Abstract
Introduction
The chemotherapeutic regimen recommended by guidelines to prevent the development of a drug-resistant strain of Mycobacterium avium complex (MAC) consists of a combination of clarithromycin, rifampicin, and ethambutol. In severe cases, it is desirable to use either kanamycin or streptomycin in addition to these three drugs. However, it is unclear whether treatment is administered in accordance with the guidelines in real-world clinical settings.
Objectives
This study aimed to determine the chemotherapy patterns among patients treated for MAC lung disease in medical facilities in Japan.
Methods
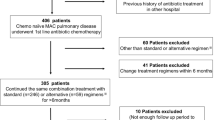
We investigated treatment patterns regarding patients treated for MAC lung disease between 2007 and 2017, in relation to the latest Japanese guidelines for the treatment of MAC lung disease, using insurance claims data of 378 patients.
Results
The basic triple-agent regimen of clarithromycin, ethambutol, and rifampicin was received by 238 (63%) of the 378 patients. Of these, 115 (48.3%) received the regimen for the recommended period of > 1 year. Therefore, widely publicizing the need for application of standard treatment for at least 2 years is necessary, as is the need to develop methods to overcome adverse effects.
Conclusion
Many patients with MAC lung disease do not complete a full course of treatment over the standard treatment period. Therefore, it is important to develop methods to overcome adverse effects or to develop an alternative treatment regimen for MAC lung disease.



Similar content being viewed by others
References
Ryu YJ, Koh WJ, Daley CL. Diagnosis and treatment of nontuberculous mycobacteria lung disease: clinicians’ perspectives. Tuberc Respir Dis. 2016;79(2):74–8.
Ho N, Atsuyuki K, Kozo M, et al. Epidemiology of pulmonary nontuberculous mycobacterial disease, Japan. Emerg Infect Dis. 2016;22(6):1116–7.
Adjemian J, Prevots DR, Gallagher J, et al. Lack of adherence to evidence-based treatment guidelines for nontuberculous mycobacterial lung disease. Ann Am Thorac Soc. 2014;11(1):9–16.
van Ingen J, Wagner D, Gallagher J, et al. Poor adherence to management guidelines in nontuberculous mycobacterial pulmonary diseases. Eur Respir J. 2017;49(2):1601855.
The Nontuberculous Mycobacteriosis Control Committee of the Japanese Society for Tuberculosis. The Scientific Assembly for Infection and Tuberculosis of the Japanese Respiratory Society, Guidelines for chemotherapy of pulmonary nontuberculous mycobacterial disease: 2012 revised version in Japanese. Kekkaku. 2013;88(1):29–32
Kwon YS, Koh WJ. Diagnosis and treatment of nontuberculous mycobacterial lung disease. J Korean Med Sci. 2016;31(5):649–59.
Griffith DE, Aksamit T, Brown-Elliot BA, et al. An Official ATS/IDSA Statement: diagnosis, treatment and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416.
Schlossberg DL, editor. Tuberculosis and nontuberculous mycobacterial infections. 7th ed. New York: ASM Press; 2017.
Haworth CS, Banks J, Capstick T, et al. British Thoracic Society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax. 2017;72(Suppl 2):ii1–64.
Yoshihiro K, Toshiharu M. The microbiological and clinical effects of combined therapy according to guidelines on the treatment of pulmonary Mycobacterium avium complex disease in Japan-including a follow-up study. Respiration. 2007;74(4):394–400.
Owusu-Edusei K, Marks SM, Miramontes R, et al. Tuberculosis hospitalization expenditures per patient from private health insurance claims data, 2010–2014. Int J Tuberc Lung Dis. 2017;21(4):398–404.
Japan Medical Data Center. JMDC Claims Database. https://www.jmdc.co.jp/en/pharma/database.html. Accessed 1 May 2019
Katsuhiro K, Toshiaki T. Clinical features and treatment history of clarithromycin resistance in M. avium-intracellulare complex pulmonary disease patients (in Japanese). Ann Jpn Resp Soc. 2007;45(8):587–92.
Meier A, Kirschner P, Springer B, et al. Identification of mutations in 23S rRNA gene of clarithromycin-resistant Mycobacterium intracellulare. Antimicrob Agents Chemother. 1994;38(2):381–4.
Yano H, Iwamoto T, Nishiuchi Y, et al. Population structure and local adaptation of MAC lung disease agent Mycobacterium avium subsp. hominissuis. Genome Biol Evol. 2017;9(9):2403–17.
Griffith DE, Brown-Elliot BA, Langsjoen B, et al. Clinical and molecular analysis of macrolide resistance in Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2006;174(8):928–34.
Kobashi Y, Matsushima T, Oka M. A double-blind randomized study of aminoglycoside infusion with combined therapy for pulmonary Mycobacterium avium complex disease. Respir Med. 2007;101(1):130–8.
Morimoto K, Iwai K, Uchimura K, et al. A steady increase in nontuberculous mycobacteriosis mortality and estimated prevalence in Japan. Ann Am Thorac Soc. 2014;11(1):487–90.
Acknowledgments
Tomohide Iwao wishes to thank Ms. Shigeko Noguchi for giving the opportunity to conduct this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was undertaken with the help of a research grant from the Japan Society for the Promotion of Science (grant number 17K17816) and the RintyuNet project led by the Japan Agency for Medical Research and Development.
Conflicts of interest
Tomohide Iwao, Genta Kato, Isao Ito, Toyohiro Hirai, and Tomohiro Kuroda declare no conflicts of interest.
Ethical approval
The insurance claims data was obtained from the JMDC in a completely anonymized form, therefore, approval from an Ethics Committee was not required, according to the rules of our organization.
Rights and permissions
About this article
Cite this article
Iwao, T., Kato, G., Ito, I. et al. Treatment of Mycobacterium avium–intracellulare complex lung disease in the real world: a retrospective big data analysis. Drugs Ther Perspect 36, 75–82 (2020). https://doi.org/10.1007/s40267-019-00687-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-019-00687-9