Abstract
Objective To conduct a living systematic review of the clinical evidence about the effect of different mouthrinses on the viral load of SARS-CoV-2 in the saliva of infected patients.
Methods This study was reported using the PRISMA guidelines. An electronic search was conducted in seven databases and preprint repositories. We included human clinical trials that evaluated the effect of mouthrinses with antiseptic substances on the viral load of SARS-CoV-2 in the saliva of children or adults, who tested positive for SARS-CoV-2 by reverse transcriptase-polymerase chain reaction (RT-PCR). The risk of bias was assessed using the ROBINS-I tool. PROSPERO registration number: CRD42021240561.
Results Five studies were included (n = 66 participants). Study participants underwent oral rinses with hydrogen peroxide (H2O2) at 1%, povidone-iodine (PI) at 0.5% or 1%, chlorhexidine gluconate (CHX) at 0.2% or 0.12%, cetylpyridinium chloride (CPC) at 0.075%, and Linolasept. Only one study included a control group with sterile water. Three of the studies identified a reduction in viral load in saliva after the use of mouthrinses with PI (up to three hours), CHX (up to four hours), or Linolasept mouthwash (up to six hours). One study reported a statistically significant reduction after the use of mouthrinses with CPC or PI vs water (up to six hours) and one study reported a non-significant reduction in viral load after the use of H2O2 rinses.
Conclusions According to the present systematic review, the effect of mouthrinses on SARS-CoV-2 viral load in the saliva of COVID-19 patients remains uncertain. Evidence from well-designed randomised clinical trials is required for further and more objective evaluation of this effect.
Similar content being viewed by others
Introduction
The SARS-CoV-2 pandemic has had a great impact on the health of the global population because of its increasing spread and lack of treatment to prevent infection or reduce disease severity. Since the first case report in November 20191 and up to March 2021, more than 121 million infections and over 2.6 million deaths have been registered and cases continue to increase.2 The global scientific community has therefore started a series of studies aimed at identifying public health measures and technologies to mitigate the spread of this disease.
So far, the only effective measures endorsed by the World Health Organisation (WHO) to control and prevent the transmission of this disease at the community level are continuous hand washing, physical distancing, and the correct use of face masks.3 Likewise, concerning hospital care, the WHO has recommended the use of personal protective equipment (glasses/face shields, gloves, gowns, and N95 respirators or their equivalents), for health personnel who care for patients with COVID-19 and perform activities with a high risk of contagion, such as aerosol-generating procedures performed by dentists. These procedures can cause viral shedding through aerosols and splashes generated during dental care, potentially infecting health care personnel or patients who were seen between appointments.
Because there is no known treatment for COVID-19, the administration of a series of drugs currently being tested in clinical trials or approved for other uses has been proposed for off-label use during the pandemic - as preventive or recuperative therapies for COVID-19 based on studies describing some level of in vitro activity against SARS-CoV-2. Nonetheless, clinical studies published later have shown a lack of efficacy of these drugs to prevent or treat the disease, and in some cases, they were associated with higher mortality and morbidity.4 In the field of dentistry, various investigators have proposed that the preprocedural use of mouthrinses that include antiseptic substances could generate a reduction of SARS-CoV-2 viral load in the saliva of infected patients.5,6 These proposals are mainly based on evidence from in vitro studies,7 and more recently, human clinical trials.8
In response, international organisations such as the Centers for Disease Control and Prevention and the American Dental Association9,10 have incorporated recommendations about the use of mouthrinses before dental procedures in their guidelines for dental health care during the COVID-19 pandemic. These recommendations are aimed at reducing the load of oral microorganisms in aerosols generated during treatment, emphasising the lack of clinical evidence about their efficacy in reducing the transmission of SARS-CoV-2. This has generated controversy among the population, mouthrinse manufacturing companies, health care professionals, and researchers about the applicability of this measure in the prevention of SARS-CoV-2 infection.11
Taking into account the present interest in the utility of this oral hygiene product in the prevention of SARS-CoV-2 infection, the objective of this study was to make a living systematic review of the clinical evidence regarding the effect of different mouthrinses on the viral load of SARS-CoV-2 in the saliva of infected patients. Additionally, we aimed to evaluate the effect of mouthwashes on the quantification of the virus in the aerosols generated during dental care of infected patients, and the duration of the reduction of viral load in saliva and aerosols. We will also perform periodic updates of the study search, since according to the ClinicalTrials.gov registry, clinical trials on the subject are ongoing.12,13,14 This will eventually provide new clinical evidence to complement the currently published information and the conclusions of this systematic review.
Methods
The protocol of this living systematic review was prospectively registered in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement15 on PROSPERO with reference number CRD42021240561. We will update the search every month according to the availability of new evidence as a living systematic review.16 We also plan to maintain the review in a living mode for at least 12 months from the publication of the protocol. This article currently reports the basic findings from relevant articles identified up to May 24 2021. The results reported comply with the 'Preferred Reporting Items for Systematic reviews and Meta-Analyses' (PRISMA) guidelines17 (see online Supplementary Checklist 1).
Inclusion criteria
We included human clinical trials that evaluated the effect of mouthrinses with antiseptic substances on the viral load of SARS-CoV-2 in the saliva of patients, children or adults with COVID-19, diagnosed by reverse transcriptase-polymerase chain reaction (RT-PCR). Likewise, we included studies that evaluated the outcome of viral load on aerosols generated during dental procedures, the duration of the reduction in viral load, viral clearance, SARS-CoV-2 cellular infectivity in saliva, and salivary cytokine profiles. We did not restrict our criteria to any dosage, duration, or timing of mouthrinses. The comparison of interest was distilled water, sterile water, tap water, saline solution, or no treatment. We included articles published in both peer-reviewed journals and preprints, and publications written either in English or Spanish. We excluded comments, conference abstracts, interviews, and studies developed in animal models or in vitro conditions. The preprints included will be reassessed at the time of peer-reviewed publication, and the most recent version will be included.
Search strategy
A systematic electronic search of articles published up to February 26 2021 was conducted using PubMed, CINAHL, The Cochrane Library, Embase, Scopus, Dentistry & Oral Sciences Source, and LILACS databases. Preprint repositories including medRxiv and bioRxiv were also searched. This search was later updated to include articles published until May 24 2021.
A librarian (DC) developed the search strategies which were later validated by the authors (AHV, ABP, and DA). We initially designed a search strategy in PubMed, which was adapted to the other databases containing the following terms with synonyms and other medical descriptors: 'coronavirus', 'SARS-CoV-2' and 'mouthrinse'. The details of the search terms used are given in online Supplementary Table 1. The same search strategies will be run on every update. We also manually screened the references of the original studies and reviews that were included to identify additional eligible studies. Restrictions on date, language, study design, or publication status were not applied to the searches in the databases.
For this living systematic review, three independent authors (DC, ABP, and AHV) will receive an updated literature search file every month. They will continuously include relevant, newly published, or unpublished studies as per the above inclusion criteria.
Study selection
Initially, the results of the electronic search were imported to the reference management software EndNote X9. We eliminated all duplicate registries following the methodology described by Bramer et al.18 An independent two-stage screening process was undertaken to identify studies meeting the eligibility criteria by two authors (ABP and AHV) using the web application 'Rayyan'.19 First, we evaluated the registries by title and abstract; those appearing to meet the inclusion criteria were selected and the remaining were discarded. Afterward, full texts of the selected papers were evaluated under the same inclusion criteria. Any disagreement was discussed among the reviewers and in case of indecisiveness, a third reviewer took part in the discussion (DA).
Extraction and synthesis of results
The reduction of viral load of SARS-CoV-2 in saliva or aerosols generated by dental procedures and the duration of the said reduction was reported using different units of measurement registered before and after the use of mouthrinses according to the results of each study. If a study did not report relevant data for extraction (for example, viral load of SARS-CoV-2 in saliva), the corresponding author was contacted in order to obtain that information. In the absence of response, if the values of viral load of SARS-CoV-2 were available in published figures of the manuscript, these data were then extracted via WebPlotDigitizer version 4.4.20 The data were independently extracted by two authors (ABP and AHV), and any disagreement was resolved through discussion with a third author (DA).
We also extracted the following information: study design, settings, participant characteristics, study eligibility criteria, intervention, control, and the risk of bias assessment for each study. Data were independently extracted by two authors (ABP and AHV) using standardised forms. If these data were not reported, we contacted the authors to request them.
The general information about the publications and specific data of each study included are compiled in the summary tables. For any outcome in which data were sufficient to calculate an effect estimate, we planned to conduct a meta-analysis.
Risk of bias assessment
Two authors (AHV and ABP) independently assessed the risk of bias using the ROBINS-I (Risk Of Bias In Non-Randomized Studies of Interventions) tool,21 and disagreements were resolved through discussion with a third author (DA).
Ethical considerations
We did not request approval of the study by an Institutional Review Board because this is a revision of bibliographic databases.
Results
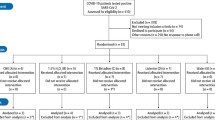
The search strategy among the different databases identified 860 articles. After removing duplicates, 660 articles were included and a total of 648 studies were excluded in phase one after the title and abstract review. The remaining 12 articles were evaluated in full text, and seven were excluded after this evaluation; the reasons for exclusion were: not measuring viral load in saliva or aerosols after the intervention with mouthrinses (six studies), and only considering qualitative measurements to establish the diagnosis of COVID-19 (one study) (Fig. 1). After this process, five studies (see online Supplementary References 1) were included.8,22,23,24,25
Three of the studies included were original articles,8,24,25 whereas the rest were short communications.22,23 All were reported in English (n = 5). Among the five studies, a total of 66 participants were included. The patients subjected to an intervention received mouthrinses with either hydrogen peroxide (H2O2) 1%, povidone-iodine (PI) (0.5% or 1%), chlorhexidine gluconate (CHX) (0.2% or 0.12%), or cetylpyridinium chloride (CPC) (0.075%). One study only specified the use of an over-the-counter antiseptic mouthwash for their intervention ('Linolasept'), and no active component was named. Only one study included a control group that used sterile water for comparisons.8 This latter study included the second largest number of participants (n = 16) and mentioned having used commercially available mouthrinses with PI, CHX, and CPC (Table 1).
The main objective of these studies was to evaluate the effect of the use of different mouthrinses on the viral load of SARS-CoV-2 in the oral cavity or saliva. Measurements of this outcome were conducted before and after the intervention at variable time intervals. The minimum interval of time post intervention for the first measurement was five minutes, and the maximum was six hours. The highest number of measurements per participant was five (basal, after five minutes, one hour, two hours, and three hours; and basal, after five minutes, two hours, four hours, and six hours) and the lowest was two (basal and after five minutes; and, basal and after 30 minutes). Most studies were carried out in a single day and only one conducted serial measurements at the hospital on days 3 and 6 (Table 1).24
The viral load obtained during follow-up was reported as copies/mL and only one study reported it as average fold change values calculated from cycle threshold values. Measurements of viral load were highly variable and at times conflicting among the studies (Table 2). In their intervention, Yoon et al. observed that in two patients on hospital day 3, the viral load became undetectable at two and four hours of follow-up after the use of mouthrinses based on CHX, becoming detectable again after six hours.24 Nonetheless, on hospital day 6, the viral load of SARS-CoV-2 was detectable in all the follow-up measurements.24 Seneviratne et al. identified statistically significant differences in the average fold changes of viral load values after the use of mouthrinses from baseline, in comparisons between CPC vs. water at five minutes and six hours of follow-up, and PI vs. water at six hours of follow-up.8 Likewise, Martínez Lamas et al. observed a progressive reduction of the mean viral load obtained from the four participants from baseline until three hours of follow-up.23 Meanwhile, Schürmann described how the viral load of SARS-CoV-2 can be reduced by up to 90% after the use of mouthrinse and recovers to preintervention values after approximately six hours. These authors agree that the use of mouthrinses could reduce the viral load of SARS-CoV-2 in the saliva samples of patients, reaffirming the need for more thorough studies to confirm these preliminary findings.8,23,24,25 In contrast, Gottsauner et al. concluded that mouthrinses based on H2O2 1% did not reduce the intraoral viral load of those infected with the new coronavirus and were not able to establish a statistically significant reduction in the viral load in saliva after 30 minutes of follow-up in ten patients.22
Assessment of the risk of bias
After using the ROBINS-I tool, we concluded that the five studies analysed have a critical22,23,24,25 or serious risk8 of bias mainly because confounding factors and the selection of patients (Fig. 2) were not controlled. Regarding the first domain, the majority of studies did not consider the beginning of COVID-19 symptoms, did not control the ingestion of food or water by patients before the start of the intervention, and in one study, participants had been taking antiviral medication during the duration of the study.24 For the second domain, these studies had very small samples, with the largest including only 29 patients (with measurements at baseline and after five minutes) of 34 recruited.25 Moreover, the characteristics of the participants were very heterogeneous among the studies, and no clear inclusion or exclusion criteria were established.
Discussion
The main objective of this living systematic review was to evaluate the effect of different kinds of mouthrinses on the viral load of SARS-CoV-2 in the saliva of patients with COVID-19. Five studies were included: three published in original article format and two as short communications. They included patients with positive SARS-CoV-2 infection confirmed by RT-PCR (66 participants in total), who underwent oral rinses with H2O2 at 1%, PI at 0.5% or 1%, CHX at 0.2% or 0.12%, CPC at 0.075% or other kinds of antiseptic mouthwashes (Linolasept). Only one of the studies included a control group in which sterile water was used. All studies included a baseline assessment of viral load in saliva or oropharyngeal secretions and between two and five follow-up periods with a minimum of five minutes and a maximum of six hours after the intervention. Measurement of viral load was reported in copies/mL and one of the studies used the average fold change values of the cycle threshold values to determine changes in the viral load from baseline and each follow-up. Three of the studies identified a reduction of viral load in saliva after the use of mouthrinses with PI (up to three hours), CHX (up to four hours), and Linolasept mouthwash (up to six hours). One study reported a statisticaly significant reduction after the use of mouthrinses with CPC or PI vs. water (up to six hours), and, one study reported a non significant reduction in viral load after the use of H2O2 rinses (comparing baseline vs 30-minute measurements). All the studies evaluated were at high risk of bias.
The results of four studies reported that the use of mouthrinses with PI, CHX, CPC or an over-the-counter mouthwash (Linolasept) could reduce the viral load of SARS-CoV-2 in the saliva of confirmed COVID-19 patients. However, it should be taken into account that the evidence to date corresponds to studies with a small sample size (between two and 34 patients) and with a risk of serious or critical bias - mainly because the potential effect of confounding variables is impossible to control. For example, the studies did not take into account variables such as the onset of COVID-19 symptoms or the consumption of food before the intervention, which could have had an impact on the viral load in saliva. Therefore, with the results of these studies, it is not possible to conclude that the reduction in viral load is solely based on the effect of the mouthrinses. In addition, despite the fact that most of the studies included reported a positive effect on reducing the viral load of SARS-CoV-2, we could not state that these results are consistent, because of the marked heterogeneity among the studies. These differences were mainly identified in the measurement units used to express viral load, the number and periods of follow-up, the concentrations of antiseptic substances, and the procedures for the use of mouthrinses, among other aspects. Future studies must address confounding factors through the development of well-designed randomised clinical trials, or at least, well designed prospective studies preferably using matching techniques of analysis (for example, propensity score matching).
Moreover, the studies analysed suggest that different types of mouthrinses reduce the viral load of SARS-CoV-2 in the saliva of infected patients for variable time frames after their application, with one study reporting a maximum time of 6 hours. This could translate into a reduction in the viral content found in aerosols generated during dental procedures, resulting in a reduction in the spread of the disease in health personnel and patients without infection. However, we must highlight that none of the studies included evaluated this outcome nor were they developed in dental clinical settings; therefore, based on the current evidence, the effect of mouthwashes on the viral load of SARS-CoV-2 in aerosols generated during dental procedures remains unknown. Furthermore, the included studies did not conduct viral load measurements after the performance of a dental procedure. This is important because it is hypothesised that SARS-CoV-2 could be present in the salivary glands of infected patients26,27 and expelled into the oral cavity through saliva.28,29,30 Therefore, given that salivary secretion is stimulated during oral instrumentation for dental procedures, it would be reasonable to assume that the duration of viral load reduction would probably be shorter in clinical scenarios. Evidence from studies of a higher methodological level, such as randomised clinical trials, conducted in real or simulated clinical settings is of vital importance to better understand the effect of mouthrinses on SARS-CoV-2 viral load in the saliva of patients with COVID-19 and in aerosols generated during dental procedures in these patients.
One of the limitations of our study is that because of the low quality of the studies, the small sample size, the heterogeneity reported in terms of follow-up periods, and reporting of viral load measurement, the calculation of a meta-analysis would have very limited utility. However, an extensive bibliographic search has been carried out in seven databases, and the search has also been extended to preprint repositories including medRxiv and bioRxiv, to cover the greatest amount of evidence available on the subject. Likewise, the present study has a living systematic review design to perform future updates according to the results of completed or ongoing clinical trials registered in the ClinicalTrials.gov portal. This will enable the adoption of a more conclusive position for or against the use of mouthrinses to reduce the viral load of SARS-CoV-2 in the saliva of patients with COVID-19.
Conclusion
In conclusion, according to the present systematic review, the effect of mouthrinses on the viral load of SARS-CoV-2 continues to be uncertain. The recommendations by governmental organisations around the world about the use of these mouthrinses as a preventive measure against infection by SARS-CoV-2 could generate a false sense of security among dentists, care staff, and patients. This could subsequently lead to a groundless reduction in the use of known effective measures for the prevention of infection and dissemination of COVID-19 during aerosol-generating procedures, resulting in an increase in contagion rates.
Change history
24 June 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41432-022-0279-2
References
Kpozehouen E B, Chen X, Zhu M, Macintyre C R. Using Open-Source Intelligence to Detect Early Signals of COVID-19 in China: Descriptive Study. JMIR Public Health Surveill 2020; DOI: 10.2196/18939.
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020; 20: 533-534.
World Health Organisation. Coronavirus disease (COVID-19) advice for the public. 2020. Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed July 2021).
Ghazy R M, Almaghraby A, Shaaban R et al. A systematic review and meta-analysis on chloroquine and hydroxychloroquine as monotherapy or combined with azithromycin in COVID-19 treatment. Sci Rep 2020; 10: 22139.
O'Donnell V B, Thomas D, Stanton R et al. Potential Role of Oral Rinses Targeting the Viral Lipid Envelope in SARS-CoV-2 Infection. Function (Oxf) 2020; DOI: 10.1093/function/zqaa002.
Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020; 12: 9.
Meister T L, Brüggemann Y, Todt D et al. Virucidal Efficacy of Different Oral Rinses Against Severe Acute Respiratory Syndrome Coronavirus 2. J Infect Dis 2020; 222: 1289-1292.
Seneviratne C J, Balan P, Ko K K K et al. Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: randomized control trial in Singapore. Infection 2021; 49: 305-311.
American Dental Association. ADA interim guidance for minimizing risk of COVID-19 transmission. Chicago: ADA, 2020.
Centres for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. 2020. Available at https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (accessed July 2021).
Reis I N R, do Amaral G, Mendoza A A H et al. Can preprocedural mouthrinses reduce SARS-CoV-2 load in dental aerosols? Med Hypotheses 2021; 146: 110436.
Clinical Trials.gov. Double-blind, Randomized, Parallel, Placebo-controlled Clinical Study to Evaluate the Viral Load of SARS-CoV-2 in the Oral Cavity of SARS-CoV-2 Positive Subjects After the Use of a Mouthwash Containing Cetylpyridinium Chloride 0,07%. 2021. Available at https://clinicaltrials.gov/ct2/show/NCT04757818 (accessed July 2021).
Clinical Trials.gov. The Efficacy of Pre-procedural Mouth Rinses on COVID-19 Saliva Viral Load. 2021. Available at https://clinicaltrials.gov/ct2/show/NCT04721457 (accessed July 2021).
Clinical Trials.gov. Mouth Rinses for Inactivation of COVID-19. 2020. Available at https://clinicaltrials.gov/ct2/show/NCT04584684 (accessed July 2021).
Moher D, Shamseer L, Clarke M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1.
Elliott J H, Synnot A, Turner T et al. Living systematic review: 1. Introduction-the why, what, when, and how. J Clin Epidemiol 2017; 91: 23-30.
Moher D, Liberati A, Tetzlaff J, Altman D G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006-1012.
Bramer W M, Giustini D, de Jonge G B, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016; 104: 240-243.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210.
Rohatgi A. WebPlotDigitizer version 4.4. 2020. Available at https://automeris.io/WebPlotDigitizer (accessed July 2021).
Sterne J A, Hernán M A, Reeves B C et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; DOI: 10.1136/bmj.i4919.
Gottsauner M J, Michaelides I, Schmidt B et al. A prospective clinical pilot study on the effects of a hydrogen peroxide mouthrinse on the intraoral viral load of SARS-CoV-2. Clin Oral Investig 2020; 24: 3707-3713.
Martínez Lamas L, Diz Dios P, Pérez Rodríguez M T et al. Is povidone iodine mouthwash effective against SARS-CoV-2? First in vivo tests. Oral Dis 2020; DOI: 10.1111/odi.13526.
Yoon J G, Yoon J, Song J Y et al. Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva. J Korean Med Sci 2020; DOI: 10.3346/jkms.2020.35.e195.
Schürmann M, Aljubeh M, Tiemann C, Sudhoff H. Mouthrinses against SARS-CoV-2: anti-inflammatory effectivity and a clinical pilot study. Eur Arch Otorhinolaryngol 2021; 278: 5059-5067.
Xu J, Li Y, Gan F, Du Y, Yao Y. Salivary Glands: Potential Reservoirs for COVID-19 Asymptomatic Infection. J Dent Res 2020; 99: 989.
Xu R, Cui B, Duan X, Zhang P, Zhou X, Yuan Q. Saliva: potential diagnostic value and transmission of 2019-nCoV. Int J Oral Sci 2020; 12: 11.
Sakanashi D, Asai N, Nakamura A et al. Comparative evaluation of nasopharyngeal swab and saliva specimens for the molecular detection of SARS-CoV-2 RNA in Japanese patients with COVID-19. J Infect Chemother 2021; 27: 126-129.
Wyllie A L, Fournier J, Casanovas-Massana A et al. Saliva or Nasopharyngeal Swab Specimens for Detection of SARS-CoV-2. N Engl J Med 2020; 383: 1283-1286.
Zhu J, Guo J, Xu Y, Chen X. Viral dynamics of SARS-CoV-2 in saliva from infected patients. J Infect 2020; DOI: 10.1016/j.jinf.2020.06.059.
Acknowledgements
The authors are grateful to Donna Pringle for reviewing the language and style.
Funding
None.
Author information
Authors and Affiliations
Contributions
AHV and DA conceived the study. All authors contributed to the design of the study. DA and AHV were involved in the planning, supervision and validation of the work. DC executed the searches and de-duplicated the references. For the review, AHV and ABP contributed to the data screening, data extraction and assessment of study quality. AHV, ABP and DA contributed to the analyses of the results and the writing of the manuscript. All authors contributed to the preparation of tables and figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The authors declared that they had no conflicts of interest.
Supplementary Information
Rights and permissions
About this article
Cite this article
Hernández-Vásquez, A., Barrenechea-Pulache, A., Comandé, D. et al. Mouthrinses and SARS-CoV-2 viral load in saliva: a living systematic review. Evid Based Dent (2022). https://doi.org/10.1038/s41432-022-0253-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41432-022-0253-z
This article is cited by
-
Efficacy of mouthwash on reducing salivary SARS-CoV-2 viral load and clinical symptoms: a systematic review and meta-analysis
BMC Infectious Diseases (2023)
-
Efficacy of three antimicrobial mouthwashes in reducing SARS-CoV-2 viral load in the saliva of hospitalized patients: a randomized controlled pilot study
Scientific Reports (2023)
-
Aerosol in the oral health-care setting: a misty topic
Clinical Oral Investigations (2023)