Abstract
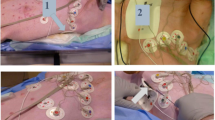
The presence of temporary myocardial pacing leads is considered a safety contraindication for magnetic resonance imaging (MRI). The aim of this ex vivo tissue study was to measure the heating effects at the tip of the leads using proton magnetic resonance spectroscopy (1HMRS) thermometry. The tissue effects were verified by histological analyses. Pig hearts with implanted temporary pacemaker myocardial pacing leads were examined by whole-body MRI at 1.5 Tesla. The tests were performed either by a sequence with high specific absorption rate (SAR) or by standard clinical sequences with lower SAR. Temperature changes were detected via 1HMRS thermometry, by monitoring the frequency difference between water protons and the reference signals of N-methyl protons of creatine/phosphocreatine (Cr/PCr) and trimethylamine (TMA). Histology was performed using several staining techniques. Standard low-SAR and high-SAR sequences did not cause significant temperature increases in the myocardial tissue surrounding the implanted leads. There were no histopathological signs of thermal damage around the tips of the leads in any of the hearts or in a control implanted heart not subjected to MRI. The present data suggest that temporary pacemaker myocardial pacing leads may be compatible with MR scanning at 1.5 Tesla. However, further in vivo studies and carefully monitored patient studies are needed before final safety recommendations can be made.




Similar content being viewed by others
Abbreviations
- 1HMRS:
-
Proton magnetic resonance spectroscopy
- Cr/PCr:
-
Creatine/phosphocreatine
- EPI:
-
Echo planar imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- HLSVD:
-
Hankel Lanczos squares singular values decomposition
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- Ppm:
-
Parts per million
- SAR:
-
Specific absorption rate
- TMA:
-
Trimethylamine
References
Newman MF, Mathew JP, Grocott HP, Mackensen GB, Monk T, Welsh-Bohmer KA, Blumenthal JA, Laskowitz DT, Mark DB (2006) Central nervous system injury associated with cardiac surgery. Lancet 368(9536):694–703
Grocott HP, Yoshitani K (2007) Neuroprotection during cardiac surgery. J Anesth 21(3):367–377
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C (1996) Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 335(25):1857–1863
Levine GN, Gomes AS, Arai AE, Bluemke DA, Flamm SD, Kanal E, Manning WJ, Martin ET, Smith JM, Wilke N, Shellock FS (2007) Safety of magnetic resonance imaging in patients with cardiovascular devices: an American Heart Association scientific statement from the Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Council on Cardiovascular Radiology and Intervention: endorsed by the American College of Cardiology Foundation, the North American Society for Cardiac Imaging, and the Society for Cardiovascular Magnetic Resonance. Circulation 116(24):2878–2891
Rezai AR, Phillips M, Baker KB, Sharan AD, Nyenhuis J, Tkach J, Henderson J, Shellock FG (2004) Neurostimulation system used for deep brain stimulation (DBS): MR safety issues and implications of failing to follow safety recommendations. Invest Radiol 39(5):300–303
Shellock FG, Crues JV (2004) MR procedures: biologic effects, safety, and patient care. Radiology 232(3):635–652
Achenbach S, Moshage W, Diem B, Bieberle T, Schibgilla V, Bachmann K (1997) Effects of magnetic resonance imaging on cardiac pacemakers and electrodes. Am Heart J 134(3):467–473
Gimbel J (2001) Implantable pacemaker and defibrillator safety in the MR environment: new thoughts for the new millennium. In: Special Cross-Specialty Categorical Course in Diagnostic Radiology: Practical MR Safety Considerations for Physicians, Physicists, and Technologists. Radiological Society of North America, Oak Lawn, pp 69–76
Duru F, Luechinger R, Scheidegger MB, Luscher TF, Boesiger P, Candinas R (2001) Pacing in magnetic resonance imaging environment: clinical and technical considerations on compatibility. Eur Heart J 22(2):113–124
Luechinger R, Duru F, Scheidegger MB, Boesiger P, Candinas R (2001) Force and torque effects of a 1.5-Tesla MRI scanner on cardiac pacemakers and ICDs. Pacing Clin Electrophysiol 24(2):199–205
Pavlicek W, Geisinger M, Castle L, Borkowski GP, Meaney TF, Bream BL, Gallagher JH (1983) The effects of nuclear magnetic resonance on patients with cardiac pacemakers. Radiology 147(1):149–153
Hayes DL, Holmes DR Jr, Gray JE (1987) Effect of 1.5 tesla nuclear magnetic resonance imaging scanner on implanted permanent pacemakers. J Am Coll Cardiol 10(4):782–786
Holmes DR Jr, Hayes DL, Gray JE, Merideth J (1986) The effects of magnetic resonance imaging on implantable pulse generators. Pacing Clin Electrophysiol 9(3):360–370
Fontaine JM, Mohamed FB, Gottlieb C, Callans DJ, Marchlinski FE (1998) Rapid ventricular pacing in a pacemaker patient undergoing magnetic resonance imaging. Pacing Clin Electrophysiol 21(6):1336–1339
Fetter J, Aram G, Holmes DR Jr, Gray JE, Hayes DL (1984) The effects of nuclear magnetic resonance imagers on external and implantable pulse generators. Pacing Clin Electrophysiol 7(4):720–727
Erlebacher JA, Cahill PT, Pannizzo F, Knowles RJ (1986) Effect of magnetic resonance imaging on DDD pacemakers. Am J Cardiol 57(6):437–440
Gimbel JR, Johnson D, Levine PA, Wilkoff BL (1996) Safe performance of magnetic resonance imaging on five patients with permanent cardiac pacemakers. Pacing Clin Electrophysiol 19(6):913–919
Nitz WR, Brinker G, Diehl D, Frese G (2005) Specific absorption rate as a poor indicator of magnetic resonance-related implant heating. Invest Radiol 40(12):773–776
Shellock FG, Cosendai G, Park SM, Nyenhuis JA (2004) Implantable microstimulator: magnetic resonance safety at 1.5 Tesla. Invest Radiol 39(10):591–599
Kuroda K, Oshio K, Chung AH, Hynynen K, Jolesz FA (1997) Temperature mapping using the water proton chemical shift: a chemical shift selective phase mapping method. Magn Reson Med 38(5):845–851
Cady EB, D’Souza PC, Penrice J, Lorek A (1995) The estimation of local brain temperature by in vivo 1H magnetic resonance spectroscopy. Magn Reson Med 33(6):862–867
Hitzig BM, Perng WC, Burt T, Okunieff P, Johnson DC (1994) 1H-NMR measurement of fractional dissociation of imidazole in intact animals. Am J Physiol 266(3 Pt 2):R1008–R1015
MacFall JR, Prescott DM, Charles HC, Samulski TV (1996) 1H MRI phase thermometry in vivo in canine brain, muscle, and tumor tissue. Med Phys 23(10):1775–1782
van den Boogaart A, van Ormondt D, Pijnappel WW, de Beer R, Ala-Korpela M (1994) Removal of the water resonance from1H-magnetic resonance spectra. In: McWhirter JG (ed) Mathematics in signal processing III. Clarendon Press, Oxford, pp 175–195
Watts AM, Tyler MP, Perry ME, Roberts AH, McGrouther DA (2001) Burn depth and its histological measurement. Burns 27(2):154–160
Haller H (2009) Verbrennungstiefe und Ausmaß. In: Kamolz LP, Herndon DN, Jeschke MG (eds) Verbrennungen. Springer, Wien, pp 159–160
Peters RD, Hinks RS, Henkelman RM (1998) Ex vivo tissue-type independence in proton-resonance frequency shift MR thermometry. Magn Reson Med 40(3):454–459
Kuroda K, Mulkern RV, Oshio K, Panych LP, Nakai T, Moriya T, Okuda S, Hynynen K, Jolesz FA (2000) Temperature mapping using the water proton chemical shift: self-referenced method with echo-planar spectroscopic imaging. Magn Reson Med 43(2):220–225
Zhu M, Bashir A, Ackerman JJ, Yablonskiy DA (2008) Improved calibration technique for in vivo proton MRS thermometry for brain temperature measurement. Magn Reson Med 60(3):536–541
Mulkern RV, Chung AH, Jolesz FA, Hynynen K (1997) Temperature monitoring of ultrasonically heated muscle with RARE chemical shift imaging. Med Phys 24(12):1899–1906
Kuroda K, Suzuki Y, Ishihara Y, Okamoto K (1996) Temperature mapping using water proton chemical shift obtained with 3D-MRSI: feasibility in vivo. Magn Reson Med 35(1):20–29
Sommer T, Vahlhaus C, Lauck G, von Smekal A, Reinke M, Hofer U, Block W, Traber F, Schneider C, Gieseke J, Jung W, Schild H (2000) MR imaging and cardiac pacemakers: in vitro evaluation and in vivo studies in 51 patients at 0.5 T. Radiology 215(3):869–879
Shellock FG, Shellock VJ (1998) Cardiovascular catheters and accessories: ex vivo testing of ferromagnetism, heating, and artifacts associated with MRI. J Magn Reson Imaging 8(6):1338–1342
Finelli DA, Rezai AR, Ruggieri PM, Tkach JA, Nyenhuis JA, Hrdlicka G, Sharan A, Gonzalez-Martinez J, Stypulkowski PH, Shellock FG (2002) MR imaging-related heating of deep brain stimulation electrodes: in vitro study. AJNR Am J Neuroradiol 23(10):1795–1802
Mattei E, Triventi M, Calcagnini G, Censi F, Kainz W, Mendoza G, Bassen HI, Bartolini P (2008) Complexity of MRI induced heating on metallic leads: experimental measurements of 374 configurations. Biomed Eng Online 7:11
Acknowledgments
The authors thank Dr. Nicola M. Osypka (managing and sales director, Dr. Osypka GmbH, Germany) for the use of the temporary pacemaker myocardial pacing leads; Rüdiger Vollandt, PhD, for statistical advice; and Dr. Ernesta Palombo-Kinne for critical revision of the manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pfeil, A., Drobnik, S., Rzanny, R. et al. Compatibility of temporary pacemaker myocardial pacing leads with magnetic resonance imaging: an ex vivo tissue study. Int J Cardiovasc Imaging 28, 317–326 (2012). https://doi.org/10.1007/s10554-011-9800-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-011-9800-y