Abstract
Objectives
This study aimed to compare the performance of a xenograft (XG) and a biomimetic synthetic graft (SG) in three-wall alveolar defects in minipigs by means of 3D computerised tomography and histology.
Materials and methods
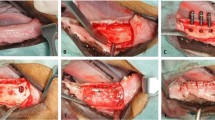
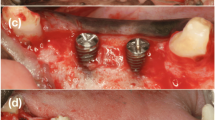
Eight minipigs were used. A total of eight defects were created in the jaw of each animal, three of which were grafted with XGs, three with SGs, and two were left empty as a negative control. The allocation of the different grafts was randomised. Four animals were euthanised at 6 weeks and four at 12 weeks. The grafted volume was then measured by spiral computed tomography to assess volume preservation. Additionally, a histological analysis was performed in undecalcified samples by backscattered scanning electron microscopy and optical microscopy after Masson’s trichrome staining.
Results
A linear mixed-effects model was applied considering four fixed factors (bone graft type, regeneration time, anatomic position, and maxilla/mandible) and one random factor (animal). The SG exhibited significantly larger grafted volume (19%) than the XG. The anterior sites preserved better the grafted volume than the posterior ones. Finally, regeneration time had a positive effect on the grafted volume. Histological observations revealed excellent osseointegration and osteoconductive properties for both biomaterials. Some concavities found in the spheroidal morphologies of SGs were associated with osteoclastic resorption.
Conclusions
Both biomaterials met the requirements for bone grafting, i.e. biocompatibility, osseointegration, and osteoconduction. Granule morphology was identified as an important factor to ensure a good volume preservation.
Clinical relevance
Whereas both biomaterials showed excellent osteoconduction, SGs resulted in better volume preservation.









Similar content being viewed by others
References
Duncan RL, Turner CH (1995) Mechanotransduction and the functional response of bone to mechanical strain. Calcif Tissue Int 57:344–358. https://doi.org/10.1007/BF00302070
Araujo MG, Lindhe J (2005) Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32:212–218. https://doi.org/10.1111/j.1600-051X.2005.00642.x
Esposito M, Grusovin MG, Coulthard P, Worthington HV The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants 21:696–710
Greenwald AS, Boden SD, Goldberg VM, Khan Y, Laurencin CT, Rosier RN, American Academy of Orthopaedic Surgeons. The Committee on Biological Implants (2001) Bone-graft substitutes: facts, fictions, and applications. J Bone Jt Surg-Am Vol 83:98–103. https://doi.org/10.2106/00004623-200100022-00007
Zeugolis DI, Keeney M, Collin E, et al (2011) Xenogenic tissues and biomaterials for the skeletal system. In: Comprehensive Biomaterials. Elsevier, pp 387–404
Kunert-Keil C, Gredes T, Gedrange T (2011) Biomaterials applicable for alveolar sockets preservation: in vivo and in vitro studies. In: Implant Dentistry - The Most Promising Discipline of Dentistry. InTech
Precheur HV (2007) Bone graft materials. Dent Clin N Am 51:729–746. https://doi.org/10.1016/j.cden.2007.03.004
Ginebra M-P, Espanol M, Maazouz Y et al (2018) Bioceramics and bone healing. EFORT Open Rev 3:173–183. https://doi.org/10.1302/2058-5241.3.170056
Sadowska JM, Wei F, Guo J, Guillem-Marti J, Ginebra MP, Xiao Y (2018) Effect of nano-structural properties of biomimetic hydroxyapatite on osteoimmunomodulation. Biomaterials 181:318–332. https://doi.org/10.1016/j.biomaterials.2018.07.058
Barba A, Maazouz Y, Diez-Escudero A, Rappe K, Espanol M, Montufar EB, Öhman-Mägi C, Persson C, Fontecha P, Manzanares MC, Franch J, Ginebra MP (2018) Osteogenesis by foamed and 3D-printed nanostructured calcium phosphate scaffolds: effect of pore architecture. Acta Biomater 79:135–147. https://doi.org/10.1016/j.actbio.2018.09.003
Barba A, Diez-Escudero A, Maazouz Y, Rappe K, Espanol M, Montufar EB, Bonany M, Sadowska JM, Guillem-Marti J, Öhman-Mägi C, Persson C, Manzanares MC, Franch J, Ginebra MP (2017) Osteoinduction by foamed and 3D-printed calcium phosphate scaffolds: effect of nanostructure and pore architecture. ACS Appl Mater Interfaces 9:41722–41736. https://doi.org/10.1021/acsami.7b14175
Kirmeier R, Payer M, Wehrschuetz M, Jakse N, Platzer S, Lorenzoni M (2008) Evaluation of three-dimensional changes after sinus floor augmentation with different grafting materials. Clin Oral Implants Res 19:366–372. https://doi.org/10.1111/j.1600-0501.2007.01487.x
Mazzocco F, Lops D, Gobbato L et al (2014) Three-dimensional volume change of grafted bone in the maxillary sinus. Int J Oral Maxillofac Implants 29:178–184. https://doi.org/10.11607/jomi.3236
Schilling AF, Linhart W, Filke S, Gebauer M, Schinke T, Rueger JM, Amling M (2004) Resorbability of bone substitute biomaterials by human osteoclasts. Biomaterials 25:3963–3972. https://doi.org/10.1016/j.biomaterials.2003.10.079
Sadowska JM, Ginebra M-P (2020) Inflammation and biomaterials: role of the immune response in bone regeneration by inorganic scaffolds. J Mater Chem B 8:9404–9427. https://doi.org/10.1039/D0TB01379J
Thomas MV, Puleo DA (2011) Infection, inflammation, and bone regeneration: a paradoxical relationship. J Dent Res 90:1052–1061. https://doi.org/10.1177/0022034510393967
Hankenson KD, Dishowitz M, Gray C, Schenker M (2011) Angiogenesis in bone regeneration. Injury 42:556–561. https://doi.org/10.1016/j.injury.2011.03.035
Flautre B, Descamps M, Delecourt C, Blary MC, Hardouin P (2001) Porous HA ceramic for bone replacement: role of the pores and interconnections—experimental study in the rabbit. J Mater Sci Mater Med 12:679–682. https://doi.org/10.1023/A:1011256107282
Rustom LE, Boudou T, Nemke BW, Lu Y, Hoelzle DJ, Markel MD, Picart C, Wagoner Johnson AJ (2017) Multiscale porosity directs bone regeneration in biphasic calcium phosphate scaffolds. ACS Biomater Sci Eng 3:2768–2778. https://doi.org/10.1021/acsbiomaterials.6b00632
Hench LL, Wilson J (1993) An introduction to bioceramics. World Scientific Pub Co Inc
Hoornaert A, Maazouz Y, Pastorino D, Aparicio C, de Pinieux G, Fellah BH, Ginebra MP, Layrolle P (2019) Vertical bone regeneration with synthetic biomimetic calcium phosphate onto the calvaria of rats. Tissue Eng Part C Methods 25:1–11. https://doi.org/10.1089/ten.tec.2018.0260
Rissolo AR, Bennett J (1998) Bone grafting and its essential role in implant dentistry. Dent Clin N Am 42:91–116
Uchida Y, Goto M, Katsuki T, Soejima Y (1998) Measurement of maxillary sinus volume using computerized tomographic images. Int J Oral Maxillofac Implants 13:811–818
Doube M, Klosowski MM, Arganda-Carreras I et al (2010) BoneJ: Free and extensible bone image analysis in ImageJ. Bone 47:1076–1079. https://doi.org/10.1016/j.bone.2010.08.023
Pinheiro JC, Bates DM (2000) Mixed-effects models in S and S-PLUS. Springer-Verlag, New York
Bromage TG, Goldman HM, McFarlin SC et al (2003) Circularly polarized light standards for investigations of collagen fiber orientation in bone. Anat Rec 274B:157–168. https://doi.org/10.1002/ar.b.10031
Ginebra MP, Fernández E, De Maeyer EAP et al (1997) Setting reaction and hardening of an apatitic calcium phosphate cement. J Dent Res 76:905–912. https://doi.org/10.1177/00220345970760041201
Roveri N, Iafisco M (2010) Evolving application of biomimetic nanostructured hydroxyapatite. Nanotechnol Sci Appl 107. https://doi.org/10.2147/NSA.S9038
Jemt T, Lekholm U (2003) Measurements of Buccal tissue volumes at single-implant restorations after local bone grafting in maxillas: a 3-year clinical prospective study case series. Clin Implant Dent Relat Res 5:63–70. https://doi.org/10.1111/j.1708-8208.2003.tb00185.x
Oltramari PVP, de Lima NR, Henriques JFC et al (2007) Evaluation of bone height and bone density after tooth extraction: an experimental study in minipigs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104:e9–e16. https://doi.org/10.1016/j.tripleo.2007.06.015
Ruehe B, Niehues S, Heberer S, Nelson K (2009) Miniature pigs as an animal model for implant research: bone regeneration in critical-size defects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:699–706. https://doi.org/10.1016/j.tripleo.2009.06.037
Misch CE, Suzuki JB (2008) Tooth extraction, socket grafting, and barrier membrane bone regeneration. In: Contemporary Implant Dentistry, 3rd ed. pp 870–904
Li Y, Chen S-K, Li L, Qin L, Wang XL, Lai YX (2015) Bone defect animal models for testing efficacy of bone substitute biomaterials. J Orthop Transl 3:95–104. https://doi.org/10.1016/j.jot.2015.05.002
Wang S, Liu Y, Fang D, Shi S (2007) The miniature pig: a useful large animal model for dental and orofacial research. Oral Dis 13:530–537. https://doi.org/10.1111/j.1601-0825.2006.01337.x
Dasmah A, Thor A, Ekestubbe A, Sennerby L, Rasmusson L (2012) Particulate vs. block bone grafts: three-dimensional changes in graft volume after reconstruction of the atrophic maxilla, a 2-year radiographic follow-up. J Cranio-Maxillofac Surg 40:654–659. https://doi.org/10.1016/j.jcms.2011.10.032
Jensen T, Schou S, Svendsen PA, Forman JL, Gundersen HJG, Terheyden H, Holmstrup P (2012) Volumetric changes of the graft after maxillary sinus floor augmentation with Bio-Oss and autogenous bone in different ratios: a radiographic study in minipigs. Clin Oral Implants Res 23:902–910. https://doi.org/10.1111/j.1600-0501.2011.02245.x
Salem D, Alshihri A, Arguello E et al (2019) Volumetric analysis of allogeneic and xenogeneic bone substitutes used in maxillary sinus augmentations utilizing cone beam computed tomography: a prospective randomized pilot study. Int J Oral Maxillofac Implants 34:920–926. https://doi.org/10.11607/jomi.7318
Younes F, Cosyn J, De Bruyckere T et al (2019) A 2-year prospective case series on volumetric changes, PROMs, and clinical outcomes following sinus floor elevation using deproteinized bovine bone mineral as filling material. Clin Implant Dent Relat Res 21:301–309. https://doi.org/10.1111/cid.12730
Mordenfeld A, Hallman M, Johansson CB, Albrektsson T (2010) Histological and histomorphometrical analyses of biopsies harvested 11 years after maxillary sinus floor augmentation with deproteinized bovine and autogenous bone. Clin Oral Implants Res 961–970. https://doi.org/10.1111/j.1600-0501.2010.01939.x
Sakka S, Coulthard P (2009) Bone Quality: A reality for the process of osseointegration. Implant Dent 18:480–485. https://doi.org/10.1097/ID.0b013e3181bb840d
Rho J-Y, Kuhn-Spearing L, Zioupos P (1998) Mechanical properties and the hierarchical structure of bone. Med Eng Phys 20:92–102. https://doi.org/10.1016/S1350-4533(98)00007-1
Barba A, Diez-Escudero A, Espanol M, Bonany M, Sadowska JM, Guillem-Marti J, Öhman-Mägi C, Persson C, Manzanares MC, Franch J, Ginebra MP (2019) Impact of biomimicry in the design of osteoinductive bone substitutes: nanoscale matters. ACS Appl Mater Interfaces 11:8818–8830. https://doi.org/10.1021/acsami.8b20749
Cuzmar E, Perez RA, Manzanares M-C, Ginebra MP, Franch J (2015) In vivo osteogenic potential of biomimetic hydroxyapatite/collagen microspheres: comparison with injectable cement pastes. PLoS One 10:e0131188. https://doi.org/10.1371/journal.pone.0131188
Mai R, Reinstorf A, Pilling E, Hlawitschka M, Jung R, Gelinsky M, Schneider M, Loukota R, Pompe W, Eckelt U, Stadlinger B (2008) Histologic study of incorporation and resorption of a bone cement–collagen composite: an in vivo study in the minipig. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:e9–e14. https://doi.org/10.1016/j.tripleo.2007.09.016
Skoglund A, Hising P, Young C (1997) A clinical and histologic examination in humans of the osseous response to implanted natural bone mineral. Int J Oral Maxillofac Implants 12:194–199
Duda M, Pajak J (2004) The issue of bioresorption of the Bio-Oss xenogeneic bone substitute in bone defects. Ann Univ Mariae Curie Sklodowska Med 59(1):269–277
Schlegel A, Donath K (1998) BIO-OSS®—a resorbable bone substitute? J Long-Term Eff Med Implants 8(3–4):201–209
Hallman M, Cederlund A, Lindskog S, Lundgren S, Sennerby L (2001) A clinical histologic study of bovine hydroxyapatite in combination with autogenous bone and fibrin glue for maxillary sinus floor augmentation: results after 6 to 8 months of healing. Clin Oral Implants Res 12:135–143. https://doi.org/10.1034/j.1600-0501.2001.012002135.x
Tadjoedin ES, De Lange GL, Bronckers ALJJ et al (2003) Deproteinized cancellous bovine bone (Bio-Oss®) as bone substitute for sinus floor elevation. A retrospective, histomorphometrical study of five cases. J Clin Periodontol 30:261–270. https://doi.org/10.1034/j.1600-051X.2003.01099.x
Zaffe D, Leghissa GC, Pradelli J, Botticelli AR (2005) Histological study on sinus lift grafting by Fisiograft and Bio-Oss. J Mater Sci Mater Med 16:789–793. https://doi.org/10.1007/s10856-005-3574-5
McAllister BS, Margolin MD, Cogan AG, Buck D, Hollinger JO, Lynch SE (1999) Eighteen-month radiographic and histologic evaluation of sinus grafting with anorganic bovine bone in the chimpanzee. Int J Oral Maxillofac Implants 14:361–368
Sartori S, Silvestri M, Forni F, Icaro Cornaglia A, Tesei P, Cattaneo V (2003) Ten-year follow-up in a maxillary sinus augmentation using anorganic bovine bone (Bio-Oss). A case report with histomorphometric evaluation. Clin Oral Implants Res 14:369–372. https://doi.org/10.1034/j.1600-0501.2003.140316.x
Araújo MG, Carmagnola D, Berglundh T et al (2001) Orthodontic movement in bone defects augmented with Bio-Oss®. An experimental study in dogs. J Clin Periodontol 28:73–80. https://doi.org/10.1034/j.1600-051x.2001.280111.x
Rumpel E, Wolf E, Kauschke E, Bienengräber V, Bayerlein T, Gedrange T, Proff P (2006) The biodegradation of hydroxyapatite bone graft substitutes in vivo. Folia Morphol (Warsz) 65:43–48
Stein GS, Lian JB (1993) Molecular mechanisms mediating proliferation/differentiation interrelationships during progressive development of the osteoblast phenotype. Endocr Rev 14:424–442. https://doi.org/10.1210/edrv-14-4-424
Acknowledgements
Y.R. acknowledges the Spanish Government for the PhD grant DI-15-08184 and M.-P.G. the Generalitat de Catalunya for the ICREA Academia Award. The authors kindly acknowledge the collaboration of the Serveis Científico-Tècnics SEM Team of the University of Barcelona. The authors thank Christian Guirola for proofreading the text.
Funding
This study was supported by Mimetis Biometerials S.L., Barcelona, Spain.
Author information
Authors and Affiliations
Contributions
D.P. and Y.M. designed the study; I.G. performed the surgeries; Y.R. and M.O. processed the samples; Y.R., D.P., Y.M., M.O., and M-C.M. collected the data; Y.R., D.P., and M.-P.G. analysed the results and wrote the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was obtained from the Specipig Ethics Committee for Animal Experimentation (Specipig S.L., Barcelona, Spain).
ARRIVE guidelines
This study has been carried out in compliance with the ARRIVE guidelines for the reporting of in-vivo experiments in animal research. The ARRIVE checklist can be found in the supplementary information.
Conflict of interest
Y.R., D.P., Y.M., and M.-P. G. have an equity interest in Mimetis Biomaterials, S.L., a spin-off company of UPC that may potentially benefit from the research results displayed in the present work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raymond, Y., Pastorino, D., Ginebreda, I. et al. Computed tomography and histological evaluation of xenogenic and biomimetic bone grafts in three-wall alveolar defects in minipigs. Clin Oral Invest 25, 6695–6706 (2021). https://doi.org/10.1007/s00784-021-03956-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03956-y