Abstract
This review aims to evaluate the current literature on the procedural costs of bariatric surgery for the treatment of severe obesity. Using a published framework for the conduct of micro-costing studies for surgical interventions, existing cost estimates from the literature are assessed for their accuracy, reliability and comprehensiveness based on their consideration of seven ‘important’ cost components. MEDLINE, PubMed, key journals and reference lists of included studies were searched up to January 2017. Eligible studies had to report per-case, total procedural costs for any type of bariatric surgery broken down into two or more individual cost components. A total of 998 citations were screened, of which 13 studies were included for analysis. Included studies were mainly conducted from a US hospital perspective, assessed either gastric bypass or adjustable gastric banding procedures and considered a range of different cost components. The mean total procedural costs for all included studies was US$14,389 (range, US$7423 to US$33,541). No study considered all of the recommended ‘important’ cost components and estimation methods were poorly reported. The accuracy, reliability and comprehensiveness of the existing cost estimates are, therefore, questionable. There is a need for a comparative cost analysis of the different approaches to bariatric surgery, with the most appropriate costing approach identified to be micro-costing methods. Such an analysis will not only be useful in estimating the relative cost-effectiveness of different surgeries but will also ensure appropriate reimbursement and budgeting by healthcare payers to ensure barriers to access this effective treatment by severely obese patients are minimised.
Similar content being viewed by others
Introduction
Bariatric surgery is considered the most efficacious treatment for severe and complex obesity [1] and can be performed using a number of different surgical techniques. In 2013, Roux-en-Y gastric bypass (RYGB) was the most common procedure, followed by sleeve gastrectomy (SG) and adjustable gastric banding (AGB), accounting for 45, 37 and 10% of surgeries performed respectively worldwide [2]. Recently, however, SG has surpassed RYGB as the most common procedure in some jurisdictions, with SG accounting for over 50% of bariatric surgeries performed in the USA [3].
Evidence from retrospective studies suggest that RYGB and SG are likely to result in the greatest amount of weight loss and improvement of comorbidities, but have greater risks and less flexibility than AGB, which is associated with less reliable long-term weight loss [4]. However, evidence from randomised controlled trials comparing the different surgeries is limited [5, 6], as is information on the relative cost-effectiveness of the three surgery types [7]. The lack of the latter evidence could be due partly to a dearth of cost information for the three procedures. Detailed cost estimates (i.e. expenditures involved in acquiring resources that are necessary for the delivery of care) are also a requisite for the development of appropriate reimbursement rates by healthcare payers [8]. For example, the National Health Service (NHS) in the UK has two main tariffs used to reimburse physicians/hospitals for performing bariatric surgery [£4028 (US$5771) for AGB and SG and £4608 (US$6602) for RYGB] [9]. However, the underlying resources and costs attributed to these tariffs are unclear, which could lead to either over- or underpayment of providers of bariatric surgery.
To fill these evidence gaps, a multi-centre randomised controlled trial, known as the By-Band-Sleeve (BBS) study, is being conducted comparing both the relative effectiveness and cost-effectiveness of RYGB, AGB and SG [5, 10]. In comparison to other bariatric surgery trials, the BBS study will assess both clinical and economic outcomes for the three most common approaches to bariatric surgery, in the largest sample size studied in a comparative trial to date (expected to randomise 447 patients per group), over a substantial follow-up period (36 months). However, an important first step in estimating the economic outcomes in the BBS study will be to obtain detailed and ‘accurate’ costs of the three types of bariatric surgery.
The costs associated with bariatric surgery are a function of the resources consumed and the unit costs associated with those resources. These parameters can be identified using a number of different approaches, but can broadly be separated into methods used to identify cost components (gross costing or micro-costing) [11] and methods used to value cost components (top-down costing and bottom-up costing) (see Box 1 for definitions) [12]. The choice of method is usually dependent on the context, data and funding available to conduct a costing study, but it is important to note that the application of different methods may result in variations in the magnitude and therefore the accuracy and reliability of the estimated costs [13, 14]. Detailed cost estimates, derived using transparent methods, are not only important to provide appropriate reimbursement but also act as accurate inputs in analyses comparing the relative cost-effectiveness of the different surgical approaches and will allow healthcare providers to budget judiciously, potentially minimising barriers to access surgery for the increasing number of severely obese patients [15]. Therefore, our study aimed to review the literature and identify robust estimates of the procedural costs of the main types of bariatric surgery. More specifically, we will summarise the international literature on procedural bariatric surgery costs and assess their comprehensiveness, accuracy and reliability.
Methods
Eligibility Criteria
Published costing studies in the English language reporting detailed, per-case (i.e. per-patient) cost estimates associated with performing any type of bariatric surgery were considered. To be included, a cost analysis had to report two or more cost components related to performing the procedure. For example, a study reporting a breakdown of the total cost of surgery in terms of inpatient stay, personnel and equipment costs would be included in the review. Studies only reporting the total cost of surgery with no breakdown into individual cost components (i.e. an aggregated cost) were excluded because it is impossible to understand from total costs what underlying resources were included. Studies only reporting detailed total costs for a single component (e.g. equipment costs) were also excluded, even if they broke down the single component into sub-components (e.g. total equipment costs broken down into maintenance costs, operating costs and personnel costs for cleaning). Studies only assessing the cost of healthcare utilisation either before or after bariatric surgery were also excluded.
Information Sources, Search and Data Collection
Two databases, Ovid MEDLINE and PubMed, were searched from inception to January 16, 2017 (Appendix). Search terms were initially developed for three different categories, costing terminology, types of bariatric surgery and obesity nomenclature, but subsequently refined to increase the sensitivity of the searches. No restrictions were initially placed on the language of the articles to ensure a large number of relevant studies were not published in languages other than English, but any studies not reported in English were excluded from the review during screening. In addition, a hand search of key journals and the quoted references from the included articles was conducted to identify any additional studies. One author (B.D.) screened the titles and abstracts of all the citations identified from the search strategies, reviewed the full-text articles identified after screening and extracted the data from all included studies.
Data Items
Study design and population, types of bariatric surgery assessed, data collection methods and types of costs (i.e. cost components) included were extracted. Total costs of the procedure were extracted as well as the cost values associated with each individual component. Costs are reported here in the currency and price year originally listed in the included study. When the price year was not reported, it was assumed that the price year would be 1 year earlier than the year in which the study was published. To compare the cost of bariatric surgery between different studies, total procedural costs were also inflated to a 2016 price year. When prices were reported over multiple years, the most recent price year was used to inflate the total cost to make a conservative assumption. In terms of currency conversion for studies conducted in different countries, costs were adjusted for purchasing power parities (PPPs) (to adjust for price differences between countries, rather than just exchange rates, which do not take price differences into account) and converted to 2016 US dollar PPPs [16]. If total costs were reported in US dollars, but had been converted from the country’s currency in which the study was conducted, the total cost estimate was first converted back to the original currency using the exchange rate provided in the article before inflating, adjusting and converting to 2016 US dollars.
Assessment of Accuracy, Reliability and Comprehensiveness
To provide an indication of the accuracy, reliability and comprehensiveness of the reported cost estimates, the inclusion of ‘important’ cost components based on criteria outlined by Ismail et al. [17] for conducting costing analyses of surgical interventions was assessed. Ismail et al. reviewed costing approaches for robotic surgeries, in general, and assessed 19 studies, three of which related to bariatric surgery [18,19,20], for their consideration of six criteria with the objective to create and validate a micro-costing methodology that could be used by surgeons and hospital administrators to evaluate the cost of implementing new surgical approaches. As standardised guidance regarding how to conduct a micro-costing is limited [21, 22], the methodology presented by Ismail et al. provides one of the only frameworks for the conduct of micro-costing studies and has specifically been designed for the evaluation of surgical interventions. The consideration of the six criteria presented by Ismail et al. was therefore thought to form a standard by which existing cost analyses could be measured. We have, however, also added an additional criterion (inclusion of overhead costs) to the six originally presented by Ismail et al. [17] as exclusion of such overheads could also affect the accuracy, reliability and comprehensiveness of cost estimates reported in the literature. A study was considered to include one of the ‘important’ cost components when a separate cost value could be identified for that individual component. The seven ‘important’ cost components included:
-
1.
Cost, not charge data used in the analysis;
-
2.
Operating room costs reported separate from hospital admission costs;
-
3.
Medical device costs reported (e.g. endoscopy column, laparoscopic tower);
-
4.
Personnel costs reported (e.g. surgeon, nurse, anaesthesiologist time);
-
5.
Re-usable instrument costs reported (e.g. bowel graspers, surgical scissors);
-
6.
Disposable instrument/consumables costs reported (e.g. needles, disposable staplers); and
-
7.
Overhead costs reported.
Reporting of the methods used to identify cost components (gross and/or micro-costing) and value cost components (top-down and/or bottom-up costing) was appraised. When methods were not specifically reported, we assigned the relevant method based on the reported data collection description for resource items and costs. The inclusion of specific parameters based on standardised formulas [17] in the calculation of ‘important’ cost components (e.g. medical devices, personnel, re-usable and disposable instruments) was also evaluated. The parameters of interest included:
-
1.
Capacity adjustment of personnel costs (e.g. adjusting salary for working days minus paid leave when determining a per-minute personnel cost);
-
2.
Amortisation or depreciation of medical devices (e.g. allocating the acquisition cost of a device over its useful lifespan);
-
3.
Maintenance fees for medical devices (in addition to the amortised acquisition cost);
-
4.
Adjustments for medical devices shared across different procedures (i.e. laparoscopic tower may only be used 50% of the time for bariatric surgery);
-
5.
Sterilisation costs of reusable instruments (e.g. personnel time disinfecting and repackaging reusable instruments); and
-
6.
Disposal costs of consumables (e.g. the waste management costs associated with consumables).
Synthesis of Results
Syntheses of the extracted data were performed to compare study characteristics and cost estimates across studies as well as combine individual study cost estimates into summary measures of total procedural costs. Important study characteristics and detailed cost estimates from the included studies were summarised in tabular format and used to evaluate the availability of cost estimates for different types of bariatric surgery, the methods used to collect the cost data and the specific cost components included in the analyses. Mean costs and standard deviations (SD) were calculated for all reported cost estimates together, estimates derived only from cost data (as charges do not necessarily reflect the actual cost of the resources consumed to deliver the surgery) and for different types of bariatric surgery. The inclusion of ‘important’ cost components was also synthesised in tabular format.
Results
Study Selection
The search strategy identified a total of 998 citations. After removing duplicates (n = 499), 499 unique citations remained for title and abstract screening, which left 73 unique citations of interest for full-text review. After full-text review, 13 studies were selected for detailed review (Fig. 1).
Study Characteristics
Thirteen studies (Table 1) reported detailed procedural costs [17, 18, 23,24,25,26,27,28,29,30,31,32,33]. The majority of the studies were conducted from a US hospital perspective [23, 26,27,28,29,30, 32, 33], with the remaining studies taking a European [17, 18, 31], Australian [25] and Brazilian [24] hospital perspective. Limited details concerning the sources of data were provided in all the studies. Most commonly, data sources were simply stated as specific hospital departments or general hospital databases [17, 24, 28,29,30]. Other sources of data included hospital charges or claims data [23, 27, 32, 33], purchase prices [31], a dedicated bariatric surgery database [26], patient case record forms [25] and a mix of prospective, retrospective, documentation and finance department data [18].
A number of different types of bariatric surgery were costed, but no study assessed the cost of the SG procedure, perhaps as this is a relatively new procedure. One study reported costs for bariatric surgery, in general [32], two studies reported costs for different gastric banding procedures [25, 31] and two studies reported costs for gastric bypass procedures [17, 24]. The remaining studies compared the costs of two or more different procedures [18, 23, 26,27,28,29,30, 33].
Most studies included hospitalisation costs [18, 23, 24, 30,31,32,33] and/or the costs of consumables/materials/supplies [17, 18, 24,25,26,27, 30, 33]. Five studies reported costs associated with operating room time [18, 24, 26, 27, 30], personnel/staff costs [17, 23, 25, 29, 32] (note that only three of these studies [23, 25, 32] explicitly stated that surgeon/physician fees were included in personnel/staff costs) and/or the costs of additional procedures [23, 24, 29,30,31]. Four studies reported costs associated with a special instrument or technology [17, 18, 26, 27]. Three studies reported the cost of medications [23, 24, 29] and/or a combined cost associated with the operating room, including operating room time, supplies, personnel, equipment, medications and examinations [28, 29, 31]. A few studies also reported intensive care unit/post-anaesthesia costs [18, 29], indirect costs (e.g. overhead, housekeeping, administrative costs, etc.) [28, 29], anaesthesiology costs [33] and other miscellaneous costs [30].
Twenty-three total procedural cost estimates were reported in the 13 included studies, with a mean of $14,389 SD $6110 (range, $7423 to $33,541) (Table 2). Excluding the five studies that used charge data to estimate total procedural costs left 14 estimates with a mean of $13,993 SD $5441. Five studies reported ten estimates of total procedural costs for different types of gastric bypass procedures with a mean of $13,496 SD $4171. Three studies reported four estimates of total procedural costs for different types of gastric banding procedures, with a mean of $15,237 SD $8556.
Inclusion of ‘Important’ Cost Components
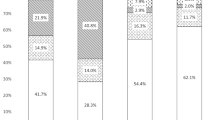
The majority of studies used cost [17, 18, 24,25,26, 28, 29, 31] rather than charge data [23, 27, 32] in their analyses, with two studies [30, 33] using both (Table 3). All the studies using cost data reported operating room costs separate from hospital admission costs, while only two [27, 30] of the four studies using charge data reported these two costs separately. The remaining five ‘important’ cost components (medical device, personnel, re-usable instruments, disposable instruments and overhead costs) varied in their reporting. Nine studies reported costs for instruments [17, 18, 24,25,26,27, 29, 30, 33], but usually did not differentiate between re-usable and disposable [18, 24, 25, 29, 30]. Only four studies [17, 18, 25, 29] included five or more of the seven important cost components in their analyses.
Methods and Parameters Used for Calculating ‘Important’ Cost Components
Only one study made specific reference to a method for identifying cost components [17]. Micro-costing methods were assumed to be most commonly employed to identify cost components, but methods of valuing components were not discernible in the majority of the studies. The inclusion of specific parameters in the calculation of ‘important’ cost components was also poorly reported. Only three studies amortised the cost [17, 18] or accounted for depreciation [26] of medical devices over their life span and only two studies accounted for the cost of maintenance fees [17, 18]. One of the studies reporting a combined operating room cost also noted that the laparoscopic equipment costs were amortised [29]. Only one study reported capacity adjusted personnel costs and accounted for sterilisation costs of reusable instruments [17]. No studies made adjustments for medical devices shared across different procedures or included the disposal costs associated with consumables.
Discussion
This paper presented a systematic review of cost analyses of a number of different approaches to bariatric surgery for the treatment of severe obesity. From the 13 studies included in the review, sources and methods of data collection were minimally reported, making it difficult to ascertain what methods were used to identify and value cost components. A number of different types of bariatric surgery were costed mainly from a US hospital perspective, including laparoscopic gastric bypass and gastric banding procedures, but no study reported a cost for the SG procedure. Some of the reported cost estimates were, however, for open procedures, procedures not commonly performed (e.g. vertical banded gastroplasty) or surgical techniques likely to be limited to certain providers (e.g. robot-assisted surgeries). This limits the generalisability and usefulness of the reported cost estimates for decision-making purposes as the majority of bariatric surgeries, worldwide, are performed laparoscopically using either the RYGB or SG procedure [2].
The inclusion of individual cost components in the total cost estimates varied widely, although the majority of the studies included hospitalisation and consumables/material/supply costs. Interestingly, only three studies explicitly considered surgeon/physician fees, despite the potential for these costs to drive differences in total procedural costs between the three procedures. Consideration of surgeon/physician fees in any future analyses will therefore be important, especially for comparing cost estimates between RYGB and SG where equipment/instrument costs could be quite similar. The variation in included cost components can potentially be explained by the lack of a clearly defined care cycle or timeframe in which resource use and costs were measured for the majority of studies (only two studies defined a care cycle [23, 30]), making it difficult to determine what cost components should be included.
Mean total procedural costs ranged from US$13,307 to US$15,237 depending on the types of studies included in the calculation. Excluding studies using charge data resulted in a lower mean total procedural cost (US$13,993 vs. US$14,389) and mean total procedural costs were observed to be lower for gastric bypass compared to gastric banding procedures (US$13,496 vs. US$15,237). These differences should, however, be interpreted with slight caution as these mean estimates are based on a small number of studies conducted in a number of different countries/settings and for a range of different procedures (e.g., open, laparoscopic and robot-assisted). In comparison to the UK tariffs for bariatric surgery, the mean estimates reported in the literature are much larger [e.g. £4608 (US$6602) for ‘Stomach bypass procedures for obesity—HRG code FZ84Z’ and £4,028 (US$5,771) for ‘Restrictive stomach procedures for obesity—HRG code FZ85Z’]. The basis of the UK tariffs is, however, unknown and their use as a relevant indicator of the accuracy of the costs of bariatric surgery reported in our review may not be appropriate.
Overall, most studies in the review did not report accurate, reliable and comprehensive estimates of the total procedural costs as the inclusion of the ‘important’ costs components based on recommended costing methods for surgical procedures was poor, with no study including all of the components. Calculation methods were also poorly reported and usually did not account for recommended parameters when estimating costs. This is not surprising as detailed cost information for interventions is lacking in many clinical areas.
Systematic reviews of costing studies of bariatric surgery are limited in the published literature. One relevant study was identified that reviewed cost approaches for robotic surgeries, in general [17], and despite the limited overlap in included studies, our review came to a similar conclusion, namely that costing studies related to surgical procedures (or specifically bariatric surgery) have not reported their methods transparently and largely do not consider ‘important’ cost components and parameters required for their estimation.
Furthermore, we have attempted to extract details of the reporting of specific parameters that would be required to generate appropriate cost estimates according to the formulas presented by Ismail et al. [17]. Just because a cost component has been included in an analysis does not mean that parameters required to estimate accurate, reliable and comprehensive costs have been considered. This point is highlighted in our review as even when important cost components were included, the methods and parameters used in their calculation were infrequently reported. Our review has also identified some additional criteria that should be reported to help improve the quality of cost estimates for bariatric surgery. Transparent reporting of the methods of identifying and valuing cost components should be provided, as the choice of method can have an impact on the magnitude of the cost estimates [13, 14]. An explicit care cycle definition should also be provided, especially to differentiate between cost estimates that have and have not included costs that are incurred before and/or after the actual conduct of the procedure, such as the costs of nutritional and psychological evaluations, 6 to 12 months of medical weight management, re-admissions, postoperative complications, routine vitamin supplements and laboratory testing for the life of the patient after surgery. These additional costs may be significant, but from the available literature, it is not clear if such costs were considered due to the lack of care cycle definitions.
Our study does, however, have limitations. First, detailed costings of bariatric surgery may have been conducted by certain healthcare providers, but not available in the literature. This is possibly due to the inclusion of sensitive pricing information (e.g. discounts negotiated with manufacturers of certain equipment) and, therefore, unlikely to be publically available.
Furthermore, our review only identified a small number of studies, with the majority conducted in a US hospital context. This makes it difficult to generalise the results of our study to other settings/jurisdictions, as different equipment, materials and personnel may be involved across different sites and countries. Caution should, therefore, be made when interpreting the mean cost estimates presented in our review in a local context.
Overall, our review indicates that there is a need for up-to-date costings of the three most common bariatric procedures (RYGB, AGB and SG). To ensure these costs are collected in a consistent manner, micro-costing methods have been identified as the most appropriate approach. We plan to conduct such a micro-costing study across a number of hospitals offering bariatric surgery within the NHS in England as part of the BBS study [5, 10]. Our study has been designed to consider all the ‘important’ cost components outlined in this review, will report the parameters involved in their calculation in a transparent manner and explicitly define the cycle of care to ensure inclusion of all relevant cost components. We will, therefore, be able to determine accurate, reliable and comprehensive estimates of the cost of bariatric surgery.
Change history
09 June 2017
An erratum to this article has been published.
References
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25(10):1822–32.
American Society for Metabolic and Bariatric Surgery (ASMBS). Estimate of Bariatric Surgery Numbers, 2011–2015. Gainesville, FL: ASMBS; July 2016 [May 4, 2017]; Available from: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers.
Farrell TM, Haggerty SP, Overby DW, et al. Clinical application of laparoscopic bariatric surgery: an evidence-based review. Surg Endosc. 2009;23(5):930–49.
Rogers CA, Welbourn R, Byrne J, et al. The by-band study: gastric bypass or adjustable gastric band surgery to treat morbid obesity: study protocol for a multi-centre randomised controlled trial with an internal pilot phase. Trials. 2014;15:53.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13(41):1–190. 215-357
Padwal R, Klarenbach S, Wiebe N, et al. Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med. 2011;26(10):1183–94.
Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22(4):233–6.
National Health Service (NHS) England and NHS Improvement. 2017/18 and 2018/19 National Tariff Payment System. London: NHS; December 2016.
Rogers CA, Reeves BC, Byrne J, Donovan JL, Mazza G, Paramasivan S, et al. Adaptation of the By-Band randomised controlled trial to By-Band-Sleeve to include a new intervention and to maintain relevance of the study to practice. British Journal of Surgery. 2017;In press.
Gold MR, Siegel JE, Russell LB, et al. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996.
Chapko MK, Liu CF, Perkins M, et al. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009;18(10):1188–201.
Clement Nee Shrive FM, Ghali WA, Donaldson C, et al. The impact of using different costing methods on the results of an economic evaluation of cardiac care: microcosting vs gross-costing approaches. Health Econ. 2009;18(4):377–88.
Tan SS, Rutten FF, van Ineveld BM, et al. Comparing methodologies for the cost estimation of hospital services. The European journal of health economics : HEPAC : health economics in prevention and care. 2009;10(1):39–45.
Welbourn R, le Roux CW, Owen-Smith A, et al. Why the NHS should do more bariatric surgery; how much should we do? BMJ. 2016;353:i1472.
Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evid Policy. 2010;6(1):51–9. WOS:000289188900004. English
Ismail I, Wolff S, Gronfier A, et al. A cost evaluation methodology for surgical technologies. Surg Endosc. 2015;29(8):2423–32.
Hagen ME, Pugin F, Chassot G, et al. Reducing cost of surgery by avoiding complications: the model of robotic roux-en-Y gastric bypass. Obes Surg. 2012;22(1):52–61.
Hubens G, Balliu L, Ruppert M, et al. Roux-en-Y gastric bypass procedure performed with the da Vinci robot system: is it worth it? Surg Endosc. 2008;22(7):1690–6.
Park CW, Lam EC, Walsh TM, et al. Robotic-assisted roux-en-Y gastric bypass performed in a community hospital setting: the future of bariatric surgery? Surg Endosc. 2011;25(10):3312–21.
Frick KD. Microcosting quantity data collection methods. Med Care. 2009;47(7 Suppl 1):S76–81.
Xu X, Grossetta Nardini HK, Ruger JP. Micro-costing studies in the health and medical literature: protocol for a systematic review. Systematic reviews. 2014;3:47.
Weiner JP, Goodwin SM, Chang HY, et al. Impact of bariatric surgery on health care costs of obese persons: a 6-year follow-up of surgical and comparison cohorts using health plan data. JAMA surgery. 2013;148(6):555–62.
Salgado Júnior W, Pitanga KC, et al. Costs of bariatric surgery in a teaching hospital and the financing provided by the public unified health system. Acta Cirurgica Brasileira. 2010;25(2):201–5.
Keating CL, Dixon JB, Moodie ML, et al. Cost-efficacy of surgically induced weight loss for the management of type 2 diabetes: a randomized controlled trial. Diabetes Care. 2009;32(4):580–4.
Ayloo SM, Buchs NC, Addeo P, et al. Traditional versus single-site placement of adjustable gastric banding: a comparative study and cost analysis. Obes Surg. 2011;21(7):815–9.
Muhlmann G, Klaus A, Kirchmayr W, et al. DaVinci robotic-assisted laparoscopic bariatric surgery: is it justified in a routine setting? Obes Surg. 2003;13(6):848–54.
Angus LD, Cottam DR, Gorecki PJ, et al. DRG, costs and reimbursement following roux-en-Y gastric bypass: an economic appraisal. Obes Surg. 2003;13(4):591–5.
Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279–89. discussion 89-91
Cooney RN, Bryant P, Haluck R, et al. The impact of a clinical pathway for gastric bypass surgery on resource utilization. J Surg Res. 2001;98(2):97–101.
van Gemert WG, Adang EM, Kop M, et al. A prospective cost-effectiveness analysis of vertical banded gastroplasty for the treatment of morbid obesity. Obes Surg. 1999;9(5):484–91.
Scally CP, Shih T, Thumma JR, et al. Impact of a National Bariatric Surgery Center of excellence program on Medicare expenditures. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2016;20(4):708–14.
Frezza EE, Wachtel MS, Ewing BT. Bariatric surgery costs and implications for hospital margins: comparing laparoscopic gastric bypass and laparoscopic gastric banding. Surgical laparoscopy, endoscopy & percutaneous techniques. 2007;17(4):239–44.
Edbrooke D, Hibbert C, Ridley S, et al. The development of a method for comparative costing of individual intensive care units. The Intensive Care Working Group on Costing. Anaesthesia. 1999;54(2):110–20.
Acknowledgements
This study is funded by The National Institute for Health Research Health Technology Assessment (NIHR HTA) programme (project number 09/127/53). The views and opinions expressed are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, the UK National Health Service or the Department of Health. J.M.B. is a NIHR Senior Investigator.
By-Band-Sleeve Trial Management Group: Jane Blazeby (Chief Investigator), University of Bristol; Richard Welbourn (Surgical Lead), Musgrove Park Hospital; James Byrne (Surgical Expertise), Southampton University Hospitals NHS Trust; Barnaby C. Reeves (Methodologist Lead), University of Bristol; Sarah Wordsworth (Health Economics Lead), University of Oxford; Robert C. Andrews (Endocrinology Lead), University of Exeter; Janice L. Thompson (Nutritional Lead), University of Birmingham; Graziella Mazza (Trial Manager), University of Bristol; Chris A. Rogers (Statistical Lead), University of Bristol.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
R.W. declares receiving support from Ethicon Endo-Surgery for attending conferences and funding a Bariatric Clinical Fellow at their hospital as well as receiving honoraria from Novo Nordisk.
The other authors declare that they have no conflict of interest, except support from a government grant as detailed in the acknowledgements.
Ethical Approval
For this study, formal consent is not required, as it is a review of the literature.
Informed Consent
Does not apply.
Additional information
The original version of this article was revised because of an error in the author group.
An erratum to this article is available at https://doi.org/10.1007/s11695-017-2768-5.
Appendix
Appendix
SEARCH STRATEGY FOR TARGETED LITERATURE REVIEW
Database: Epub Ahead of Print, In-process and Other Non-Indexed Citations, Ovid MEDLINER(R) 1946 to Present.
Date of search: 22/11/2016
-
1.
exp. “costs and cost analysis”/ or exp health care costs/ or exp health expenditures/ or exp hospital costs/
-
2.
bottom-up.ab,hw,kf,kw,ot,sh,ti,tw.
-
3.
1 and 2
-
4.
(microcost$ or micro-cost$).ab,hw,kf,kw,ot,sh,ti,tw.
-
5.
(bottom-up adj5 cost$).ab,hw,kf,kw,ot,sh,ti,tw.
-
6.
(bottom-up adj5 accounting).ab,hw,kf,kw,ot,sh,ti,tw.
-
7.
(activity-based adj5 accounting).ab,hw,kf,kw,ot,sh,ti,tw.
-
8.
(activity-based adj5 cost$).ab,hw,kf,kw,ot,sh,ti,tw.
-
9.
3 or 4 or 5 or 6 or 7
-
10.
time study.ab,hw,kf,kw,ot,sh,ti,tw.
-
11.
time motion study.ab,hw,kf,kw,ot,sh,ti,tw.
-
12.
(time and motion method).ab,hw,kf,kw,ot,sh,ti,tw.
-
13.
time-and-motion method.ab,hw,kf,kw,ot,sh,ti,tw.
-
14.
(time and motion study).ab,hw,kf,kw,ot,sh,ti,tw.
-
15.
time-and-motion study.ab,hw,kf,kw,ot,sh,ti,tw.
-
16.
time motion analysis.ab,hw,kf,kw,ot,sh,ti,tw.
-
17.
9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
-
18.
exp bariatric surgery/ or exp gastric bypass/ or exp jejunoileal bypass/ or exp anastomosis, roux-en-y/ or exp gastroenterostomy/ or exp gastrostomy/
-
19.
gastric bypass.ab,hw,kf,kw,ot,sh,ti,tw.
-
20.
adjustable gastric banding.ab,hw,kf,kw,ot,sh,ti,tw.
-
21.
gastric banding.ab,hw,kf,kw,ot,sh,ti,tw.
-
22.
sleeve gastrectomy.ab,hw,kf,kw,ot,sh,ti,tw.
-
23.
(Roux-en-Y adj5 gastric bypass).ab,hw,kf,kw,ot,sh,ti,tw.
-
24.
bariatric surgery.ab,hw,kf,kw,ot,sh,ti,tw.
-
25.
metabolic surgery.ab,hw,kf,kw,ot,sh,ti,tw.
-
26.
weight-loss surgery.ab,hw,kf,kw,ot,sh,ti,tw.
-
27.
digestive surgery.ab,hw,kf,kw,ot,sh,ti,tw.
-
28.
18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27
-
29.
exp obesity/ or exp obesity, morbid/
-
30.
(obesity adj5 severe).ab,hw,kf,kw,ot,sh,ti,tw.
-
31.
(obesity adj5 complex).ab,hw,kf,kw,ot,sh,ti,tw.
-
32.
morbid obes$.ab,hw,kf,kw,ot,sh,ti,tw.
-
33.
weight-loss.ab,hw,kf,kw,ot,sh,ti,tw.
-
34.
29 or 30 or 31 or 32 or 33
-
35.
9 and 28—Total hits 1
-
36.
9 or 17
-
37.
28 and 36—Total hits 2
-
38.
1 and 28 and 34—Total hits 327
-
39.
1 and 28—Total hits 499
-
40.
1 and 28—Update 26/12/2016 Total hits 16
-
41.
1 and 28—Update 02/01/2017 Total hits 3
-
42.
1 and 28—Update 09/01/2017 Total hits 8
-
43.
1 and 28—Update 16/01/2017 Total hits 3
Database: PubMed.
Date of search: 22/11/2016
-
1.
((((((costs and cost analysis[MeSH Terms])) OR costs, cost analysis[MeSH Terms]) OR costs, health care[MeSH Terms]) OR costs, hospital[MeSH Terms]) OR costs, treatment[MeSH Terms]) OR health expenditures[MeSH Terms]
-
2.
bottom-up[Title/Abstract]
-
3.
1 and 2
-
4.
(microcosting[Title/Abstract]) OR micro-costing[Title/Abstract]
-
5.
bottom-up costing[Title/Abstract]
-
6.
bottom-up accounting[Title/Abstract]
-
7.
activity-based accounting[Title/Abstract]
-
8.
activity-based costing[Title/Abstract]
-
9.
3 or 4 or 5 or 6 or 7 or 8
-
10.
(time and motion studies[MeSH Terms])
-
11.
time study[Title/Abstract]
-
12.
time motion study[Title/Abstract]
-
13.
time-and-motion method[Title/Abstract]
-
14.
time-and-motion study[Title/Abstract]
-
15.
time motion analysis[Title/Abstract]
-
16.
10 or 11 or 12 or 13 or 14 or 15
-
17.
((((((((((bariatric surgery[MeSH Terms]) OR surgeries, bariatric[MeSH Terms]) OR gastric bypass[MeSH Terms]) OR gastric bypass, greenville[MeSH Terms]) OR gastric bypass, roux en y[MeSH Terms]) OR bypass, jejunoileal[MeSH Terms]) OR anastomosis, roux en y[MeSH Terms]) OR diversion, roux en y[MeSH Terms]) OR loop, roux en y[MeSH Terms]) OR gastroenterostomy[MeSH Terms]) OR gastrostomy[MeSH Terms]
-
18.
gastric bypass[Title/Abstract]
-
19.
adjustable gastric banding[Title/Abstract]
-
20.
gastric banding[Title/Abstract]
-
21.
sleeve gastrectomy[Title/Abstract]
-
22.
roux-en-y gastric bypass[Title/Abstract]
-
23.
bariatric surgery[Title/Abstract]
-
24.
metabolic surgery[Title/Abstract]
-
25.
weight-loss surgery[Title/Abstract]
-
26.
digestive surgery[Title/Abstract]
-
27.
17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26
-
28.
(obesity[MeSH Terms]) OR morbid obesity[MeSH Terms]
-
29.
severe obesity[Title/Abstract]
-
30.
complex obesity[Title/Abstract]
-
31.
morbid obesity[Title/Abstract]
-
32.
weight-loss[Title/Abstract]
-
33.
28 or 29 or 30 or 31 or 32
-
34.
9 and 27—Total hits 1
-
35.
9 or 16
-
36.
27 and 35—Total hits 4
-
37.
1 and 27 and 33—Total hits 297
-
38.
1 and 27—Total hits 459
-
39.
1 and 27—Update 19/12/2016 Total hits 5
-
40.
1 and 27—Update 26/12/2016 Total hits 1
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Doble, B., Wordsworth, S., Rogers, C.A. et al. What Are the Real Procedural Costs of Bariatric Surgery? A Systematic Literature Review of Published Cost Analyses. OBES SURG 27, 2179–2192 (2017). https://doi.org/10.1007/s11695-017-2749-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2749-8