Abstract
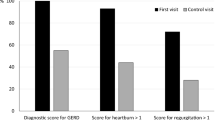
Gut Inflammatory bowel disease (IBD) is a group of chronic gastrointestinal disorders characterised by relapsing and remitting inflammation of the gastrointestinal tract. The two most common types of IBDs are ulcerative colitis and Crohn’s disease. Patients with glycogen storage disease (GSD) type Ia present with gastrointestinal symptoms such as recurrent abdominal pain, bloating and changes in stool form or frequency, which is clinically difficult to distinguish from IBD. We report the case of a 36-year-old man with GSD type Ia and IBD-like disease. A commercial probiotic (VSL#3®) was chosen as a nutritional supplement treatment because of its high content of microbial species and strains. Three different tests were performed: normal-dose, no-dose and half-dose tests. The study periods for the normal-dose, no-dose and half-dose tests were 4 weeks from the treatment initiation, 72 h from the end of the previous period and 4 weeks to 6 months after the end of the 72-h period, respectively. When the probiotic treatment was stopped, he experienced several symptoms similar to those before the start of the treatment. The intestinal symptoms were less severe with the half-dose nutritional supplement treatment than with no treatment. Probiotics may reduce the number of irritable gut episodes and improve the patient’s well-being and overall quality of life. More studies are needed to determine whether the improvement in more severe cases of GSD is due mainly to changes in the composition of the gut microbiota, as in this patient.



Similar content being viewed by others
References
Chen YT (2001) Glycogen storage diseases. In: Scriver C, Beaudet A, Sly W, Valle D (eds) The metabolic & molecular bases of inherited disease. McGraw-Hill, New York, pp 1521–1551
Fine RN, Kogut MD, Donnell GN (1969) Intestinal absorption in type I glycogen storage disease. J Pediatr 75(4):632–635. https://doi.org/10.1016/S0022-3476(69)80459-2
Lawrence NT, Chengsupanimit T, Brown LM, Derks TGJ, Smit GPA, Weinstein DA (2017) Inflammatory bowel disease in glycogen storage disease type Ia. J Pediatr Gastroenterol Nutr 64(2):e52–e54. https://doi.org/10.1097/MPG.0000000000000592
Lawrence NT, Chengsupanimit T, Brown LM, Weinstein DA (2015) High incidence of serologic markers of inflammatory bowel disease in asymptomatic patients with glycogen storage disease type Ia. JIMD Rep 24:123–128. https://doi.org/10.1007/8904_2015_452
Xavier RJ, Podolsky DK (2007) Unravelling the pathogenesis of inflammatory bowel disease. Nature 448(7152):427–434. https://doi.org/10.1038/nature06005
Laparra JM, Sanz Y (2010) Interactions of gut microbiota with functional food components and nutraceuticals. Pharmacol Res 61(3):219–225. https://doi.org/10.1016/j.phrs.2009.11.001
Aureli P, Capurso L, Castellazzi AM, Clerici M, Giovannini M, Morelli L, Poli A, Pregliasco F, Salvini F, Zuccotti GV (2011) Probiotics and health: an evidence-based review. Pharmacol Res 63(5):366–376. https://doi.org/10.1016/j.phrs.2011.02.006
Phillips ML (2009) Gut reaction: environmental effects on the human microbiota. Environ Health Perspect 117(5):A198–A205. https://doi.org/10.1289/ehp.117-a198
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, Nielsen T, Pons N, Levenez F, Yamada T, Mende DR, Li J, Xu J, Li S, Li D, Cao J, Wang B, Liang H, Zheng H, Xie Y, Tap J, Lepage P, Bertalan M, Batto JM, Hansen T, Le Paslier D, Linneberg A, Nielsen HB, Pelletier E, Renault P, Sicheritz-Ponten T, Turner K, Zhu H, Yu C, Li S, Jian M, Zhou Y, Li Y, Zhang X, Li S, Qin N, Yang H, Wang J, Brunak S, Doré J, Guarner F, Kristiansen K, Pedersen O, Parkhill J, Weissenbach J, MetaHIT Consortium, Bork P, Ehrlich SD, Wang J (2010) A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464(7285):59–65. https://doi.org/10.1038/nature08821
Tappenden KA, Deutsch AS (2007) The physiological relevance of the intestinal microbiota—contributions to human health. J Am Coll Nutr 26(6):679S–683S
Resta SC (2009) Effects of probiotics and commensals on intestinal epithelial physiology: implications for nutrient handling. J Physiol 587(Pt17):4169–4174. https://doi.org/10.1113/jphysiol.2009.176370
Brahe LK, Chatelier EL, Prifti E, Brahe LK, Chatelier EL, Prifti E, Pons N, Kennedy S, Hansen T, Pedersen O, Astrup A, Ehrlich SD, Larsen LH (2015) Specific gut microbiota features and metabolic markers in postmenopausal women with obesity. Nutr Diab 5(6):e159. https://doi.org/10.1038/nutd.2015.9
Larsen N, Vogensen FK, van den Berg FWJ, Nielsen DS, Andreasen AS, Pedersen BK, Al-Soud WA, Sørensen SJ, Hansen LH, Jakobsen M (2010) Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS One 5(2):e9085. https://doi.org/10.1371/journal.pone.0009085
Whelan K, Quigley EM (2013) Probiotics in the management of irritable bowel syndrome and inflammatory bowel disease. Curr Opin Gastroenterol 29(2):184–189. https://doi.org/10.1097/MOG.0b013e32835d7bba
Scaldaferri F, Gerardi V, Lopetuso LR, Zompo FD, Mangiola F, Boškoski I, Bruno G, Petito V, Laterza L, Cammarota G, Gaetani E, Sgambato A, Gasbarrini A (2013) Gut microbial flora, prebiotics, and probiotics in IBD: their current usage and utility. Biomed Res Int 2013:435268–435269. https://doi.org/10.1155/2013/435268
Ritchie ML, Romanuk TN (2012) A meta-analysis of probiotic efficacy for gastrointestinal diseases. PLoS One 7(4):e34938. https://doi.org/10.1371/journal.pone.0034938
Champagne CP, Ross RP, Saarela M, Hansen KF, Charalampopoulos D (2011) Recommendations for the viability assessment of probiotics as concentrated cultures and in food matrices. Int J Food Microbiol 149(3):185–193. https://doi.org/10.1016/j.ijfoodmicro.2011.07.005
Abayasekara LM, Perera J, Chandrasekharan V, Gnanam VS, Udunuwara NA, Liyanage DS, Bulathsinhala NE, Adikary S, Aluthmuhandiram JVS, Thanaseelan CS, Tharmakulasingam DP, Karunakaran T, Ilango J (2017) Detection of bacterial pathogens from clinical specimens using conventional microbial culture and 16S metagenomics: a comparative study. BMC Infect Dis 17(1):631. https://doi.org/10.1186/s12879-017-2727-8
Argollo M, Fiorino G, Hindryckx P, Peyrin-Biroulet L, Danese S (2017) Novel therapeutic targets for inflammatory bowel disease. J Autoimmun 85:103–116. https://doi.org/10.1016/j.jaut.2017.07.004
Kim YA, Keogh JB, Clifton PM (2017) The anti-diabetic effects of probiotics include reducing pro-inflammatory cytokines via a NF-κB pathway, reduced intestinal permeability, and lowered oxidative stress. Nutr Res Rev 17:1–17. https://doi.org/10.1017/S095442241700018X
Hegazy SK, El-Bedewy MM (2010) Effect of probiotics on pro-inflammatory cytokines and NF-kappaB activation in ulcerative colitis. World J Gastroenterol 16(33):4145–4151. https://doi.org/10.3748/wjg.v16.i33.4145
Rasmussen HE, Hamaker BR (2017) Prebiotics and inflammatory bowel disease. Gastroenterol Clin N Am 46(4):783–795. https://doi.org/10.1016/j.gtc.2017.08.004
Buss C, Valle-Tovo C, Miozzo S, Alves de Mattos A (2014) Probiotics and synbiotics mayimprove liver aminotransferases levels in non-alcoholic fatty liver disease patients. Ann Hepatol 13(5):482–488
Kirpich IA, Solovieva NV, Leikhter SN, Shidakova NA, Lebedeva OV, Sidorov PI, Bazhukova TA, Soloviev AG, Barve SS, McClain CJ, Cave M (2008) Probiotics restore bowel flora and improve liver enzymes in human alcohol-induced liver injury: a pilot study. Alcohol 42(8):675–682. https://doi.org/10.1016/j.alcohol.2008.08.006
Khalesi S, Johnson DW, Campbell K, Williams S, Fenning A, Saluja S, Irwin C (2017) Effect of probiotics and synbiotics consumption on serum concentrations of liver function test enzymes: a systematic review and meta-analysis. Eur J Nutr. https://doi.org/10.1007/s00394-017-1568-y
Ministro P, Martins D (2017) Fecal biomarkers in inflammatory bowel disease: how, when and why? Expert Rev Gastroenterol Hepatol 11(4):317–328. https://doi.org/10.1080/17474124.2017.129212
Conroy S, Hale MF, Cross SS, Swallow K, Sidhu RH, Sargur R, Lobo AJ (2017) Unrestricted faecal calprotectin testing performs poorly in the diagnosis of inflammatory bowel disease in patients in primary care. J Clin Pathol. https://doi.org/10.1136/jclinpath-2017-204506
Acknowledgements
We thank the staff of the Endocrinology and Nutrition consultation of the University of Santiago de Compostela Hospital Complex for their help in conducting the anthropometric measures.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Competing Interest
The authors declare that there are no competing interests regarding the publication of this paper.
Ethical Responsibilities
Right to privacy and informed consent. The authors have obtained informed consent of the patients and/or subjects referred to in the manuscript.
Electronic Supplementary Material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Carnero-Gregorio, M., Molares-Vila, A., Corbalán-Rivas, A. et al. Effect of VSL#3 Probiotic in a Patient with Glycogen Storage Disease Type Ia and Irritable Bowel Disease-like Disease. Probiotics & Antimicro. Prot. 11, 143–149 (2019). https://doi.org/10.1007/s12602-017-9372-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-017-9372-9