Abstract
Proctology is one of the surgical specialties that suffered the most during COVID-19 pandemic. Using data from a cross-sectional worldwide web survey, we aimed to snapshot the current status of proctologic practice in Italy with differences between three macro areas (North, Centre, South). Specialists affiliated to renowned scientific societies with an interest in coloproctology were invited to join a 27-item survey. Predictive power of respondents’ and hospitals’ demographics on the change of status of surgical activities was calculated. The study was registered at ClinicalTrials.gov (NCT 04392245). Of 299 respondents from Italy, 94 (40%) practiced in the North, 60 (25%) in the Centrer and 82 (35%) in the South and Islands. The majority were men (79%), at consultant level (70%), with a mean age of 46.5 years, practicing in academic hospitals (39%), where a dedicated proctologist was readily available (68%). Southern respondents were more at risk of infection compared to those from the Center (OR, 3.30; 95%CI 1.46; 7.47, P = 0.004), as were males (OR, 2.64; 95%CI 1.09; 6.37, P = 0.031) and those who routinely tested patients prior to surgery (OR, 3.02; 95%CI 1.39; 6.53, P = 0.005). The likelihood of ongoing surgical practice was higher in the South (OR 1.36, 95%CI 0.75; 2.46, P = 0.304) and in centers that were not fully dedicated to COVID-19 care (OR 4.00, 95%CI 1.88; 8.50, P < 0.001). The results of this survey highlight important factors contributing to the deadlock of proctologic practice in Italy and may inform the development of future management strategies.
Similar content being viewed by others
‘La vérité de demain se nourrit de l'erreur d'hier’
Antoine de Saint-Exupéry
Introduction
COVID-19 pandemic has critically impacted the surgical world [1]. More than 28 million procedures would be cancelled or postponed during the 12-week peak according to a recent global expert‐response study [2]. The vast majority (90%) of operations would be treating benign diseases, with an estimated overall 12-week cancellation rate of 72%.
This scenario has strongly challenged proctologic practice, which includes a large spectrum of conditions with a significant psycho-socio-economic burden [3].
Detection of the novel coronavirus (SARS-COV-2) RNA in patients’ stool samples and gastrointestinal epithelium has led to enhance infection control precautions [4]. Consequently, several guidelines have been developed to optimize treatment strategies while ensuring healthcare workers’ safety by means of adequate personal protective equipment (PPE) [5,6,7]. However, the ever-changing situation observed in most countries has often hampered the attempts to put these guidelines into practice [8].
ProctoLock 2020 is a survey aimed to assess the current status of proctologic practice worldwide.
In our previous global report [9], the proportion of unaltered, reduced or fully stopped practice has been snapshotted in 69 countries.
The purpose of this study was to explore the impact of COVID-19 on proctologic practice in Italy, looking for differences between North, South and Central regions.
Materials and methods
Experts in the field who joined a previous qualitative study [10] (N = 492) were invited to complete a web survey. The survey link was sent to national scientific societies of interest to coloproctologists and disseminated to their members. All collaborators committed to further recruitment of participants by direct invitation.
A 27-item survey (namely, ‘ProctoLock 2020′; Appendix 1) was designed and developed by the authors using an online platform (‘Online surveys’ [formerly BOS—Bristol Online Survey], developed by the University of Bristol) in accordance with the Checklist for Reporting Results of Internet E-Surveys (the CHERRIES statement) [11]. The finalized online survey was made available online from April 15th to 26th 2020. The survey aimed to capture the current status of proctologic practice worldwide, first exploring the overall changes in terms of resource allocation, and second assessing in more detail the various fields of application for both proctologic surgery (i.e. elective [oncological and non oncological] and urgent) and outpatient practice, with a focus on sexually transmitted disease and pelvic floor clinics. The availability of anorectal physiology testing was also assessed. The study was registered at ClinicalTrials.gov (NCT 04392245).
Statistical analysis
Logistic models for binary or ordinal variables were performed to assess the association between respondents’ preferences and their characteristics (adjusted odds ratio [OR]). Multivariable models were fitted using a pre-defined set of covariates which included respondents’ and hospitals’ demographics (i.e. geographical area, age, gender, type of hospital, hospital rearrangement, external facilities for proctologic surgery, use of PPE, pre-operative testing policies for COVID-19). Brant test to check the proportional odds assumption was performed for the ordinal logistic model. No formal correction for multiple testing has been made although we have critically assessed all P values < 0.05.
All analyses were performed using Stata 16 (StataCorp LLC, College Station, TX, USA).
Results
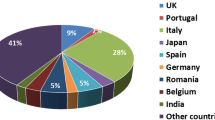
From a total of 1,050 respondents worldwide, 570 (54%) were Europeans (Appendix 2), with 299 (52%) from Italy. Among these, 94 (40%) practiced in the North, 60 (25%) in the Centre and 82 (35%) in the South and Islands (Table 1). The majority were men (79%), at consultant level (70%), with a mean age of 46.5 years, working in academic hospitals (39%), where a dedicated proctologist was readily available (68%). Overall, 34%, 54% and 70% reported the presence of dedicated pathways for sexually transmitted disease, pelvic floor disorders and anorectal physiology testing, respectively.
A multivariable logistic model showed that respondents from the South were more at risk of infection compared to those from the Centre (OR, 3.30; 95%CI 1.46; 7.47, P = 0.004), as were males (OR, 2.64; 95%CI 1.09; 6.37, P = 0.031) and those who routinely tested patients prior to surgery (OR, 3.02; 95CI 1.39; 6.53, P = 0.005) compared to their counterparts.
The majority of Italian respondents worked in centres that were partially rearranged (N = 216 [72%]) to guarantee the assistance to COVID-19 patients, with a similar distribution between regions (Table 2).
Conversely, hospitals fully converted to COVID-19 centers (N = 30 [10%]) and those not directly involved in COVID-19 care (N = 53 [18%]) were more prevalent in the North and South, respectively.
More than a half of respondents had modified the surgical informed consent for both COVID-19 positive (N = 164 [55%]) and negative patients (N = 177 [59%]), by mentioning the higher risk of infection and SARS-COV-2-related complications.
PPE ready availability and routine pre-operative testing for COVID-19 were more likely reported by respondents from the North (N = 92 [45%] and N = 93 [43%], respectively) compared to other regions (P = 0.002 and P = 0.033, respectively).
One-third of respondents (N = 97 [32%]) faced patients refusing surgery, with the fear of SARS-COV-2 infection as the main reason.
Forty percent (N = 116) of respondents had yet to reschedule patients waiting for surgery or outpatient visit.
Compared to the rest of Europe, elective proctologic surgery in Italy was considerably reduced (with a test of heterogeneity at P = 0.026) (Fig. 1).
The likelihood of ongoing proctologic practice was higher in southern regions (OR vs central regions 1.36, 95%CI 0.75; 2.46, P = 0.304) and in centers that were not fully dedicated to COVID-19 care (OR 4.00, 95%CI 1.88; 8.50, P < 0.001) (Table 3).
Among the 116 (39%) respondents who found flaws or delay in the management of oncological patients, the majority was from the North (N = 52 [56%]).
More than 82% (N = 247) of participants declared that elective non oncological surgery was fully stopped, with the main reasons being hospital directions and/or reduced referrals.
Emergency surgery was fully stopped according to one-fourth (N = 61) of respondents, while half (N = 150) experienced a reduced activity. Among those still performing emergency surgery (N = 238 [80%]), the majority (N = 212 [71%]) stated that patients were routinely tested for COVID-19 pre-operatively, with similar interregional distribution.
Following national or local hospital directions, outpatient activity was fully stopped or reduced in Italy according to 53% (N = 158) or 45% (N = 135) of respondents, respectively. The majority (127 [90%)]) reported regular use of PPE during the visits.
Possible diagnostic delays resulting from a decreased outpatient activity concerned 265 [88.6%] respondents.
Discussion
In Italy (and Europe), the hunt for patient zero has proven unsuccessful and only served to fuel the confusion on the origin of the outbreak [12]. SARS-COV-2 spread across Europe following multiple paths and heterogeneously impacted on countries and between different geographical areas within the same nation.
The higher prevalence of male over female subjects was consistent with the results of our worldwide survey [9].
Despite proctology has been recognized worldwide as subspecialty, only two-thirds of Italian respondents reported the availability of dedicated proctologist in their center.
The alarmingly high prevalence of COVID-19 positivity among Italian respondents (twice that of all healthcare workers) [13] might suggest that proctologists carry a higher risk of contagion compared to other specialists. Several case studies have reported gastrointestinal symptoms and/or evidence that some patients with COVID-19 have viral RNA viable in stool or gastrointestinal epithelium, suggesting fecal–oral pathway as a further possible route of transmission [4, 14, 15]. Compared to those from the Center, prevalence of COVID-19 positivity among Southern respondents was three times higher. In this geographic area, PPE were less frequently deemed readily available and the likelihood of continuing the surgical activity was 36% higher. Such a worrying proportion of COVID-19 positive respondents in the South suggests that the different timing of the epidemic and the prompt lockdown measures put in place by the Italian government likely may have rescued this area from a potential catastrophe.
As proof of resilience during troubled times, a significant number of respondents were redeployed to other activities [16].
More than 50% of respondents reported to have amended the surgical consent form, reflecting a great awareness of growing evidence from the literature about the increased operative risks in COVID-19 patients [17, 18].
Compared to the rest of Europe, the reduction in elective surgical activity has been more pronounced in Italy. To further confirm the deadlock of proctologic practice in this country, almost 40% of respondents had yet to reschedule patients’ outpatient visits or operations. While being unable to access healthcare services, many patients refrained from attending the emergency department due to the fear of being infected [19].
The suspension of oncological activity was reported by 39% of Italian respondents, with a peak of 56% in the North (the worst-hit area), where all activities were more likely to be put on hold and hospitals forced to shift all resources towards COVID-19 care.
Most respondents were concerned about the negative effects of delaying care, with potentially irreversible consequences, especially for cancer patients [20].
As recently suggested [7], the outpatient/office surgical activity could have helped to diminish commitment to hospitals and optimize resource allocation in terms of operating spaces, staffing and beds. But this was not the case for at least two reasons, namely the full closure of all non-COVID-related activities (as per national directions) and the currently very limited experience with delivering this type of proctologic surgery. Undoubtedly, this should prompt health authorities and specialists to redesign and optimize the whole proctologic pathway across the national territory [21, 22].
This study has some limitations that are commonly observed in survey-based studies (e.g. recall and selection bias). Nevertheless, the high percentage of consultants among respondents vouches for a satisfactory level of experience and supports the reliability of collected data.
The results of ProctoLock 2020 survey highlighted key critical issues that have emerged during COVID-19 pandemic worldwide and in particular in Italy, thus building foundations for future development of organizational solutions and nation-level initiatives.
References
Caricato M, Baiocchi GL, Crafa F et al (2020) Colorectal surgery in Italy during the Covid19 outbreak: a survey from the iCral study group [published online ahead of print, 2020 May 20]. Updates Surg. https://doi.org/10.1007/s13304-020-00760-3
CovidSurg Collaborative, Nepogodiev D, Bhangu A (2020) Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, 2020 May 12]. Br J Surg. https://doi.org/10.1002/bjs.11746
Giani I, Elbetti C, Trompetto M, Gallo G (2020) Proctology in the COVID-19 era: handle with care [published online ahead of print, 2020 May 15]. Br J Surg. https://doi.org/10.1002/bjs.11676
Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H (2020) Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 158(6):1831–1833.e3. https://doi.org/10.1053/j.gastro.2020.02.055
Gallo G, La Torre M, Pietroletti R et al (2020) Italian society of colorectal surgery recommendations for good clinical practice in colorectal surgery during the novel coronavirus pandemic. Tech Coloproctol 24(6):501–505. https://doi.org/10.1007/s10151-020-02209-6
COVIDSurg Collaborative (2020) Global guidance for surgical care during the COVID-19 pandemic [published online ahead of print, 2020 Apr 15]. Br J Surg. https://doi.org/10.1002/bjs.11646
Di Saverio S, Pata F, Gallo G et al (2020) Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. https://doi.org/10.1111/codi.15056
Felice C, Di Tanna GL, Zanus G, Grossi U (2020) Impact of COVID-19 outbreak on healthcare workers in Italy: results from a National E-Survey [published online ahead of print, 2020 May 22]. J Community Health. https://doi.org/10.1007/s10900-020-00845-5
https://clinicaltrials.gov/ct2/show/NCT04392245?term=proctolock&draw=2&rank=1. Accessed July 1st 2020
Ratto C, Grossi U, Litta F et al (2019) Contemporary surgical practice in the management of anal fistula: results from an international survey. Tech Coloproctol 23(8):729–741. https://doi.org/10.1007/s10151-019-02051-5
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [published correction appears in doi:10.2196/jmir.2042]. J Med Internet Res 6(3):e34
Carinci F (2020) Covid-19: preparedness, decentralisation, and the hunt for patient zero. BMJ 368:bmj.m799. https://doi.org/10.1136/bmj.m799
https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_7aprile%2520ITA.pdf. Accessed 7 April 2020
Hindson J (2020) COVID-19: faecal-oral transmission? Nat Rev Gastroenterol Hepatol 17(5):259. https://doi.org/10.1038/s41575-020-0295-7
Bianco F, Incollingo P, Grossi U, Gallo G (2020) Preventing transmission among operating room staff during COVID-19 pandemic: the role of the Aerosol Box and other personal protective equipment. Updates Surg. https://doi.org/10.1007/s13304-020-00818-2
Giulio M, Maggioni D, Montroni I et al (2020) Being a doctor will never be the same after the COVID-19 pandemic. Am J Med S0002–9343(20):30216–30223. https://doi.org/10.1016/j.amjmed.2020.03.003
Ives J, Huxtable R (2020) Surgical Ethics During a Pandemic: Moving into the Unknown? [published online ahead of print, 2020 Mar 30]. Br J Surg. https://doi.org/10.1002/bjs.11638
Bryan AF, Milner R, Roggin KK, Angelos P, Matthews JB (2020) Unknown unknowns: surgical consent during the COVID-19 pandemic [published online ahead of print, 2020 Apr 29]. Ann Surg. https://doi.org/10.1097/SLA.0000000000003995
de Leo D, Trabucchi M (2020) COVID-19 and the fears of Italian senior citizens. Int J Environ Res Public Health 17(10):E3572. https://doi.org/10.3390/ijerph17103572
Pellino G, Spinelli A (2020) How COVID-19 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection [published online ahead of print, 2020 Mar 17]. Dis Colon Rectum. https://doi.org/10.1097/DCR.0000000000001685
Elbetti C, Caminati F, Giani I et al (2019) Tailored anal block (TAB): a new anesthesia procedure for surgical treatment of hemorrhoids in an outpatient setting. Tech Coloproctol 23(5):497–500. https://doi.org/10.1007/s10151-019-01998-9
Gallo G, Sturiale A, De Simone V et al (2020) The impact of COVID-19 on proctologic practice in Italy. Tech Coloproctol. https://doi.org/10.1007/s10151-020-02319-1
Acknowledgements
PROCTOLOCK2020 Working Group: Italian Society of Colorectal Surgery (SICCR) Steering Committee: Domenico Aiello, Francesco Bianco, Andrea Bondurri, Gaetano Gallo, Marco La Torre, Giovanni Milito, Roberto Perinotti, Renato Pietroletti, Alberto Serventi, Marina Fiorino. Young Group of the Italian Society of Colorectal Surgery (Y-SICCR): Veronica De Simone, Ugo Grossi, Michele Manigrasso, Alessandro Sturiale, Gloria Zaffaroni. Mediterranean Society of Coloproctology (MSCP): Ferruccio Boffi. Dissemination Committee: Italy—Vittoria Bellato, Francesco Cantarella, Simona Deidda, Fabio Marino, Jacopo Martellucci, Marco Milone, Arcangelo Picciariello; Spain—Ana Minaya Bravo, Vincenzo Vigorita; Portugal—Miguel Fernandes Cunha; Turkey—Sezai Leventoglu; Russia—Tatiana Garmanova, Petr Tsarkov; Denmark—Alaa El-Hussuna; France—Alice Frontali; Greece—Argyrios Ioannidis; Belgium—Gabriele Bislenghi; Egypt—Mostafa Shalaby; Chile—Felipe Celedon Porzio; China—Jiong Wu; The Netherlands—David Zimmerman. External Advisors: Claudio Elbetti, Julio Mayol, Gabriele Naldini, Mario Trompetto, Giuseppe Sammarco, Giulio Aniello Santoro.
Funding
None reported.
Author information
Authors and Affiliations
Consortia
Contributions
GG, AS, IG, GLT, VS, UG contributed equally to this work: substantial contributions to the conception and design of the work; acquisition, analysis, and interpretation of data for the work. Drafting the work and revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved. SM, GM, FB, RP contributed equally to this work: Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved Members of the ProctoLock2020 Working Group are collaborators and are listed in Appendix A as ESM.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no personal conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the PROCTOLOCK2020 Working Group are listed in Acknowledgements section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gallo, G., Sturiale, A., De Simone, V. et al. Deadlock of proctologic practice in Italy during COVID-19 pandemic: a national report from ProctoLock2020. Updates Surg 72, 1255–1261 (2020). https://doi.org/10.1007/s13304-020-00860-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00860-0