysis. Pediatr Pulmonol 50(11):1090–1198
Higgins RD et al (2018) Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr 197:300–308
Jensen EA et al (2019) The diagnosis of bronchopulmonary dysplasia in very preterm infants: an evidence-based approach. Am J Respir Crit Care Med 200(6):751–759
Bancalari E, Claure N, Jain D (2019) Diagnostic classification of bronchopulmonary dysplasia: a compromise between defining lung disease versus long-term outcome prediction. Am J Respir Crit Care Med 200(10):1322–1323
Wu KY et al (2020) Characterization of disease phenotype in very preterm infants with severe bronchopulmonary dysplasia. Am J Respir Crit Care Med 201(11):1398–1406
Poindexter BB et al (2015) Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc 12(12):1822–1830
Villamor-Martinez E et al (2019) Association of chorioamnionitis with bronchopulmonary dysplasia among preterm infants: a systematic review, meta-analysis, and metaregression. JAMA Netw Open 2(11):e1914611
Pietrasanta C et al (2019) Impact of different stages of intrauterine inflammation on outcome of preterm neonates: gestational age-dependent and -independent effect. PLoS One 14(2):e0211484
Clyman RI et al (2021) Prolonged tracheal intubation and the association between patent ductus arteriosus and bronchopulmonary dysplasia: a secondary analysis of the PDA-TOLERATE trial. J Pediatr 229:283-288.e2
Clyman RI et al (2020) Relationship between duration of infant exposure to a moderate-to-large patent ductus arteriosus shunt and the risk of developing bronchopulmonary dysplasia or death before 36 weeks. Am J Perinatol 37(2):216–223
Zysman-Colman Z et al (2013) Bronchopulmonary dysplasia: trends over three decades. Paediatr Child Health 18(2):86–90
Laughon MM et al (2011) Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med 183(12):1715–1722
Naeye RL, Freeman RK, Blanc WA (1974) Nutrition, sex, and fetal lung maturation. Pediatr Res 8(3):200–204
Lorente-Pozo S et al (2018) Influence of sex on gestational complications, fetal-to-neonatal transition, and postnatal adaptation. Front Pediatr 6:63
Fulton CT et al (2018) Gene expression signatures point to a male sex-specific lung mesenchymal cell PDGF receptor signaling defect in infants developing bronchopulmonary dysplasia. Sci Rep 8(1):17070
Kitterman JA et al (2002) Effects of oligohydramnios on lung growth and maturation in the fetal rat. Am J Physiol Lung Cell Mol Physiol 282(3):L431–L439
Lindner W et al (2002) Acute respiratory failure and short-term outcome after premature rupture of the membranes and oligohydramnios before 20 weeks of gestation. J Pediatr 140(2):177–182
Weiner E et al (2019) Amniotic fluid volume at presentation with early preterm prelabor rupture of membranes and association with severe neonatal respiratory morbidity. Ultrasound Obstet Gynecol 54(6):767–773
Aikio O et al (2012) Transient defect in nitric oxide generation after rupture of fetal membranes and responsiveness to inhaled nitric oxide in very preterm infants with hypoxic respiratory failure. J Pediatr 161(3):397-403.e1
Mirza H et al (2018) Natural history of postnatal cardiopulmonary adaptation in infants born extremely preterm and risk for death or bronchopulmonary dysplasia. J Pediatr 198:187-193.e1
Chandrasekharan P et al (2017) Early use of inhaled nitric oxide in preterm infants: is there a rationale for selective approach? Am J Perinatol 34(5):428–440
Kim DH et al (2012) Risk factors for pulmonary artery hypertension in preterm infants with moderate or severe bronchopulmonary dysplasia. Neonatology 101(1):40–46
Mourani PM, Abman SH (2013) Pulmonary vascular disease in bronchopulmonary dysplasia: pulmonary hypertension and beyond. Curr Opin Pediatr 25(3):329–337
Abman SH (2001) Bronchopulmonary dysplasia: “a vascular hypothesis.” Am J Respir Crit Care Med 164(10 Pt 1):1755–1756
Bhatt AJ et al (2001) Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med 164(10 Pt 1):1971–1980
Check J et al (2013) Fetal growth restriction and pulmonary hypertension in premature infants with bronchopulmonary dysplasia. J Perinatol 33(7):553–557
Taglauer E, Abman SH, Keller RL (2018) Recent advances in antenatal factors predisposing to bronchopulmonary dysplasia. Semin Perinatol 42(7):413–424
Laughon M et al (2009) Patterns of respiratory disease during the first 2 postnatal weeks in extremely premature infants. Pediatrics 123(4):1124–1131
Acknowledgements
The authors would like to thank Professor Eduardo Bancalari for assistance in revision of the manuscript the Institute for the Improvement in Healthcare (IMAS) for its support and Professor Julio Ancochea, Professor Jaques Belik, Professor Borja García-Cosio and Joan B. Soriano members of the GEIDIS advisory committee. María del Mar Serrano Martín, María Cristina Pradillo Martín: Hospital Materno Infantil Málaga. Ester Sanz López, Cristina Ramos Navarro, Elena Maderuelo Rodriguez: Hospital Gregorio Marañón. Ohiana Muga Zuriarrain, Paula Corcuera Elosegui: Hospital Universitario Donostia. Margarita Ferrer, Mikel Santiago, Eneritz Guerra: Hospital Universitario de Cruces. Ana Gutiérrez Amorós, Maria Angeles Villar: Hospital de Basurto; Sonia Sánchez de Antonio, Marta del Hoyo Moracho: Hospital de Txagorritxu. Wifredo Coroleu Lletget, Mª del Mar Martínez Colls: Hospital Germans Trias i Pujol; Segundo Rite Gracia, Carlos Martín Vicente: Hospital Miguel Servet (Zaragoza); Miguel Ramón, María José García Borau, Fátima Castillo, Gema García del Cerro, Laura Armendáriz: Hospital St. Pau; Amalui Vásquez, Olalla Otero Vaccarello, Aitana García: Hospital Joan XXIII. Julia Arroyo: Hospital St. Joan de Reus; Cristina Carrasco Carrasco, Jordi Costa Colomer: H. Sant Joan Deu. Juan José Comuñas Gómez, Félix Castillo Salinas, Antonio Moreno Galdó, Alba Torrent Vernetta, Carmen Ribes: Hospital Valle de Hebrón (Vall d´Hebron); Jose María Lloreda, Carolina Diaz Garcia, Ana Marin Cassinello, Javier Martinez Olmos, Jose Luis Leante Castellanos: Hospital General Universitario Santa Lucía (Cartagena); Verónica Jimenez Escobar, Inés Esteban Díez: Hospital San Pedro (Logroño); Pilar Robles Cascallar: H. U. Puerta de Hierro (Majadahonda). Cristina de Frutos: Hospital Universitario de Burgos; Susana Herrero Pérez: Hospital Son Llàtzer (Palma de Mallorca); Roser Porta Ribera, Miquel Ramon Jimenez: Hospital Universitario Quiron Dexeus. Francisco Canals Candela: Hospital General Universitario de Elche; Debora Becerra Alonso: Hospital Universitario de Canarias. Amaya Pérez Ocón, Gemma Sierra Colomina: Complejo Hospitalario de Navarra (Ant. H. Virgen del Camino); Eva García Valle: Hospital. Rocio Sancho Gutierrez: Hospital Universitario Marqués de Valdecilla. Victoria Ramos Ramos, Carmen Aragón Fernández, Maricruz Díaz Colom: Hospital Universitario Jerez de la Frontera. Miquel Fiol Jaume, Catalina Bover, Francisco de Borja Osona Rodríguez de Torres, Ignacio Benitez Segura: Hospital Son Espases, Palma de Mallorca. Luis Pérez Baena, Orlando Mesa Medina: Nuestra Señora de la Candelaria; Santiago Pérez Tarazona, Isidoro Cortell Aznar: Hospital La Fe. Valencia; Agustín Molina Merino, Eva Flor Macián, Silvia Castillo Corullón, Javier Estañ Capell: Hospital Clínico Universitario de Valencia, Maria Baquero Cano: Hospital General Albacete. Josep Sirvent Gómez, María Taboada Perianes: CHUAC (Hosp. J. Canalejo) A Coruña, Alicia Sardina Ríos, María Montserrat Berrocal: Hospital Ntra. Sra. Del Cristal Orense; Pilar Crespo Suarez, Javier Vilas González: Hospital Provincial De Pontevedra; Carme Figaró, Roser Ayats: Hospital Parc Tauli; Elena Hierro Delgado, Paula Alonso Quintela: Complejo Hospitalario de León. Marta Suárez Rodríguez, Laura Mantecón Fernandez: HUCA (Hosp. Unv. Central de Asturias); Marianela Marcos Temprano, Asunción Pino Vázquez: Hospital Clínico Universitario de Valladolid. Sara Isabel Marín Urueña, Mar Montejo Vicente,; Nuria Díez Monge: Hospital Rio Hortega, Valladolid; Maria Jesús Rodríguez Sáez; Ana Concheiro: Complejo Hospitalario de Vigo. Mercedes García Reymundo: Hospital de Merida (Badajoz); Elena Vázquez Rodríguez, Francisco José Carrión Castellet: Hospital de Valme (Sevilla). Elisabeth Gómez Santos, David Mora Navarro: Hospital Juan Ramón Jimenez (Huelva); Mª Dolores Ruiz González, Javier; Torres Borrego: Hospital Reina Sofía (Córdoba); Ana Raquel Barrio Sacristán, Ofelia Fernández de la Cruz: Hospital San Pedro de Alcantara (Cáceres). Maria Carmen Martínez Padilla, Victoria Esteban Marfil: Hospital Universitario Médico quirúrgico de Jaen. Guadalupe Pérez Pérez, Leonor Bardallo Cruzado, Anselmo Andrés, Guadalupe Pérez, Pérez Hospital Universitario Virgen de la Macareno (Sevilla). Elisa García García, Isabel Delgado Pecellín, Maria José Moreno Valera, Antonio Pavón Delgado: Hospital Virgen del Rocio (Sevilla). Alfonso Romero Otero, José Fernández-Cantalejo Padial: Fundación Jimenez Díaz, Madrid; Mª Salomé Albi Rodríguez, Carmen Luna: Hospital 12 de Octubre, Madrid. Dr Luis Arruza Gómez, Santiago Rueda Esteban; Hospital Clínico San Carlos. Jesus Cecilio Lopez Menchero Oliva: Hospital de Ciudad Real. Ana María Sanchéz Torres, Olga de la Serna Blázquez: Hospital La Paz, Madrid; Ana Remesal Escalero, Teresa Sánchez Vélez, Barajas Sánchez: Complejo Hospitalario de Salamanca. Mª Dolores Sánchez-Redondo, Sánchez-Gabriel María Jesús Navarro Carmona: Hospital Virgen de la Salud (Toledo). Doña María Penín Anton, Ana Navarro Dourdil; José Beceiro Mosquera: Hospital Príncipe de Asturias (Alcalá de Henares.). Marta Ruiz Jimenez, Gemma Villar Villar: Hospital Universitario de Getafe. Sergio Quevedo Teruel, María Arroyas Mª Luz García García: Hospital Severo Ochoa. Eva García Cantó, Luis Moral Gil: Hospital General Universitario de Alicante. Ana Rosa Sánchez Vázquez, Teresa Rubí Ruiz: Hospital Torrecardenas (Almería). Juan José Agüera Arenas Manuel Sanchéz Solís: Hospital Clínico Universitario Virgen de la Arrixaca (Murcia). Paula Méndez Abad: Hospital Puerta del Mar. Emma Ametller, Andreu Peñas: Hospital Josep Trueta Girona, Manuel Gresa Muñoz, Elisa Canino Calderín:. Hospital Materno Infantil de Las Palmas. Felipe Verjano, Sergio Ocaña: Hospital Costa del Sol. Ana Muñoz Serrano: Hospital la Mancha Centro (Alcazar de San Juan). Mario Ferrer Vázquez: Hospital General de Castellón. Eduardo Narbona López, A. Jerez Calero: Hospital Universitario San Cecilio (Granada).
Author information
Authors and Affiliations
Consortia
Contributions
CN designed the study, performed the acquisition and analysis of the data, and draft the test. EMR, ACG, SPT, SRE, AST, MSS, and ESL designed the study, collected data during the study period, and revised the draft. MSL designed the study, made contributions on the conception of the work, and revised the draft critically.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any interventional studies with human participants or animals performed by any of the authors. This study was approved and monitored by the Clinical Research Ethics Committee at Virgen de la Arrixaca Hospital. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Consent to participate
Informed consent was obtained from the legal guardians of participants included in the study.
Consent for publication
All the authors revised and approved the final version of the text and consents its publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ramos-Navarro, C., Maderuelo-Rodríguez, E., Concheiro-Guisán, A. et al. Risk factors and bronchopulmonary dysplasia severity: data from the Spanish Bronchopulmonary Dysplasia Research Network. Eur J Pediatr 181, 789–799 (2022). https://doi.org/10.1007/s00431-021-04248-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04248-z