Abstract
Introduction
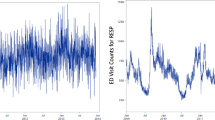
There have been no time-series studies of air pollution in Peru. Here we evaluate the effect of ambient PM2.5 on emergency room (ER) visits in Lima.
Methods
We estimated daily PM2.5 levels at a 1 km2 resolution during 2010–2016 using ground measurements, satellite data, and chemical transport model simulations. Population-weighted average daily PM2.5 levels were calculated for each district in Lima (n = 40), and assigned to patients based on residence. ER visits for respiratory and circulatory diseases were gathered from nine large public hospitals. Poisson regression was used to estimate the rate ratio for daily ER visits with change in daily PM2.5, controlling for meteorology, time trends, and district.
Results
For each interquartile range (IQR) increase in PM2.5, respiratory disease ER visits increased 4% (95% CI: 0–5%), stroke visits 10% (3–18%), and ischemic heart disease visits (adults, 18–64 years) 11% (−1, 24%). Districts with higher poverty showed significantly stronger associations of PM2.5 and respiratory disease ER visits than districts with lower poverty. Effects were diminished 24–42% using Lima-wide instead of district-specific PM2.5 levels.
Conclusions
Short-term exposure to ambient PM2.5 is associated with increases in ER visits in Lima for respiratory diseases and stroke, and among middle-aged adults, ischemic heart disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Achilleos S, Kioumourtzoglou MA, Wu CD, Schwartz JD, Koutrakis P, Papatheodorou SI. Acute effects of fine particulate matter constituents on mortality: a systematic review and meta-regression analysis. Environ Int. 2017;109:89–100.
Pope CA III, Turner MC, Burnett RT, Jerrett M, Gapstur SM, Diver WR, et al. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ Res. 2015;116:108–15.
Kim KH, Kabir E, Kabie S. A review on the human health impact of airborne particulate matter. Environ Int. 2015;74:136–43.
Apte JS, Marshall JD, Cohen AJ, Brauer M. Addressing global mortality from ambient PM2.5. Environ Sci Technol. 2015;49:8057–66.
World Health Organization (2018). Ambient (outdoor) air quality and health. https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (2018). Accessed 8 Mar 2019.
Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42:1187–95.
Requia W, Adams M, Arain A, Papatheodorou S, Koutrakis P, Mhmoud M. Global association of air pollution and cardiorespiratory diseases: a systematic review, meta-analysis, and investigation of modifier variables. Am J Public Health. 2018;108:S123–30.
World Health Organization Ambient (outdoor) air pollution in cities database 2014. https://www.who.int/phe/health_topics/outdoorair/databases/cities-2014/en/ (2014). Accessed 8 Mar 2019.
Silva J, Rojas J, Norabuena M, Molina C, Toro R, Leiva-Guzman M. Particulate matter levels in a South American megacity: the metropolitan area of Lima-Callao, Peru. Environ Monit Asses. 2017;189:635.
Gonzales GF, Steenland K. Environmental health in Peru: outdoor and indoor air contamination. Rev Panam Salud Publica. 2014;36:141.
Robinson CL, Baumann LM, Romero K, Combe JM, Gomez A, Gilman RH, et al. Effect of urbanization on asthma, allergy and airways inflammation in a developing country setting. Thorax. 2011;66:1051–7.
Underhill LJ, Bose S, Williams DL, Romero KM, Malpartioda G, Breyss PN, et al. Association of roadway proximity with indoor air pollution in a peri-urban community in Lima, Peru. Int J Environ Res Public Health. 2015;12:13466–81.
Carbajal-Arroyo L, Barraza-Villarreal A, Durand-Pardo R, Moreno-Macías H, Espinoza-Laín R, Chiarella-Ortigosa P, et al. Impact of traffic flow on the asthma prevalence among school children in Lima, Peru. J Asthma 2007;44:197–202.
Vu B, Sánchez O, Bi J, Qingyang Xiao Q, Hansel N, Checkley W, et al. Developing advanced PM2.5 exposure models in Lima, Peru. Remote Sens. 2019;11:641. https://doi.org/10.3390/rs11060641.
Bose S, Romero K, Psoter KJ, Curriero FC, Chen C, Johnson CM, et al. Association of traffic air pollution and rhinitis quality of life in Peruvian children with asthma. PLoS ONE. 2018;13:e0193910.
Grell GA, Peckham SE, Schmitz, McKee SA, Frost G, Skamarock WC, et al. Fully coupled “online” chemistry within the WRF model. Atmos Environ. 2005;39:6957–75.
Sánchez-Ccoyllo O, Ordoñez-Aquino C, Muñoz AL, lacza A, Andrade M, Liu Y. Modeling study of the particulate matter in lima with the WRF-Chem model: case study of April 2016. Int J Appl Eng Res. 2016;13:10129–41.
Sarnat SE, Sarnat JA, Mulholland J, Isakov V, Özkaynak H, Chang HH, et al. Application of alternative spatiotemporal metrics of ambient air pollution exposure in a time-series epidemiological study in Atlanta. J Expo Sci Environ Epidemiol. 2013;23:593–605.
Levy JI, Clougherty JE, Baxter LK, Houseman EA, Paciorek C. HEI Health Review Committee. Evaluating heterogeneity in indoor and outdoor air pollution using land-use regression and constrained factor analysis. Res Rep Health Eff Inst. 2010:5–80.
Liu Y, Peciorek CJ, Koutrakis P. Estimating regional spatial and temporal variability of PM2.5 concentrations using satellite data, meteorology, and land use information. Environ Health Perspect. 2009;117:886–92.
Miri M, Ghassoun Y, Dovlatabadi A, Ebrahimnejad A, Lowner MO. Estimated annual and seasonal PM1, PM2.5 and PM10 concentrations using land use regression model. Ecotoxicol Environ Saf. 2019;174:137–45.
Paciorek CJ, Liu Y, HEI Health Review Committee. Assessment and statistical modelling of the relationship between remotely sensed aerosol optical depth and PM2.5 in the eastern United States. Res Rep Health Eff Inst. 2012:5–83.
Chen SY, Lin YL, Chang WT, Lee CT, Chan CC. Increasing emergency room visits for stroke by elevated levels of fine particulate constituents. Sci Total Environ. 2014;473-474:446–50.
Ge E, Lai K, Xiao X, Luo M, Fang Z, Zeng Y, et al. Differential effects of size-specific particulate matter on emergency department visits for respiratory and cardiovascular diseases in Guangzhou, China. Environ Pollut. 2018;243:336–45.
Rodopoulou S, Samoli E, Chalbot MG, Kavouras IG. Air pollution and cardiovascular and respiratory emergency visits in Central Arkansas: a time-series analysis. Sci Total Environ. 2015;536:872–9.
Weber SA, Insaf TZ, Hall ES, Talbot TO, Huff AK. Assessing the impact of fine particulate matter (PM(2.5)) on respiratory-cardiovascular chronic diseases in the New York City Metropolitan area using Hierarchical Bayesian Model estimates. Environ Res. 2016;151:399–409.
Weichenthal S, Lavigne E, Evans G, Pollitt K, Burnett RT. Ambient PM2.5 and risk of emergency room visits for myocardial infarction: impact of regional PM2.5 oxidative potential: a case-crossover study. Environ Health. 2016;15:46.
Xu Q, Wang S, Guo Y, Wang C, Huang F, Li X, et al. Acute exposure to fine particulate matter and cardiovascular hospital emergency room visits in Beijing, China. Environ Pollut. 2017;220:317–27.
Zhang Q, Qi W, Yao W, Wang M, Chen Y, Zhou Y. Ambient particulate matter (PM(2.5)/PM(10)) exposure and emergency department visits for acute myocardial infarction in Chaoyang District, Beijing, China During 2014: a case-crossover study. J Epidemiol. 2016;26:538–45.
Metzger KB, Tolbert PE, Klein M, Peel JL, Flanders WD, Todd K, et al. Ambient air pollution and cardiovascular emergency department visits. Epidemiology. 2004;15:46–56.
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16:164–74.
Strickland MJ, Darrow LA, Klein M, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med. 2010;182:307–16.
Tapia V, Carbajal L, Vásquez V, Espinoza R, Vásquez-Velásquez C, Steenland K, et al. [Traffic regulation and environmental pollution by particulate material (2.5 and 10), sulfur dioxide, and nitrogen dioxide in Metropolitan Lima, Peru]. Rev Peru Med Exp Salud Publica. 2018;35:190–7.
Clougherty J, Shmool J, Kubzansky L. The role of non-chemical stressors in mediating socioeconomic susceptibility to environmental chemicals. Curr Environ Health Rep. 2014;1:302–13.
O’Lenick CR, Winquist A, Mulholland JA, Friberg MD, Chang HH, Kramer MR, et al. Assessment of neighbourhood-level socioeconomic status asa modifier of air pollution-asthma associations among children in Atlanta. J Epidemiol Community Health. 2017;71:129–36.
Cakmak S, Hebbern C, Cakmak JD, Vanos J. The modifying effect of socioeconomic status on the relationship between traffic, air pollution and respiratory health in elementary schoolchildren. J Environ Manag. 2016;177:1–8.
Wang Y, Shi L, Lee M, Liu P, Di Q, Zanobetti A, et al. Long-term exposure to PM2.5 and mortality among older adults in the Southeastern US. Epidemiology. 2017;28:207–14.
Chi GC, Hajat A, Bird CE, Cullen MR, Griffin BA, Miller KA, et al. Individual and neighborhood socioeconomic status and the association between air pollution and cardiovascular disease. Environ Health Perspect. 2016;124:1840–7.
Goodman JE, Loftus CT, Liu X, Zu K. Impact of respiratory infections, outdoor pollen, and socioeconomic status on associations between air pollutants and pediatric asthma hospital admissions. PLoS ONE. 2017;12:e0180522.
Valavanidis A, Fiotakis K, Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanism. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2008;26:339–62.
Byambaa B, Yang L, Matsuki A, Nagato EG, Gankhuyag K, Chuluunpure B, et al. Sources and characteristics of polycyclic aromatic hydrocarbons in ambient total suspended particles in Ulaanbaatar City, Mongolia. Int J Environ Res Public Health. 2019;16:442.
Acknowledgements
Research reported in this publication was supported by the NIH Fogarty International Center, National Institutes of Environmental Health Sciences (NIEHS) R01ES018845, R01ES018845-S1, National Cancer Institute, National Institute for Occupational Safety and Health, and the NIH under Award Number U01 TW0101 07. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank our colleagues at the Ministry of Health (MINSA) and the Ministry of the Environment (MINAM/SENAMHI) for their collaboration throughout this project.
Funding
The present study was founded by the National Institutes of Health (Fogarty Program) [Grant U01TW010107, 1/2 Regional GEOHealth Hub centered in Peru].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Tapia, V., Steenland, K., Sarnat, S.E. et al. Time-series analysis of ambient PM2.5 and cardiorespiratory emergency room visits in Lima, Peru during 2010–2016. J Expo Sci Environ Epidemiol 30, 680–688 (2020). https://doi.org/10.1038/s41370-019-0189-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-019-0189-3
Keywords
This article is cited by
-
An exploratory analysis of PM\(_{2.5}\)/PM\(_{10}\) ratio during spring 2016–2018 in Metropolitan Lima
Scientific Reports (2024)
-
Short-term exposure to various ambient air pollutants and emergency department visits for cause-stable ischemic heart disease: a time-series study in Shanghai, China
Scientific Reports (2023)
-
Effect modification by maximum temperature of the association between PM2.5 and short-term cardiorespiratory mortality and emergency room visits in Lima, Peru, 2010–2016
Journal of Exposure Science & Environmental Epidemiology (2022)
-
Air pollution and hospital admissions for critical illness in emergency department: a tertiary-center research in Changsha, China, 2016–2020
Environmental Science and Pollution Research (2022)
-
Air Pollution and Environmental Justice in Latin America: Where Are We and How Can We Move Forward?
Current Environmental Health Reports (2022)