Abstract
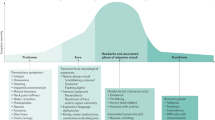
Cluster headache is a debilitating primary headache disorder that affects approximately 0.1% of the population worldwide. Cluster headache attacks involve severe unilateral pain in the trigeminal distribution together with ipsilateral cranial autonomic features and a sense of agitation. Acute treatments are available and are effective in just over half of the patients. Until recently, preventive medications were borrowed from non-headache indications, so management of cluster headache is challenging. However, as our understanding of cluster headache pathophysiology has evolved on the basis of key bench and neuroimaging studies, crucial neuropeptides and brain structures have been identified as emerging treatment targets. In this Review, we provide an overview of what is known about the pathophysiology of cluster headache and discuss the existing treatment options and their mechanisms of action. Existing acute treatments include triptans and high-flow oxygen, interim treatment options include corticosteroids in oral form or for greater occipital nerve block, and preventive treatments include verapamil, lithium, melatonin and topiramate. We also consider emerging treatment options, including calcitonin gene-related peptide antibodies, non-invasive vagus nerve stimulation, sphenopalatine ganglion stimulation and somatostatin receptor agonists, discuss how evidence from trials of these emerging treatments provides insights into the pathophysiology of cluster headache and highlight areas for future research.
Key points
-
Cluster headache is a debilitating primary headache disorder with two subtypes — episodic and chronic — that are currently defined according to a temporal cut-off.
-
Cluster headache pathogenesis involves complex interactions between the trigeminovascular pathway, trigeminal autonomic reflex, hypothalamus and the neuropeptides calcitonin gene-related peptide and pituitary adenylate cyclase-activating polypeptide 38.
-
Emerging therapies in cluster headache include calcitonin gene-related peptide monoclonal antibodies, non-invasive vagus nerve stimulation and sphenopalatine ganglion stimulation.
-
Clinical studies of these emerging treatments have highlighted differences between episodic and chronic cluster headache that imply different underlying mechanisms that could be used to distinguish them.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Russell, M. B. Epidemiology and genetics of cluster headache. Lancet Neurol. 3, 279–283 (2004).
Wallin, M. T. et al. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 269–285 (2019).
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38, 1–211 (2018).
Burish, M. J., Pearson, S. M., Shapiro, R. E., Zhang, W. & Schor, L. I. Cluster headache is one of the most intensely painful human conditions: results from the International Cluster Headache Questionnaire. Headache 61, 117–124 (2021).
Goadsby, P. J. et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol. Rev. 97, 553–622 (2017).
May, A. & Goadsby, P. J. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J. Cereb. Blood Flow. Metab. 19, 115–127 (1999).
Goadsby, P. J. & Lipton, R. B. A review of paroxysmal hemicranias, SUNCT syndrome and other short-lasting headaches with autonomic feature, including new cases. Brain 120, 193–209 (1997). This review was the first to coin the term trigeminal autonomic cephalalgias to describe primary unilateral headaches with ipsilateral cranial autonomic symptoms.
Hoffmann, J. & May, A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 17, 75–83 (2018).
O’Connor, T. P. & van der Kooy, D. Pattern of intracranial and extracranial projections of trigeminal ganglion cells. J. Neurosci. 6, 2200–2207 (1986).
Feindel, W., Penfield, W. & McNaughton, F. The tentorial nerves and localization of intracranial pain in man. Neurology 10, 555–563 (1960).
McNaughton, F. & Feindel, W. Innervation of intracranial structures: a reappraisal in Physiological Aspects of Clinical Neurology (ed. Rose, F. C.) 279–293 (Blackwell, 1977).
Fontaine, D. et al. Dural and pial pain-sensitive structures in humans: new inputs from awake craniotomies. Brain 141, 1040–1048 (2018).
Goadsby, P. J. & Hoskin, K. L. The distribution of trigeminovascular afferents in the nonhuman primate brain Macaca nemestrina: a c-fos immunocytochemical study. J. Anat. 190, 367–375 (1997).
Hoskin, K. L., Zagami, A. S. & Goadsby, P. J. Stimulation of the middle meningeal artery leads to Fos expression in the trigeminocervical nucleus: a comparative study of monkey and cat. J. Anat. 194, 579–588 (1999).
Arbab, M. A., Wiklund, L. & Svendgaard, N. A. Origin and distribution of cerebral vascular innervation from superior cervical, trigeminal and spinal ganglia investigated with retrograde and anterograde WGA-HRP tracing in the rat. Neuroscience 19, 695–708 (1986).
Arbab, M. A., Delgado, T., Wiklund, L. & Svendgaard, N. A. Brain stem terminations of the trigeminal and upper spinal ganglia innervation of the cerebrovascular system: WGA-HRP transganglionic study. J. Cereb. Blood Flow. Metab. 8, 54–63 (1988).
Zagami, A. S. & Lambert, G. A. Stimulation of cranial vessels excites nociceptive neurones in several thalamic nuclei of the cat. Exp. Brain Res. 81, 552–566 (1990).
Zagami, A. S. & Goadsby, P. J. Stimulation of the superior sagittal sinus increases metabolic activity in cat thalamus in New Advances in Headache Research: 2 (ed. Rose, F. C.) 169–171 (Smith-Gordon, 1991).
O’Connor, T. P. & van der Kooy, D. Enrichment of a vasoactive neuropeptide (calcitonin gene related peptide) in the trigeminal sensory projection to the intracranial arteries. J. Neurosci. 8, 2468–2476 (1988).
Zagami, A. S., Goadsby, P. J. & Edvinsson, L. Stimulation of the superior sagittal sinus in the cat causes release of vasoactive peptides. Neuropeptides 16, 69–75 (1990).
Liu-Chen, L. Y., Gillespie, S. A., Norregaard, T. V. & Moskowitz, M. A. Co-localization of retrogradely transported wheat germ agglutinin and the putative neurotransmitter substance P within trigeminal ganglion cells projecting to cat middle cerebral artery. J. Comp. Neurol. 225, 187–192 (1984).
Marfurt, C. F. The central projections of trigeminal primary afferent neurons in the cat as determined by the tranganglionic transport of horseradish peroxidase. J. Comp. Neurol. 203, 785–798 (1981).
Penfield, W. & McNaughton, F. Dural headache and innervation of the dura mater. Arch. Neurol. Psychiatry 44, 43–75 (1940).
Ray, B. S. & Wolff, H. G. Experimental studies on headache: pain-sensitive structures of the head and their significance in headache. Arch. Surg. 41, 813–856 (1940).
Johnston, M. M., Jordan, S. E. & Charles, A. C. Pain referral patterns of the C1 to C3 nerves: implications for headache disorders. Ann. Neurol. 74, 145–148 (2013).
Spencer, S. E., Sawyer, W. B., Wada, H., Platt, K. B. & Loewy, A. D. CNS projections to the pterygopalatine parasympathetic preganglionic neurons in the rat: a retrograde transneuronal viral cell body labeling study. Brain Res. 534, 149–169 (1990).
Knight, Y. E. et al. Patterns of fos expression in the rostral medulla and caudal pons evoked by noxious craniovascular stimulation and periaqueductal gray stimulation in the cat. Brain Res. 1045, 1–11 (2005).
Nakai, M., Tamaki, K., Ogata, J., Matsui, Y. & Maeda, M. Parasympathetic cerebrovasodilator center of the facial nerve. Circ. Res. 72, 470–475 (1993).
Goadsby, P. J., Lambert, G. A. & Lance, J. W. Effects of locus coeruleus stimulation on carotid vascular resistance in the cat. Brain Res. 278, 175–183 (1983).
Goadsby, P. J., Lambert, G. A. & Lance, J. W. The peripheral pathway for extracranial vasodilatation in the cat. J. Auton. Nerv. Syst. 10, 145–155 (1984).
Goadsby, P. J. Sphenopalatine ganglion stimulation increases regional cerebral blood flow independent of glucose utilization in the cat. Brain Res. 506, 145–148 (1990).
Goadsby, P. J., Uddman, R. & Edvinsson, L. Cerebral vasodilatation in the cat involves nitric oxide from parasympathetic nerves. Brain Res. 707, 110–118 (1996).
Jansen-Olesen, I., Goadsby, P. J., Uddman, R. & Edvinsson, L. Vasoactive intestinal peptide (VIP) like peptides in the cerebral circulation of the cat. J. Auton. Nerv. Syst. 49 (Suppl.), S97–S103 (1994).
Goadsby, P. J. & Shelley, S. High-frequency stimulation of the facial nerve results in local cortical release of vasoactive intestinal polypeptide in the anesthetised cat. Neurosci. Lett. 112, 282–289 (1990).
Csati, A., Tajti, J., Tuka, B., Edvinsson, L. & Warfvinge, K. Calcitonin gene-related peptide and its receptor components in the human sphenopalatine ganglion – interaction with the sensory system. Brain Res. 1435, 29–39 (2012).
Uddman, R., Goadsby, P. J., Jansen, I. & Edvinsson, L. PACAP, a VIP-like peptide: immunohistochemical localization and effect upon cat pial arteries and cerebral blood flow. J. Cereb. Blood Flow. Metab. 13, 291–297 (1993).
Möller, M., Haji, A. A., Hoffmann, J. & May, A. Peripheral provocation of cranial autonomic symptoms is not sufficient to trigger cluster headache attacks. Cephalalgia 38, 1498–1502 (2018).
Guo, S. et al. Cranial parasympathetic activation induces autonomic symptoms but no cluster headache attacks. Cephalalgia 38, 1418–1428 (2018).
Brain, S. D., Williams, T. J., Tippins, J. R., Morris, H. R. & MacIntyre, I. Calcitonin gene-related peptide is a potent vasodilator. Nature 313, 54–56 (1985).
Storer, R. J., Akerman, S. & Goadsby, P. J. Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br. J. Pharmacol. 142, 1171–1181 (2004).
Russell, F. A., King, R., Smillie, S. J., Kodji, X. & Brain, S. D. Calcitonin gene-related peptide: physiology and pathophysiology. Physiol. Rev. 94, 1099–1142 (2014).
Edvinsson, L., Mulder, H., Goadsby, P. J. & Uddman, R. Calcitonin gene-related peptide and nitric oxide in the trigeminal ganglion: cerebral vasodilatation from trigeminal nerve stimulation involves mainly calcitonin gene-related peptide. J. Auton. Nerv. Syst. 70, 15–22 (1998).
Eftekhari, S. & Edvinsson, L. Calcitonin gene-related peptide (CGRP) and its receptor components in human and rat spinal trigeminal nucleus and spinal cord at C1-level. BMC Neurosci. 12, 112 (2011).
McLatchie, L. M. et al. RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor. Nature 393, 333–339 (1998).
Russo, A. F. Calcitonin gene-related peptide (CGRP): a new target for migraine. Annu. Rev. Pharmacol. Toxicol. 55, 533–552 (2015).
Edvinsson, L., Haanes, K. A., Warfvinge, K. & Krause, D. N. CGRP as the target of new migraine therapies — successful translation from bench to clinic. Nat. Rev. Neurol. 14, 338–350 (2018).
Goadsby, P. J. & Edvinsson, L. Human in vivo evidence for trigeminovascular activation in cluster headache. Neuropeptide changes and effects of acute attacks therapies. Brain 117, 427–434 (1994). This seminal study was the first to associate CGRP with the pathogenesis of cluster headache by showing that CGRP levels increase in the serum during a cluster headache attack and normalize after treatment and resolution of the attack with sumatriptan.
Fanciullacci, M., Alessandri, M., Figini, M., Geppetti, P. & Michelacci, S. Increase in plasma calcitonin gene-related peptide from the extracerebral circulation during nitroglycerin-induced cluster headache attack. Pain 60, 119–123 (1995).
Fanciullacci, M., Alessandri, M., Sicuteri, R. & Marabini, S. Responsiveness of the trigeminovascular system to nitroglycerine in cluster headache patients. Brain 120, 283–288 (1997).
Vollesen, A. L. H. et al. Effect of infusion of calcitonin gene-related peptide on cluster headache attacks: a randomized clinical trial. JAMA Neurol. 75, 1187–1197 (2018). This study demonstrated that CGRP induces attacks in patients with episodic cluster headache when in bout and in patients with chronic cluster headache with frequent attacks in the preceding 30 days, but not in patients with episodic cluster headache out of bout.
Snoer, A. et al. Calcitonin-gene related peptide and disease activity in cluster headache. Cephalalgia 39, 575–584 (2019).
Miyata, A. et al. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem. Biophys. Res. Commun. 164, 567–574 (1989).
Steinberg, A., Frederiksen, S. D., Blixt, F. W., Warfvinge, K. & Edvinsson, L. Expression of messenger molecules and receptors in rat and human sphenopalatine ganglion indicating therapeutic targets. J. Headache Pain. 17, 78 (2016).
Laburthe, M., Couvineau, A. & Tan, V. Class II G protein-coupled receptors for VIP and PACAP: structure, models of activation and pharmacology. Peptides 28, 1631–1639 (2007).
Dickson, L. & Finlayson, K. VPAC and PAC receptors: from ligands to function. Pharmacol. Ther. 121, 294–316 (2009).
Jansen-Olesen, I. et al. PACAP-38 but not VIP induces release of CGRP from trigeminal nucleus caudalis via a receptor distinct from the PAC1 receptor. Neuropeptides 48, 53–64 (2014).
Hannibal, J. et al. Pituitary adenylate cyclase-activating peptide (PACAP) in the retinohypothalamic tract: a potential daytime regulator of the biological clock. J. Neurosci. 17, 2637–2644 (1997).
Tuka, B. et al. Release of PACAP-38 in episodic cluster headache patients – an exploratory study. J. Headache Pain 17, 69 (2016).
Saper, C. B., Scammell, T. E. & Lu, J. Hypothalamic regulation of sleep and circadian rhythms. Nature 437, 1257–1263 (2005).
Settle, M. The hypothalamus. Neonatal Netw. 19, 9–14 (2000).
Buijs, R. M. The autonomic nervous system: a balancing act. Handb. Clin. Neurol. 117, 1–11 (2013).
Bartsch, T., Levy, M. J., Knight, Y. E. & Goadsby, P. J. Inhibition of nociceptive dural input in the trigeminal nucleus caudalis by somatostatin receptor blockade in the posterior hypothalamus. Pain 117, 30–39 (2005).
Holland, P. & Goadsby, P. J. The hypothalamic orexinergic system: pain and primary headaches. Headache 47, 951–962 (2007).
Malick, A., Strassman, R. M. & Burstein, R. Trigeminohypothalamic and reticulohypothalamic tract neurons in the upper cervical spinal cord and caudal medulla of the rat. J. Neurophysiol. 84, 2078–2112 (2000).
Kunkle, E. C., Pfieffer J, J. B., Wilhoit, W. M. & Hamrick J, L. W. Recurrent brief headache in “cluster” pattern. Trans. Am. Neurol. Assoc. 27, 240–243 (1952). The first description of patients with cluster headache having bouts that cluster through the year.
Kudrow, L. The cyclic relationship of natural illumination to cluster period frequency. Cephalalgia 7 (Suppl. 6), 76–78 (1987). This is the first study to show the relationship between photoperiodism and bout occurrence.
Waldenlind, E., Gustafsson, S. A., Ekbom, K. & Wetterberg, L. Circadian secretion of cortisol and melatonin in cluster headache during active cluster periods and remission. J. Neurol. Neurosurg. Psychiatry 50, 207–213 (1987).
Leone, M. & Bussone, G. A review of hormonal findings in cluster headache. Evidence for hypothalamic involvement. Cephalalgia 13, 309–317 (1993).
Kudrow, L. Plasma testosterone levels in cluster headache preliminary results. Headache 16, 28–31 (1976).
Holland, P. R. & Goadsby, P. J. Cluster headache, hypothalamus, and orexin. Curr. Pain. Headache Rep. 13, 147–154 (2009).
May, A., Bahra, A., Büchel, C., Frackowiak, R. S. J. & Goadsby, P. J. Hypothalamic activation in cluster headache attacks. Lancet 352, 275–278 (1998). This seminal study presents neuroimaging findings of ipsilateral hypothalamic activation in nitroglycerin induced cluster headache attacks.
Robert, C. et al. Paraventricular hypothalamic regulation of trigeminovascular mechanisms involved in headaches. J. Neurosci. 33, 8827–8840 (2013).
Matharu, M. S., Levy, M. J., Meeran, K. & Goadsby, P. J. Subcutaneous octreotide in cluster headache: randomized placebo-controlled double-blind crossover study. Ann. Neurol. 56, 488–494 (2004).
Hosoya, Y., Matsushita, M. & Sugiura, Y. A direct hypothalamic projection to the superior salivatory nucleus neurons in the rat. A study using anterograde autoradiographic and retrograde HRP methods. Brain Res. 266, 329–333 (1983).
Hosoya, Y., Sugiura, Y., Ito, R. & Kohno, K. Descending projections from the hypothalamic paraventricular nucleus to the A5 area, including the superior salivatory nucleus, in the rat. Exp. Brain Res. 82, 513–518 (1990).
Li, C. et al. Projections from the hypothalamic paraventricular nucleus and the nucleus of the solitary tract to prechoroidal neurons in the superior salivatory nucleus: pathways controlling rodent choroidal blood flow. Brain Res. 1358, 123–139 (2010).
Akerman, S., Holland, P. R., Lasalandra, M. P. & Goadsby, P. J. Oxygen inhibits neuronal activation in the trigeminocervical complex after stimulation of trigeminal autonomic reflex, but not during direct dural activation of trigeminal afferents. Headache. 49, 1131–1143 (2009). This important animal study showed that oxygen acts on the trigeminal autonomic reflex rather than the trigeminovascular system.
Ibuka, N. & Kawamura, H. Loss of circadian rhythm in sleep-wakefulness cycle in the rat by suprachiasmatic nucleus lesions. Brain Res. 96, 76–81 (1975).
Hastings, M. H., Maywood, E. S. & Brancaccio, M. Generation of circadian rhythms in the suprachiasmatic nucleus. Nat. Rev. Neurosci. 19, 453–469 (2018).
Wurtman, R. J., Axelrod, J. & Phillips, L. S. Melatonin synthesis in the pineal gland: control by light. Science 142, 1071–1073 (1963).
Chazot, G. et al. A chronobiological study of melatonin, cortisol growth hormone and prolactin secretion in cluster headache. Cephalalgia 4, 213–220 (1984).
Leone, M. et al. Twenty-four-hour melatonin and cortisol plasma levels in relation to timing of cluster headache. Cephalalgia 15, 224–229 (1995).
Waldenlind, E. et al. Lowered circannual urinary melatonin concentrations in episodic cluster headache. Cephalalgia 14, 199–204 (1994).
Coomans, C. P., Ramkisoensing, A. & Meijer, J. H. The suprachiasmatic nuclei as a seasonal clock. Front. Neuroendocrinol. 37, 29–42 (2015).
Hofman, M. A., Purba, J. S. & Swaab, D. F. Annual variations in the vasopressin neuron population of the human suprachiasmatic nucleus. Neuroscience 53, 1103–1112 (1993).
Rozen, T. D. & Fishman, R. S. Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 52, 99–113 (2012).
Manzoni, G. C. et al. Cluster headache–clinical findings in 180 patients. Cephalalgia 3, 21–30 (1983).
Gaul, C. et al. Differences in clinical characteristics and frequency of accompanying migraine features in episodic and chronic cluster headache. Cephalalgia 32, 571–577 (2012).
Barloese, M. et al. Sleep and chronobiology in cluster headache. Cephalalgia 35, 969–978 (2015).
Lin, K. H. et al. Cluster headache in the Taiwanese – a clinic-based study. Cephalalgia 24, 631–638 (2004).
Ofte, H. K., Berg, D. H., Bekkelund, S. I. & Alstadhaug, K. B. Insomnia and periodicity of headache in an arctic cluster headache population. Headache 53, 1602–1612 (2013).
May, A. et al. Experimental cranial pain elicited by capsaicin: a PET study. Pain 74, 61–66 (1998).
Wei, D. Y., Khalil, M. & Goadsby, P. J. Managing cluster headache. Pract. Neurol. 19, 521–528 (2019).
May, A. et al. Cluster headache. Nat. reviews. Dis. Prim. 4, 18006 (2018).
The Sumatriptan Cluster Headache Study Group. Treatment of acute cluster headache with sumatriptan. N. Engl. J. Med. 325, 322–326 (1991).
Cohen, A. S., Burns, B. & Goadsby, P. J. High-flow oxygen for treatment of cluster headache. JAMA 302, 2451–2457 (2009).
Silberstein, S. D. et al. Non-invasive vagus nerve stimulation for the ACute treatment of cluster headache: findings from the randomized, double-blind, sham-controlled ACT1 study. Headache 56, 1317–1332 (2016).
Goadsby, P. J. et al. Non-invasive vagus nerve stimulation for the acute treatment of episodic and chronic cluster headache: A randomized, double-blind, sham-controlled ACT2 study. Cephalalgia 38, 959–969 (2018).
van Vliet, J. A. et al. Intranasal sumatriptan in cluster headache: randomized placebo-controlled double-blind study. Neurology 60, 630–633 (2003).
Cittadini, E. et al. Effectiveness of intranasal zolmitriptan in acute cluster headache: a randomized, placebo-controlled, double-blind crossover study. Arch. Neurol. 63, 1537–1542 (2006).
Rapoport, A. M. et al. Zolmitriptan nasal spray in the acute treatment of cluster headache: a double-blind study. Neurology 69, 821–826 (2007).
Ekbom, K. et al. Subcutaneous sumatriptan in the acute treatment of cluster headache: a dose comparison study. The Sumatriptan Cluster Headache Study Group. Acta Neurol. Scand. 88, 63–69 (1993).
Ekbom, K. et al. Cluster headache attacks treated for up to three months with subcutaneous sumatriptan (6 mg). Sumatriptan Cluster Headache Long-term Study Group. Cephalalgia 15, 230–236 (1995).
Göbel, H., Lindner, V., Heinze, A., Ribbat, M. & Deuschl, G. Acute therapy for cluster headache with sumatriptan: findings of a one-year long-term study. Neurology 51, 908–911 (1998).
Paemeleire, K., Bahra, A., Evers, S., Matharu, M. S. & Goadsby, P. J. Medication-overuse headache in patients with cluster headache. Neurology 67, 109–113 (2006).
Diener, H. C. et al. Pathophysiology, prevention, and treatment of medication overuse headache. Lancet Neurol. 18, 891–902 (2019).
Bahra, A. et al. Oral zolmitriptan is effective in the acute treatment of cluster headache. Neurology 54, 1832–1839 (2000).
Goadsby, P. J. The pharmacology of headache. Prog. Neurobiol. 62, 509–525 (2000).
Kaube, H., Hoskin, K. L. & Goadsby, P. J. Inhibition by sumatriptan of central trigeminal neurones only after blood-brain barrier disruption. Br. J. Pharmacol. 109, 788–792 (1993).
Levy, D., Jakubowski, M. & Burstein, R. Disruption of communication between peripheral and central trigeminovascular neurons mediates the antimigraine action of 5HT 1B/1D receptor agonists. Proc. Natl Acad. Sci. USA 101, 4274–4279 (2004).
Goadsby, P. J. & Edvinsson, L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann. Neurol. 33, 48–56 (1993).
Shields, K. G. & Goadsby, P. J. Serotonin receptors modulate trigeminovascular responses in ventroposteromedial nucleus of thalamus: a migraine target? Neurobiol. Dis. 23, 491–501 (2006).
Deen, M. et al. Association between sumatriptan treatment during a migraine attack and central 5-HT1B receptor binding. JAMA Neurol. 76, 834–840 (2019).
Muzzi, M. et al. Ultra-rapid brain uptake of subcutaneous sumatriptan in the rat: implication for cluster headache treatment. Cephalalgia 40, 330–336 (2020).
Monstad, I. et al. Preemptive oral treatment with sumatriptan during a cluster period. Headache 35, 607–613 (1995).
Horton, B. T. Histaminic cephalgia. J. Lancet 72, 92–98 (1952).
Kudrow, L. Response of cluster headache attacks to oxygen inhalation. Headache 21, 1–4 (1981).
Fogan, L. Treatment of cluster headache. A double-blind comparison of oxygen v air inhalation. Arch. Neurol. 42, 362–363 (1985).
Petersen, A. S., Barloese, M. C., Lund, N. L. & Jensen, R. H. Oxygen therapy for cluster headache. A mask comparison trial. A single-blinded, placebo-controlled, crossover study. Cephalalgia 37, 214–224 (2016).
Mirzai, R., Chang, C., Greenspan, A. & Gershwin, M. E. The pathogenesis of osteonecrosis and the relationships to corticosteroids. J. Asthma 36, 77–95 (1999).
Jammes, J. L. The treatment of cluster headaches with prednisone. Dis. Nerv. Syst. 36, 375–376 (1975).
Couch, J. R. Jr. & Ziegler, D. K. Prednisone therapy for cluster headache. Headache 18, 219–221 (1978).
Holle, D. et al. Study protocol of Prednisone in episodic Cluster Headache (PredCH): a randomized, double-blind, placebo-controlled parallel group trial to evaluate the efficacy and safety of oral prednisone as an add-on therapy in the prophylactic treatment of episodic cluster headache with verapamil. BMC Neurol. 13, 99 (2013).
Obermann, M. & Holle, D. Prednisone in short-term prevention of episodic cluster headache [abstract]. Neurology 94 (Suppl. 15), 4645 (2020).
Neeb, L., Hellen, P., Hoffmann, J., Dirnagl, U. & Reuter, U. Methylprednisolone blocks interleukin 1 beta induced calcitonin gene related peptide release in trigeminal ganglia cells. J. Headache Pain 17, 19 (2016).
Neeb, L. et al. Corticosteroids alter CGRP and melatonin release in cluster headache episodes. Cephalalgia 35, 317–326 (2015).
Anthony, M. in Migraine: Clinical and Research Advances (ed. Rose F. C.) 169–173 (Karger, 1985).
Ambrosini, A. et al. Suboccipital injection with a mixture of rapid- and long-acting steroids in cluster headache: a double-blind placebo-controlled study. Pain 118, 92–96 (2005).
Afridi, S. K., Shields, K. G., Bhola, R. & Goadsby, P. J. Greater occipital nerve injection in primary headache syndromes – prolonged effects from a single injection. Pain 122, 126–129 (2006).
Leroux, E. et al. Suboccipital steroid injections for transitional treatment of patients with more than two cluster headache attacks per day: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 10, 891–897 (2011).
Gantenbein, A. R., Lutz, N. J., Riederer, F. & Sándor, P. S. Efficacy and safety of 121 injections of the greater occipital nerve in episodic and chronic cluster headache. Cephalalgia 32, 630–634 (2012).
Lambru, G. et al. Greater occipital nerve blocks in chronic cluster headache: a prospective open-label study. Eur. J. Neurol. 21, 338–343 (2014).
Gaul, C. et al. Efficacy and safety of a single occipital nerve blockade in episodic and chronic cluster headache: a prospective observational study. Cephalalgia 37, 873–880 (2017).
Shields, K. G., Levy, M. J. & Goadsby, P. J. Alopecia and cutaneous atrophy after greater occipital nerve infiltration with corticosteroid. Neurology 63, 2193–2194 (2004).
Wei, J. & Robbins, M. S. Greater occipital nerve injection versus oral steroids for short term prophylaxis of cluster headache: a retrospective comparative study. Headache 58, 852–858 (2018).
Bartsch, T. & Goadsby, P. J. Stimulation of the greater occipital nerve induces increased central excitability of dural afferent input. Brain 125, 1496–1509 (2002).
Goadsby, P. J., Knight, Y. E. & Hoskin, K. L. Stimulation of the greater occipital nerve increases metabolic activity in the trigeminal nucleus caudalis and cervical dorsal horn of the cat. Pain 73, 23–28 (1997).
Bartsch, T. & Goadsby, P. J. The trigeminocervical complex and migraine: current concepts and synthesis. Curr. Pain Headache Rep. 7, 371–376 (2003).
Meyer, J. S. & Hardenberg, J. Clinical effectiveness of calcium entry blockers in prophylactic treatment of migraine and cluster headaches. Headache 23, 266–277 (1983).
Jónsdóttir, M., Meyer, J. S. & Rogers, R. L. Efficacy, side effects and tolerance compared during headache treatment with three different calcium blockers. Headache 27, 364–369 (1987).
Gabai, I. J. & Spierings, E. L. Prophylactic treatment of cluster headache with verapamil. Headache 29, 167–168 (1989).
Leone, M. et al. Verapamil in the prophylaxis of episodic cluster headache: a double-blind study versus placebo. Neurology 54, 1382–1385 (2000).
Bussone, G. et al. Double blind comparison of lithium and verapamil in cluster headache prophylaxis. Headache 30, 411–417 (1990).
Cohen, A. S., Matharu, M. S. & Goadsby, P. J. Electrocardiographic abnormalities in patients with cluster headache on verapamil therapy. Neurology 69, 668–675 (2007).
Blau, J. N. & Engel, H. O. Individualizing treatment with verapamil for cluster headache patients. Headache 44, 1013–1018 (2004).
Lanteri-Minet, M., Silhol, F., Piano, V. & Donnet, A. Cardiac safety in cluster headache patients using the very high dose of verapamil (≥720 mg/day). J. Headache Pain 12, 173–176 (2011).
Matharu, M. S., van Vliet, J. A., Ferrari, M. D. & Goadsby, P. J. Verapamil induced gingival enlargement in cluster headache. J. Neurol. Neurosurg. Psychiatry 76, 124–127 (2005).
Dougall, H. T. & McLay, J. A comparative review of the adverse effects of calcium antagonists. Drug Saf. 15, 91–106 (1996).
King, B. D. et al. Impotence during therapy with verapamil. Arch. Intern. Med. 143, 1248–1249 (1983).
Tsien, R. W., Lipscombe, D., Madison, D. V., Bley, K. R. & Fox, A. P. Multiple types of neuronal calcium channels and their selective modulation. Trends Neurosci. 11, 431–438 (1988).
Westenbroek, R. E. et al. Immunochemical identification and subcellular distribution of the alpha 1A subunits of brain calcium channels. J. Neurosci. 15, 6403–6418 (1995).
Kim, H. C. & Chung, M. K. Voltage-dependent sodium and calcium currents in acutely isolated adult rat trigeminal root ganglion neurons. J. Neurophysiol. 81, 1123–1134 (1999).
Akerman, S., Williamson, D. J. & Goadsby, P. J. Voltage-dependent calcium channels are involved in neurogenic dural vasodilatation via a presynaptic transmitter release mechanism. Br. J. Pharmacol. 140, 558–566 (2003).
Lubberink, M. et al. Evaluation of tracer kinetic models for quantification of P-glycoprotein function using (R)-[11C]verapamil and PET. J. Cereb. Blood Flow. Metab. 27, 424–433 (2007).
Colwell, C. S. Circadian modulation of calcium levels in cells in the suprachiasmatic nucleus. Eur. J. Neurosci. 12, 571–576 (2000).
Biel, M., Wahl-Schott, C., Michalakis, S. & Zong, X. Hyperpolarization-activated cation channels: from genes to function. Physiol. Rev. 89, 847–885 (2009).
Vila-Pueyo, M., Bojarowska, Z., Goadsby, P. J. & Holland, R. R. Mechanisms of action of verapamil in preclinical model of cluster headache. Cephalalgia 40, 3–17 (2020). This animal study demonstrated the novel mechanism of action of verapamil on hyperpolarization-activated cyclic nucleotide-gated channels.
Ekbom, K. Lithium for cluster headache: review of the literature and preliminary results of long-term treatment. Headache 21, 132–139 (1981).
Steiner, T., Hering, R., Couturier, E., Davies, P. & Whitmarsh, T. Double-blind placebo-controlled trial of lithium in episodic cluster headache. Cephalalgia 17, 673–675 (1997).
Kudrow, L. Lithium prophylaxis for chronic cluster headache. Headache 17, 15–18 (1977).
Becker, W. J. Cluster headache: conventional pharmacological management. Headache 53, 1191–1196 (2013).
Ekbom, K. Litium vid kroniska symptom av cluster headache. Opusc. Medica 19, 148–156 (1974).
Fanciullacci, M., Pietrini, U., Boccuni, M., Gatto, G. & Cangi, F. Does lithium balance the neuronal bilateral asymmetries in cluster headache? Cephalalgia 3 (Suppl. 1), 85–87 (1983).
Vincent, M. B. Lithium inhibits substance P and vasoactive intestinal peptide-induced relaxations on isolated porcine ophthalmic artery. Headache 32, 335–339 (1992).
Moreira, J. & Geoffroy, P. A. Lithium and bipolar disorder: impacts from molecular to behavioural circadian rhythms. Chronobiol. Int. 33, 351–373 (2016).
Chazot, G., Claustrat, B., Brun, J. & Zaidan, R. Effects on the patterns of melatonin and cortisol in cluster headache of a single administration of lithium at 7.00 p.m. daily over one week: a preliminary report. Pharmacopsychiatry 20, 222–223 (1987).
Leone, M. et al. Dexamethasone suppression test, melatonin and TRH-test in cluster headache. Ital. J. Neurol. Sci. 13, 227–232 (1992).
Leone, M. et al. Abnormal 24-hour urinary excretory pattern of 6-sulphatoxymelatonin in both phases of cluster headache. Cephalalgia 18, 664–667 (1998).
Leone, M., D’Amico, D., Moschiano, F., Fraschini, F. & Bussone, G. Melatonin versus placebo in the prophylaxis of cluster headache: a double-blind pilot study with parallel groups. Cephalalgia 16, 494–496 (1996).
Pringsheim, T., Magnoux, E., Dobson, C. F., Hamel, E. & Aube, M. Melatonin as adjunctive therapy in the prophylaxis of cluster headache: a pilot study. Headache 42, 787–792 (2002).
Peres, M. F. & Rozen, T. D. Melatonin in the preventive treatment of chronic cluster headache. Cephalalgia 21, 993–995 (2001).
Robbins, M. S., Starling, A. J., Pringsheim, T. M., Becker, W. J. & Schwedt, T. J. Treatment of cluster headache: the American Headache Society evidence-based guidelines. Headache 56, 1093–1106 (2016).
Gelfand, A. A. & Goadsby, P. J. The role of melatonin in the treatment of primary headache disorders. Headache 56, 1257–1266 (2016).
Mantovani, M. et al. Mechanisms involved in the antinociception caused by melatonin in mice. J. Pineal Res. 41, 382–389 (2006).
El-Shenawy, S. M., Abdel-Salam, O. M., Baiuomy, A. R., El-Batran, S. & Arbid, M. S. Studies on the anti-inflammatory and anti-nociceptive effects of melatonin in the rat. Pharmacol. Res. 46, 235–243 (2002).
Ambriz-Tututi, M., Rocha-González, H. I., Cruz, S. L. & Granados-Soto, V. Melatonin: a hormone that modulates pain. Life Sci. 84, 489–498 (2009).
Srinivasan, V. et al. Melatonin in antinociception: its therapeutic applications. Curr. Neuropharmacol. 10, 167–178 (2012).
Viswanathan, M. Melatonin inhibits calcitonin gene-related peptide-induced vasodilation and increase in cAMP in rat middle cerebral arteries. Eur. J. Pharmacol. 415, 247–250 (2001).
da Cunha Tanuri, F., Amado, D., Filho, I. & Peres, M. Melatonin reverts CGRP expression induced by capsaicin. Headache Med. 10, 24–28 (2019).
Wheeler, S. D. & Carrazana, E. J. Topiramate-treated cluster headache. Neurology 53, 234–236 (1999).
Forderreuther, S., Mayer, M. & Straube, A. Treatment of cluster headache with topiramate: effects and side-effects in five patients. Cephalalgia 22, 186–189 (2002).
Lainez, M. J. et al. Topiramate in the prophylactic treatment of cluster headache. Headache 43, 784–789 (2003).
Huang, W. Y., Lo, M. C., Wang, S. J., Tsai, J. J. & Wu, H. M. Topiramate in prevention of cluster headache in the Taiwanese. Neurol. India 58, 284–287 (2010).
Leone, M. et al. Topiramate in cluster headache prophylaxis: an open trial. Cephalalgia 23, 1001–1002 (2003).
Pascual, J., Lainez, M. J., Dodick, D. & Hering-Hanit, R. Antiepileptic drugs for the treatment of chronic and episodic cluster headache: a review. Headache 47, 81–89 (2007).
Rosenfeld, W. E. Topiramate: a review of preclinical, pharmacokinetic, and clinical data. Clin. Ther. 19, 1294–1308 (1997).
Storer, R. J. & Goadsby, P. J. Topiramate inhibits trigeminovascular neurons in the cat. Cephalalgia 24, 1049–1056 (2004).
Storer, R. J. & Goadsby, P. J. Topiramate is likely to act outside of the trigeminocervical complex. Cephalalgia 33, 291–300 (2013).
Andreou, A. P. & Goadsby, P. J. Topiramate in the treatment of migraine: a kainate (glutamate) receptor antagonist within the trigeminothalamic pathway. Cephalalgia 31, 1343–1358 (2011).
Hoffmann, J. & Charles, A. Glutamate and its receptors as therapeutic targets for migraine. Neurotherapeutics 15, 361–370 (2018).
Poulsen, C. F. et al. Modulation by topiramate of AMPA and kainate mediated calcium influx in cultured cerebral cortical, hippocampal and cerebellar neurons. Neurochem. Res. 29, 275–282 (2004).
Hebestreit, J. M. & May, A. Topiramate modulates trigeminal pain processing in thalamo-cortical networks in humans after single dose administration. PLOS ONE 12, e0184406 (2017).
Akerman, S. & Goadsby, P. J. Topiramate inhibits trigeminovascular activation: an intravital microscopy study. Br. J. Pharmacol. 146, 7–14 (2005).
Benschop, R. J. et al. Development of a novel antibody to calcitonin gene-related peptide for the treatment of osteoarthritis-related pain. Osteoarthr. Cartil. 22, 578–585 (2014).
Goadsby, P. J. et al. Trial of galcanezumab in prevention of episodic cluster headache. N. Engl. J. Med. 381, 132–141 (2019). The results of the first phase III randomized, placebo-controlled trial to demonstrate efficacy of a CGRP monoclonal antibody in the prevention of episodic cluster headache.
Dodick, D. W. et al. Phase 3 randomized, placebo-controlled study of galcanezumab in patients with chronic cluster headache: results from 3-month double-blind treatment. Cephalalgia 40, 935–948 (2020). This negative study highlighted the possible mechanistic difference between episodic and chronic cluster headache.
Lipton RB, D. H. et al. Efficacy and safety of fremanezumab for the prevention of episodic cluster headache: results of a randomized, double-blind, placebo-controlled, phase 3 study. Cephalalgia 39, 358–359 (2019).
Bigal, M. E., Walter, S. & Rapoport, A. M. Therapeutic antibodies against CGRP or its receptor. Br. J. Clin. Pharmacol. 79, 886–895 (2015).
Felgenhauer, K. Protein size and cerebrospinal fluid composition. Klin. Wochenschr. 52, 1158–1164 (1974).
Johnson, K. W., Morin, S. M., Wroblewski, V. J. & Johnson, M. P. Peripheral and central nervous system distribution of the CGRP neutralizing antibody [(125)I] galcanezumab in male rats. Cephalalgia 39, 1241–1248 (2019).
Noseda, R. et al. Fluorescently-labeled fremanezumab is distributed to sensory and autonomic ganglia and the dura but not to the brain of rats with uncompromised blood brain barrier. Cephalalgia 40, 229–240 (2020).
Doods, H. et al. Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br. J. Pharmacol. 129, 420–423 (2000).
Christensen, S. L., Ernstsen, C., Olesen, J. & Kristensen, D. M. No central action of CGRP antagonising drugs in the GTN mouse model of migraine. Cephalalgia 40, 924–934 (2020).
Recober, A. et al. Role of calcitonin gene-related peptide in light-aversive behavior: implications for migraine. J. Neurosci. 29, 8798–8804 (2009).
Mauskop, A. Vagus nerve stimulation relieves chronic refractory migraine and cluster headaches. Cephalalgia 25, 82–86 (2005).
de Coo, I. F. et al. Differential efficacy of non-invasive vagus nerve stimulation for the acute treatment of episodic and chronic cluster headache: a meta-analysis. Cephalalgia 39, 967–977 (2019).
Gaul, C. et al. Non-invasive vagus nerve stimulation for PREVention and Acute treatment of chronic cluster headache (PREVA): a randomised controlled study. Cephalalgia 36, 534–546 (2016).
Nonis, R., D’Ostilio, K., Schoenen, J. & Magis, D. Evidence of activation of vagal afferents by non-invasive vagus nerve stimulation: an electrophysiological study in healthy volunteers. Cephalalgia 37, 1285–1293 (2017).
Frangos, E. & Komisaruk, B. R. Access to vagal projections via cutaneous electrical stimulation of the neck: fMRI evidence in healthy humans. Brain Stimul. 10, 19–27 (2017).
Juto, J. E. & Axelsson, M. Kinetic oscillation stimulation as treatment of non-allergic rhinitis: an RCT study. Acta Otolaryngol. 134, 506–512 (2014).
Moller, M., Schroeder, C. F. & May, A. Vagus nerve stimulation modulates the cranial trigeminal autonomic reflex. Ann. Neurol. 84, 886–892 (2018).
Schroeder, C. F., Moller, M. & May, A. nVNS sham significantly affects the trigeminal-autonomic reflex: a randomized controlled study. Neurology 93, e518–e521 (2019).
De Icco, R. et al. Peripheral vagal nerve stimulation modulates the nociceptive withdrawal reflex in healthy subjects: a randomized, cross-over, sham-controlled study. Cephalalgia 38, 1658–1664 (2018).
Akerman, S., Simon, B. & Romero-Reyes, M. Vagus nerve stimulation suppresses acute noxious activation of trigeminocervical neurons in animal models of primary headache. Neurobiol. Dis. 102, 96–104 (2017).
Goadsby, P. J. Pathophysiology of cluster headache: a trigeminal autonomic cephalgia. Lancet Neurol. 1, 251–257 (2002).
Schoenen, J. et al. Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment. Pathway CH-1: a randomized, sham-controlled study. Cephalalgia 33, 816–830 (2013).
Goadsby, P. J. et al. Safety and efficacy of sphenopalatine ganglion stimulation for chronic cluster headache: a double-blind, randomised controlled trial. Lancet Neurol. 18, 1081–1090 (2019).
Jürgens, T. P. et al. Long-term effectiveness of sphenopalatine ganglion stimulation for cluster headache. Cephalalgia 37, 423–434 (2017).
Barloese, M. et al. Sphenopalatine ganglion stimulation for cluster headache, results from a large, open-label European registry. J. Headache Pain 19, 6 (2018).
Ruskell, G. L. Orbital passage of pterygopalatine ganglion efferents to paranasal sinuses and nasal mucosa in man. Cell Tissues Organs 175, 223–228 (2003).
Ruskell, G. L. Distribution of pterygopalatine ganglion efferents to the lacrimal gland in man. Exp. Eye Res. 78, 329–335 (2004).
Suzuki, N. & Hardebo, J. E. The cerebrovascular parasympathetic innervation. Cerebrovasc. Brain Metab. Rev. 5, 33–46 (1993).
Schytz, H. W. et al. Experimental activation of the sphenopalatine ganglion provokes cluster-like attacks in humans. Cephalalgia 33, 831–841 (2013).
Sicuteri, F., Geppetti, P., Marabini, S. & Lembeck, F. Pain relief by somatostatin in attacks of cluster headache. Pain 18, 359–365 (1984).
Helyes, Z. et al. Anti-inflammatory effect of synthetic somatostatin analogues in the rat. Br. J. Pharmacol. 134, 1571–1579 (2001).
Caleri, D., Marabini, S., Panconesi, A. & Pietrini, U. A pharmacological approach to the analgesizing mechanism of somatostatin in cluster headache. Ric. Clin. Lab. 17, 155–162 (1987).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02619617 (2021).
Krisch, B. Hypothalamic and extrahypothalamic distribution of somatostatin-immunoreactive elements in the rat brain. Cell Tissue Res. 195, 499–513 (1978).
Fassler, J. E., O’Dorisio, T. M., Mekhjian, H. S. & Gaginella, T. S. Octreotide inhibits increases in short-circuit current induced in rat colon by VIP, substance P, serotonin and aminophylline. Regul. Pept. 29, 189–197 (1990).
Kapicioğlu, Z., Kalyoncu, I. N., Deger, O. & Can, G. Effect of a somatostatin analogue (SMS 201-995) on tear secretion in rats. Int. Ophthalmol. 22, 43–45 (1998).
Leone, M., Franzini, A. & Bussone, G. Stereotactic stimulation of posterior hypothalamic gray matter in a patient with intractable cluster headache. N. Engl. J. Med. 345, 1428–1429 (2001).
Franzini, A., Ferroli, P., Leone, M. & Broggi, G. Stimulation of the posterior hypothalamus for treatment of chronic intractable cluster headaches: first reported series. Neurosurgery 52, 1095–1099 (2003).
Leone, M. & Proietti Cecchini, A. Deep brain stimulation in headache. Cephalalgia 36, 1143–1148 (2015).
Schoenen, J. et al. Hypothalamic stimulation in chronic cluster headache: a pilot study of efficacy and mode of action. Brain 128, 940–947 (2005).
Burns, B., Watkins, L. & Goadsby, P. J. Treatment of medically intractable cluster headache by occipital nerve stimulation: long-term follow-up of eight patients. Lancet 369, 1099–1106 (2007).
Fontaine, D. et al. Treatment of refractory chronic cluster headache by chronic occipital nerve stimulation. Cephalalgia 31, 1101–1105 (2011).
Magis, D., Gerard, P. & Schoenen, J. Invasive occipital nerve stimulation for refractory chronic cluster headache: what evolution at long-term? Strengths and weaknesses of the method. J. Headache Pain 17, 8 (2016).
Fontaine, D. et al. Occipital nerve stimulation improves the quality of life in medically-intractable chronic cluster headache: results of an observational prospective study. Cephalalgia 37, 1173–1179 (2017).
Leone, M., Proietti Cecchini, A., Messina, G. & Franzini, A. Long-term occipital nerve stimulation for drug-resistant chronic cluster headache. Cephalalgia 37, 756–763 (2017).
Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33, 629–808 (2013).
Vollesen, A. L. H. & Ashina, M. PACAP38: emerging drug target in migraine and cluster headache. Headache 57 (Suppl. 2), 56–63 (2017).
Wei, D. Y. & Goadsby, P. J. Comprehensive clinical phenotyping of nitroglycerin infusion induced cluster headache attacks. Cephalalgia https://doi.org/10.1177/0333102421989617 (2021).
Naegel, S. et al. Cortical plasticity in episodic and chronic cluster headache. Neuroimage. Clin. 6, 415–423 (2014).
Messina, R. et al. Migraine and cluster headache classification using a supervised machine learning approach: a multimodal MRI study [abstract]. Neurology 92 (Suppl. 15), P4.10-016 (2019).
Negro, A., Sciattella, P., Spuntarelli, V., Martelletti, P. & Mennini, F. S. Direct and indirect costs of cluster headache: a prospective analysis in a tertiary level headache centre. J. Headache Pain 21, 44 (2020).
Mathew, N. T., Kailasam, J. & Meadors, L. Prophylaxis of migraine, transformed migraine, and cluster headache with topiramate. Headache 42, 796–803 (2002).
Acknowledgements
The authors are part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley National Health Service (NHS) Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
Both authors contributed to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
P.J.G. reports, over the last 36 months, grants and personal fees from Amgen and Eli-Lilly and Company, grant from Celgene, and personal fees from Alder Biopharmaceuticals, Aeon Biopharma, Allergan, Biohaven Pharmaceuticals Inc., Clexio, Electrocore LLC, eNeura, Epalex, GlaxoSmithKline, Impel Neuropharma, Lundbeck, MundiPharma, Novartis, Pfizer, Praxis, Sanofi, Santara Therapeutics, Satsuma, Teva Pharmaceuticals, Trigemina Inc., WL Gore, and personal fees for advice through Gerson Lehrman Group, LEK and Guidepoint, fees for educational materials from Massachusetts Medical Society, Medery, Medlink, PrimeEd, UptoDate, WebMD, and publishing royalties from Oxford University Press, and Wolters Kluwer, and for medicolegal advice in headache, and a patent magnetic stimulation for headache assigned to eNeura without fee (WO2016090333 A1). D.Y.W. declares no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks C. Gaul, P. Martelletti and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wei, D.Y., Goadsby, P.J. Cluster headache pathophysiology — insights from current and emerging treatments. Nat Rev Neurol 17, 308–324 (2021). https://doi.org/10.1038/s41582-021-00477-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-021-00477-w
This article is cited by
-
Involvement of the ipsilateral-to-the-pain anterior–superior hypothalamic subunit in chronic cluster headache
The Journal of Headache and Pain (2024)
-
A retrospective cohort study: is COVID-19 BNT162b2 mRNA vaccination a trigger factor for cluster headache?
Acta Neurologica Belgica (2024)
-
Current treatment options for cluster headache: limitations and the unmet need for better and specific treatments—a consensus article
The Journal of Headache and Pain (2023)
-
Cluster headache and kynurenines
The Journal of Headache and Pain (2023)
-
Cytokines in primary headache disorders: a systematic review and meta-analysis
The Journal of Headache and Pain (2023)