Abstract
Balamuthia mandrillaris is a free living amoeba that can be isolated from soil. It is an emerging pathogen causing skin lesions as well as CNS involvement with a fatal outcome if untreated. The infection has been described more commonly in inmunocompetent individuals, mostly males, many children, and with a predilection for population with Hispanic background in cases occurring in the United States. Except for Africa, all continents have reported the disease, although a majority of cases are seen in North and South America. In published reported cases from North America, most patients will debut with neurological symptoms, where as in countries like Peru, a skin lesion will precede other symptoms. The classical skin lesion is a plaque, mostly located on face or knee. Diagnosis requires a high level of suspicion. Therapeutic strategies require a multidrug approach, than includes at least one amebicidal drug, and prolonged periods of treatment.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Visvesvara GS, Martinez AJ, Schuster FL, et al. Leptomyxid amoeba, a new agent of amebic meningoencephalitis in humans and animals. J Clin Microbiol. 1990;28:2750–6.
Visvesvara GS, Schuster FL, Martinez AJ. Balamuthia mandrillaris, N. G., N. Sp., agent of amebic meningoencephalitis in humans and other animals. J Eukaryot Microbiol. 1993;40:504–14.
•• Diaz J. The public health threat from Balamuthia mandrillaris in the Southern United States. J La State Med Soc. 2011;163:197–203. The most updated review of all cases reported in the US.
Campos P, Cabrera J, Gotuzzo E, Guillen D. Neurological involvement in free living amebiasis. Rev Neurol. 1999 16–31;29(4):316–8.
CDC. Balamuthia amebic encephalitis—California, 1999–2007. MMWR. 2008;57:768–71.
Recavarren-Arce S, Verlarde C, Gotuzzo E, Cabrera J. Amoeba angeitic lesions of the central nervous system in Balamuthia mandrillaris amoebiasis. Hum Pathol. 1999;30:269–73.
Galarza C, Larrea P, Kumakawa H. Amebiasis Cutánea de Vida libre. Primer caso reportado en el Hospital Dos de Mayo, Lima, Perú. Dermatol Peru. 1997;7:65–9.
Ballona R, Aquije M. Compromiso cutáneo en encefalitis granulomatosa amebiana fatal causada por Balamuthia mandrillaris. Folia Dermatol Peru. 2003;14(1):28–30.
Taratuto AL, Monges J, Acefe JC, et al. Leptomyxid amoeba encephalitis: report of the first case in Argentina. Trans R Soc Trop Med Hyg. 1991;85(1):77.
Galarza M, Cuccia V, Sosa FP, Monges JA. Pediatric granulomatous cerebral amebiasis: a delayed diagnosis. Pediatr Neurol. 2002;26:153–6.
Martinez AJ, Guerra AE, Garcia-Tamayo J, et al. Granulomatous amebic encephalitis: a review and report of a spontaneous case from Venezuela. Acta Neuropathol. 1994;87:430–4.
Gonzalez-Alfonzo JE, Martinez AJ, Garcia V, et al. Granulomatous encephalitis due to a leptomyxid amoeba. Trans R Soc Trop Med Hyg. 1991;85(4):480.
Riestra-Castaneda JM, Riestra-Castaneda R, Gonzalez-Garrido AA, et al. Granulomatous amebic encephalitis due to Balamuthia mandrillaris (Leptomyxiidae): report of four cases from Mexico. AmJTrop Med Hyg. 1997;56(6):603–7.
Chimelli L, Hahn MD, Scaravilli F, et al. Granulomatous amoebic encephalitis due to leptomyxid amoebae: report of the first Brazilian case. Trans R Soc Trop Med Hyg. 1992;86(6):635.
Silva-Vergara ML, Da Cunha Colombo ER, De Figueiredo Vissotto E, et al. Disseminated Balamuthia mandrillaris amoeba infection in an AIDS patient from Brazil. AmJTrop Med Hyg. 2007;77(6):1096–8.
Cuevas PM, Smoje PG, Jofré ML, et al. Granulomatous amoebic meningoencephalitis by Balamuthia mandrillaris: case report and literature review. Rev Chil Infectol. 2006;23(3):237–42.
Oddó BD, Ciani AS, Vial CP. Granulomatous amebic encephalitis caused by Balamuthia mandrillaris. First case diagnosed in Chile. Rev Chil Infectol. 2006;23(3):232–6.
Schuster FL, Yagi S, Gavali S, et al. Under the radar: Balamuthia amebic encephalitis. Clin Infect Dis. 2009;1;48(7):879–87.
Deol I, Robledo L, Meza A, et al. Encephalitis due to a free-living amoeba (Balamuthia mandrillaris): case report with literature review. Surg Neurol. 2000;53(6):611–6.
Pritzker AS, Kim BK, Agrawal D, et al. Fatal granulomatous amebic encephalitis caused by Balamuthia mandrillaris presenting as a skin lesion. J Am Acad Dermatol. 2004;50(2 Suppl):38–41.
Kodet R, Nohýnková E, Tichý M, et al. Amebic encephalitis caused by Balamuthia mandrillaris in a Czech child: description of the first case from Europe. Pathol Res Pract. 1998;194(6):423–9.
White JM, Barker RD, Salisbury JR, et al. Granulomatous amoebic encephalitis. Lancet. 2004;364(9429):220.
Tavares M, da Costa JM Correia, Carpenter SS, et al. Diagnosis of first case of Balamuthia amoebic encephalitis in Portugal by immunofluorescence and PCR. J Clin Microbiol. 2006;44(7):2660–3.
Sangruchi T, Martinez AJ, Vivesvara GS. Spontaneous Granulomatous amebic encephalitis: report of four cases from Thailand. Southeast Asian J Trop Med Public Health. 1994;25:309–13.
Shirabe T, Monobe Y, Visvesvara GS. An autopsy case of amebic meningoencephalitis. The first Japanese case caused by Balamuthia mandrillaris. Neuropathology. 2002;22(3):213–7.
Reed RP, Cooke-Yarborough CM, Jaquiery AL, et al. Fatal granulomatous amoebic encephalitis caused by Balamuthia mandrillaris. Med J Aust. 1997;167(2):82–4.
Schuster FL, Glaser C, Honarmand S, et al. Balamuthia amebic encephalitis risk, Hispanic Americans. Emerg Infect Dis. 2004;10(8):1510–2.
• Centers for Disease Control and Prevention (CDC). Notes from the field: transplant-transmitted Balamuthia mandrillaris—Arizona. MMWR Morb Mortal Wkly Rep. 2010;59(36):1182. Disease is now reported as been transmissible trough organ donation.
Centers for Disease Control and Prevention (CDC). Balamuthia mandrillaris transmitted through organ transplantation Mississippi, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(36):1165–70.
Ahmad AF, Andrew PW, Kilvington S. Development of a nested PCR for environmental detection of the pathogenic free-living amoeba Balamuthia mandrillaris. Eukaryot Microbiol. 2011;58(3):269–71.
Schuster FL, Dunnebacke TH, Booton GC, et al. Environmental isolation of Balamuthia mandrillaris associated with a case of amebic encephalitis. J Clin Microbiol. 2003;41(7):3175–80.
Niyyati M, Lorenzo-Morales J, Rezaeian M, et al. Isolation of Balamuthia mandrillaris from urban dust, free of known infectious involvement. Parasitol Res. 2009;106(1):279–81.
Dunnebacke TH, Schuster FL, Yagi S, Booton GC. Balamuthia mandrillaris from soil samples. Microbiology. 2004;150(Pt 9):2837–42.
Huang ZH, Ferrante A, Carter RF. Serum antibodies to Balamuthia mandrillaris, a free-living amoeba recently demonstrated to cause granulomatous amoebic encephalitis. J Infect Dis. 1999;179(5):1305–8.
Schuster FL, Glaser C, Gilliam S, Visvesvara GS. Survey of sera from encephalitis patients for Balamuthia mandrillaris antibody. J Eukaryot Microbiol. 2001;Suppl:10S–2S.
Kiderlen AF, Radam E, Schuster FL, et al. Balamuthia and Acanthamoeba-binding antibodies in West African human sera. Exp Parasitol. 2010;126(1):28–32.
Visvesvara GS, Moura H, Schuster FL. Pathogenic and opportunistic free-living amoebae: Acanthamoeba spp., Balamuthia mandrillaris, Naegleria fowleri, and Sappinia diploidea. FEMS Immunol Med Microbiol. 2007;50(1):1–26.
Schuster FL, Visvesvara GS. Axenic growth and drug sensitivity studies of Balamuthia mandrillaris, an agent of amebic meningoencephalitis in human and other animals. J Clin Microbiol. 1996;34:385–8.
Matin A, Siddiqui R, Jung SY, et al. Balamuthia mandrillaris interactions with human brain microvascular endothelialcells in vitro. J Med Microbiol. 2007;56(Pt 8):1110–5.
Schuster FL, Yagi S, Wilkins PP, et al. Balamuthia mandrillaris, agent of amebic encephalitis: detection of serum antibodies and antigenic similarity of isolates by enzyme immunoassay. J Eukaryot Microbiol. 2008;55(4):313–20.
Yagi S, Schuster FL, Visvesvara GS. Demonstration of Balamuthia and Acanthamoeba mitochondrial DNA in sectioned archival brain and other tissues by the polymerase chain reaction. Parasitol Res. 2008;102(2):211–7.
Qvarnstrom Y, Visvesvara GS, Sriram R, da Silva AJ. Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp., Balamuthia mandrillaris, and Naegleria fowleri. J Clin Microbiol. 2006;44:3589–95.
Kiderlen AF, Radam E, Tata PS. Assessment of Balamuthia mandrillaris-specific serum antibody concentrations by flow cytometry. Parasitol Res. 2009;104(3):663–70.
Guarner J, Bartlett J, Shieh WJ, et al. Histopathologic spectrum and immunohistochemical diagnosis of amebic meningoencephalitis. Mod Pathol. 2007;20(12):1230–7.
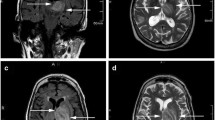
Healy J. Balamuthia mandrillaris encephalitis: radiographic and pathologic findings. Am J Neuroradiol. 2002;23:486–9.
Velarde C. Amebiasis de vida libre en el Peru: un estudio anatomo-patológico. Thesis presented for medical degree. Universidad Peruana Cayetano Heredia Faculty of Medicine. 1996.
•• Martínez DY, Seas C, Bravo F, et al. Successful treatment of Balamuthia mandrillaris amoebic infection with extensive neurological and cutaneous involvement. Clin Infect Dis. 2010;51(2):e7–e11. First description of miltefosin used as amebicidal in the treatment of the infection.
Schuster FL, Guglielmob ABJ, Visvesvara GS. In-vitro activity of miltefosine and voriconazole on clinical isolates of free-living amoebas: Balamuthia mandrillaris, Acanthamoeba spp., and Naegleria fowleri. J Eukaryot Microbiol. 2006;53:121–6.
Cary LC, Maul E, Potter C, et al. Balamuthia mandrillaris meningoencephalitis: survival of a pediatric patient. Pediatrics. 2010;125(3):e699–703.
Doyle JS, Campbell E, Fuller A, et al. Balamuthia mandrillaris brain abscess successfully treated with complete surgical excision and prolonged combination antimicrobial therapy. J Neurosurg. 2011;114:458–62.
Orozco L, Hanigan W, Khan M, Fratkin J, Lee M. Neurosurgical intervention in the diagnosis and treatment of Balamuthia mandrillaris encephalitis. J Neurosurg. 2011;115:636–40.
Acknowledgments
The authors want to recognize the joined effort of specialists from dermatology, infectious disease, neurology, pediatrics, pathology and microbiology departments at the IMTAvH and the Hospital Nacional Cayetano Heredia in caring for the patients with BMAI. It is a cooperative work among all these specialties what has allow us to reach the current level of knowledge about this disease. We also want to thank Dr. Dalila Martinez for keeping the register of patients at our institution.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bravo, F.G., Seas, C. Balamuthia Mandrillaris Amoebic Encephalitis: An Emerging Parasitic Infection. Curr Infect Dis Rep 14, 391–396 (2012). https://doi.org/10.1007/s11908-012-0266-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-012-0266-4