Abstract
Purpose of Review
Regional anesthesia of the thoracic wall has rapidly progressed with refinement of existing techniques and the evolution of novel fascial plane techniques. This article aims to provide a narrative review of the key advancements in the last 5 years.
Recent Findings
Noteworthy developments include ultrasonography for the performance of thoracic epidural and paravertebral blockade, evidence indicating that thoracic paravertebral blockade carries similar analgesic efficacy to thoracic epidural analgesia, but with a superior side effect profile, and the description of multiple novel fascial plane techniques, including paraspinal thoracic plane blocks, intercostal-paraspinal plane blocks, the pectoral blocks, and the serratus plane block.
Summary
Ultrasound continues to change the practice of regional anesthesia, with integration into time-honored techniques such as epidural or paravertebral blockade. The established gold standard—the thoracic epidural—is being challenged, with a move towards paravertebral blockade. Fascial plane blocks hold promise for the future, but require further clinical trials for validation.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Romero A, Garcia JEL, Joshi GP. The state of the art in preventing postthoracotomy pain. Semin Thorac Cardiovasc Surg. 2013;25(2):116–24.
Chin KJ, Perlas A, Chan V, Brown-Shreves D, Koshkin A, Vaishnav V. Ultrasound imaging facilitates spinal anesthesia in adults with difficult surface anatomic landmarks. Anesthesiology. 2011;115(1):94–101.
Salman A, Arzola C, Tharmaratnam U, Balki M. Ultrasound imaging of the thoracic spine in paramedian sagittal oblique plane: the correlation between estimated and actual depth to the epidural space. Reg Anesth Pain Med. 2011;36(6):542–7.
Kessler J, Moriggl B, Grau T. The use of ultrasound improves the accuracy of epidural needle placement in cadavers. Surg Radiol Anat SRA. 2014;36(7):695–703.
Auyong DB, Hostetter L, Yuan SC, Slee AE, Hanson NA. Evaluation of ultrasound-assisted thoracic epidural placement in patients undergoing upper abdominal and thoracic surgery: a randomized, double-blind study. Reg Anesth Pain Med. 2016.
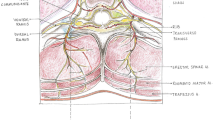
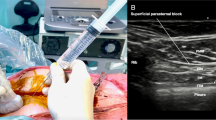
•• Krediet AC, Moayeri N, van Geffen G-J, Bruhn J, Renes S, Bigeleisen PE, et al. Different approaches to ultrasound-guided thoracic paravertebral block: an illustrated review. Anesthesiology. 2015;123(2):459–74. Excellent, detailed review of USG TPVB, with superb illustrations.
Norum HM, Breivik H. Learning from the past for the present: paravertebral blocks for thoracic surgery are not without risk. Eur J Anaesthesiol. 2011;28(7):544–5.
• Pace MM, Sharma B, Anderson-Dam J, Fleischmann K, Warren L, Stefanovich P. Ultrasound-guided thoracic paravertebral blockade: a retrospective study of the incidence of complications. Anesth Analg. 2016;122(4):1186–91. A retrospective study of 1427 USG TPVBs in 856 patients, with only six complications, including: symptomatic bradycardia and hypotension (n=3), a vasovagal episode (n=1), and possible local anesthetic systemic toxicity (LAST) (n=2). In particular, there were no instances of accidental pleural puncture or pneumothorax (8)
Wu J, Buggy D, Fleischmann E, Parra-Sanchez I, Treschan T, Kurz A, et al. Thoracic paravertebral regional anesthesia improves analgesia after breast cancer surgery: a randomized controlled multicentre clinical trial. Can J Anaesth J Can Anesth. 2015;62(3):241–51.
Mejdahl MK, Andersen KG, Gärtner R, Kroman N, Kehlet H. Persistent pain and sensory disturbances after treatment for breast cancer: six year nationwide follow-up study. BMJ. 2013;346:f1865.
Heesen M, Klimek M, Rossaint R, Imberger G, Straube S. Paravertebral block and persistent postoperative pain after breast surgery: meta-analysis and trial sequential analysis. Anaesthesia. 2016;71(12):1471–81.
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111(5):711–20.
Terkawi AS, Tsang S, Sessler DI, Terkawi RS, Nunemaker MS, Durieux ME, et al. Improving analgesic efficacy and safety of thoracic paravertebral block for breast surgery: a mixed-effects meta-analysis. Pain Physician. 2015;18(5):E757–80.
Ibarra MML, S-Carralero G-CM, Vicente GU, Cuartero del Pozo A, López Rincón R, Fajardo del Castillo MJ. Chronic postoperative pain after general anesthesia with or without a single-dose preincisional paravertebral nerve block in radical breast cancer surgery. Rev Esp Anestesiol Reanim. 2011;58(5):290–4.
Baidya DK, Khanna P, Maitra S. Analgesic efficacy and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2014;18(5):626–35.
Ding X, Jin S, Niu X, Ren H, Fu S, Li Q. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS ONE [Internet]. 2014 5 [cited 2017 Feb 26];9(5). Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4010440/
Jardim Júnior AP, Erdmann TR, dos Santos TV, Brunharo GM, Filho CTB, Losso MJ, et al. Comparison between continuous thoracic epidural and paravertebral blocks for postoperative analgesia in patients undergoing thoracotomy: systematic review. Rev Bras Anestesiol. 2013;63(5):433–42.
Scarfe AJ, Schuhmann-Hingel S, Duncan JK, Ma N, Atukorale YN, Cameron AL. Continuous paravertebral block for post-cardiothoracic surgery analgesia: a systematic review and meta-analysis. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg. 2016;50(6):1010–8.
• Yeung JHY, Gates S, Naidu BV, Wilson MJA, Gao SF. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2:CD009121. Cochrane review comparing TPVB against TEA for thoracotomy surgery. It concluded that TPVB provided similar analgesia to TEA, but with an improved side effect profile.
Teeter EG, Kumar PA. Pro: thoracic epidural block is superior to paravertebral blocks for open thoracic surgery. J Cardiothorac Vasc Anesth. 2015;29(6):1717–9.
Cowie B, McGlade D, Ivanusic J, Barrington MJ. Ultrasound-guided thoracic paravertebral blockade: a cadaveric study. Anesth Analg. 2010;110(6):1735–9.
Costache I, Sinclair J, Farrash FA, Nguyen TB, McCartney CJL, Ramnanan CJ, et al. Does paravertebral block require access to the paravertebral space? Anaesthesia. 2016;71(7):858–9.
Jüttner T, Werdehausen R, Hermanns H, Monaca E, Danzeisen O, Pannen BH, et al. The paravertebral lamina technique: a new regional anesthesia approach for breast surgery. J Clin Anesth. 2011;23(6):443–50.
Pfeiffer G, Oppitz N, Schöne S, Richter-Heine I, Höhne M, Koltermann C. Analgesia of the axilla using a paravertebral catheter in the lamina technique. Anaesthesist. 2006;55(4):423–7.
Voscopoulos C, Palaniappan D, Zeballos J, Ko H, Janfaza D, Vlassakov K. The ultrasound-guided retrolaminar block. Can J Anaesth J Can Anesth. 2013;60(9):888–95.
Zeballos JL, Voscopoulos C, Kapottos M, Janfaza D, Vlassakov K. Ultrasound-guided retrolaminar paravertebral block. Anaesthesia. 2013;68(6):649–51.
Murouchi T, Yamakage M. Retrolaminar block: analgesic efficacy and safety evaluation. J Anesth. 2016;30(6):1003–7.
• Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–7. First report of the ESPB, with a description of the ESPB in four patients, and cadaveric data.
Chin KJ, Forero M, Adhikary SD. Reply to Dr Ueshima and Dr Murouchi. Reg Anesth Pain Med. 2017;42(1):124–5.
Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: a case report. A A Case Rep. 2017; Epub ahead of print.
Shelley CL, Berry S, Howard J, De Ruyter M, Thepthepha M, Nazir N, et al. Posterior paramedian subrhomboidal analgesia versus thoracic epidural analgesia for pain control in patients with multiple rib fractures. J Trauma Acute Care Surg. 2016;81(3):463–7.
Truitt MS, Mooty RC, Amos J, Lorenzo M, Mangram A, Dunn E. Out with the old, in with the new: a novel approach to treating pain associated with rib fractures. World J Surg. 2010;34(10):2359–62.
Bryskin RB, Robie DK, Mansfield FM, Freid EB, Sukumvanich S. Introduction of a novel ultrasound-guided extrathoracic sub-paraspinal block for control of perioperative pain in Nuss procedure patients. J Pediatr Surg. 2016.
Roué C, Wallaert M, Kacha M, Havet E. Intercostal/paraspinal nerve block for thoracic surgery. Anaesthesia. 2016;71(1):112–3.
Elsharkawy H, Saifullah T, Kolli S, Drake R. Rhomboid intercostal block. Anaesthesia. 2016;71(7):856–7.
Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–13.
Blanco R. The “pecs block”: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66(9):847–8.
Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim 2012;59(9):470–475.
Blanco R. A reply. Anaesthesia. 2014;69(10):1173–4.
Pérez MF, Duany O, de la Torre PA. Redefining PECS blocks for postmastectomy analgesia. Reg Anesth Pain Med. 2015;40(6):729–30.
• Mayes J, Davison E, Panahi P, Patten D, Eljelani F, Womack J, et al. An anatomical evaluation of the serratus anterior plane block. Anaesthesia. 2016;71(9):1064–9. Cadaveric data detailing how the SPB acts—on the lateral cutaneous branches of the intercostal nerves.
Hards M, Harada A, Neville I, Harwell S, Babar M, Ravalia A, et al. The effect of serratus plane block performed under direct vision on postoperative pain in breast surgery. J Clin Anesth. 2016;34:427–31.
Hetta DF, Rezk KM. Pectoralis-serratus interfascial plane block vs thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anesth. 2016;34:91–7.
Durant E, Dixon B, Luftig J, Mantuani D, Herring A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am J Emerg Med. 2016;19.
Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014;17(5):E651–3.
Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18(3):E421–4.
Okmen K, Okmen BM, Uysal S. Serratus anterior plane (SAP) block used for thoracotomy analgesia: a case report. Korean J Pain. 2016;29(3):189–92.
Broseta AM, Errando C, De Andrés J, Díaz-Cambronero O, Ortega-Monzó J. Serratus plane block: the regional analgesia technique for thoracoscopy? Anaesthesia. 2015;70(11):1329–30.
Font MC, Navarro-Martinez J, Nadal SB, Munoz CG, Galiana-Ivars M, Montero PC. Continuous analgesia using a multi-holed catheter in serratus plane for thoracic surgery. Pain Physician. 2016;19(4):E684–6.
Tan YR, Quek KHY. Tackling the axillary blind spot with PECS II. Anaesthesia. 2015;70(2):230–1.
Purcell N, Wu D. Novel use of the PECS II block for upper limb fistula surgery. Anaesthesia. 2014;69(11):1294.
Bashandy GMN, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68–74.
Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: a randomized controlled trial. Br J Anaesth. 2016;117(3):382–6.
Li N-L, Yu B-L, Hung C-F. Paravertebral block plus thoracic wall block versus paravertebral block alone for analgesia of modified radical mastectomy: a retrospective cohort study. PLoS One. 2016;11(11):e0166227.
Wahba SS, Kamal SM. Thoracic paravertebral block versus pectoral nerve block for analgesia after breast surgery. Egypt J Anaesth. 2014;30:129–35.
Ueshima H, Kitamura A. Blocking of multiple anterior branches of intercostal nerves (Th2-6) using a transversus thoracic muscle plane block. Reg Anesth Pain Med. 2015;40(4):388.
de la Torre PA, García PD, Alvarez SL, Miguel FJG, Pérez MF. A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthet Surg J. 2014;34(1):198–200.
Del Buono R, Costa F, Agrò FE. Parasternal, pecto-intercostal, pecs, and transverse thoracic muscle plane blocks: a rose by any other name would smell as sweet. Reg Anesth Pain Med. 2016;41(6):791–2.
Raza I, Narayanan M, Venkataraju A, Ciocarlan A. Bilateral subpectoral interfascial plane catheters for analgesia for sternal fractures: a case report. Reg Anesth Pain Med. 2016;41(5):607–9.
Ohgoshi Y, Ino K, Matsukawa M. Ultrasound-guided parasternal intercostal nerve block. J Anesth. 2016;30(5):916.
Takahashi H, Suzuki T. Anterior thoracic medial block for administering postoperative analgesia in the internal mammary area. Reg Anesth Pain Med. 2016;41(5):660–1.
Chin KJ. An anatomical basis for naming plane blocks of the anteromedial chest wall. Reg Anesth Pain Med. 2017;42(in press).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kim Wild and Ki Jinn Chin declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Regional Anesthesia
Rights and permissions
About this article
Cite this article
Wild, K., Chin, K.J. Regional Techniques for Thoracic Wall Surgery. Curr Anesthesiol Rep 7, 212–219 (2017). https://doi.org/10.1007/s40140-017-0212-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-017-0212-y