Abstract
While birth weight and weight gain have been associated with hypertension (HT), the association of linear growth, independently of weight gains, has been less well studied. We assessed the independent association of body mass index (BMI) and length at birth and changes in BMI and height during the first two decades of life with adult blood pressure (BP). A birth cohort (n = 1141) was assembled in 1978–79, and followed up at school-age and adulthood. We used conditional length and BMI measures. BMI at birth was inversely associated with HT; c-BMI from school age to adulthood and c-height from birth to school age were positively associated with hypertension. Early adiposity accretion from birth to 9 years and late linear growth from 9 to 24 years were not associated with increased HT. Regarding BP, systolic and diastolic BP presented similar partterns: the lower the BMI at birth the higher the adult BP; the higher the BMI gains in the first 2 decades of life the higher the adult BP; linear accretion only in the first decade of life was associated with adult BP. Linear growth in the first decade of life and fat accretion in the second decade are associated with adults HT.
Similar content being viewed by others
Introduction
High blood pressure is widely prevalent in low and middle-income countries1. Many studies have shown an inverse association of birth weight with adult blood pressure2, 3. The Consortium of Health-Orientated Research in Transitioning Societies group found a small inverse association of birth weight, and a stronger positive association of postnatal weight gain, with systolic blood pressure, with no association of either birth weight or later weight gain with diastolic blood pressure4.
Birth weight is a limited indicator of fetal development5, and associations between length/height and body mass index with blood pressure have been less comprehensively examined. While height is correlated with blood pressure in cross-sectional models6, height gain has not been extensively studied; in one study height gain was positively associated with systolic but not with diastolic blood pressure at 10 years of age7, but studies have not extended into adulthood. Birth weight has most consistently been associated with systolic blood pressure in adulthood but associations with diastolic blood pressure are still inconclusive2, 3. Few studies have been conducted in low and middle-income settings where the burden of hypertension is emerging rapidly, and even fewer have taken a life-course perspective4, 8.
The relationship between linear growth and later blood pressure has been studied less frequently than the relationship between weight change in childhood and later blood pressure, and has not been studied previously using growth from birth to adulthood. Thus, the objective of the present study was to assess the independent associations of body mass index (BMI) and length at birth and changes in BMI and height from birth through childhood and from childhood through adulthood with adult HT and systolic and diastolic blood pressure, in a middle-income country setting.
Methods
Our data come from a prospective cohort study performed in the city of Ribeirão Preto, Brazil. The cohort was established in 1978/79, when 94.5% of all singleton live births to women resident in the city were recruited (n = 6827). In 1987–89, a school-age follow-up was conducted at child age 9–11 years. 2861 members of the cohort were identified, invited to participate, agreed and interviewed9, 10. In 2002/04, when individuals were aged 23–35 years, 5665 of the 6484 participants who were not known to have died were traced. A systematic 1 in 3 sample was performed (the first of every three names was selected from a list sorted by birth date in each geographic region and if unavailable, the next name down was selected) and 2063 cohort members were invited and reinterviewed (Fig. 1)9, 11. The sampling strategy at each follow up stage has been fully described elsewhere10.
Data from both the school and adult waves were available for 1141 individuals. This sample size has approximately 80% power to detect a risk ratio of 2.0, assuming the event has a 10% prevalence in the control group, with a 5% probability of type I error.
Maternal characteristics were collected by interview with the mother soon after birth. We extracted the following variables: ethnicity, occupation of the family head, based on the International Classification of Occupation12; maternal age at delivery in years (≤19, 20–34, ≥35); maternal schooling in years (≤4, 5–8, ≥9); number of cigarettes smoked per day during pregnancy (0, 1–10, >10); maternal hypertension during pregnancy; type of delivery (vaginal, cesarean section); gestational age in completed weeks based on the date of the last menstrual period. When unknown or implausible, missing gestational age was imputed in a regression model13, using birth weight, parity, family income and newborn gender. The newborn was considered preterm if the gestational age was <37 complete weeks. Maternal ethnicity was categorized as black and non-black based on self-reported skin colour.
Trained personnel measured newborn weight and length immediately after delivery. The babies were weighed naked in weekly-calibrated scales with 10 g precision. Two staff measured length with the baby laid in supine position on a neonatometer14.
At the school age examination, height and weight were measured according to standard techniques15.
As adults, the participants responded to a general questionnaire. Current occupation of the family head was classified in four categories: non-manual, skilled manual, semi-skilled manual, and unskilled manual. We administered the short version of the International Physical Activity Questionnaire (IPAQ)16 and individuals were classified as sedentary, insufficiently active and active. A food frequency questionnaire (FFQ) validated for the Brazilian population17 and applied by a nutritionist, ascertained information about intake over the last 12 months of 75 food items. The nutritional value of the diets was analyzed with the software Dietsys 4.0 (National Cancer Institute, Bethesda, MD, USA), and Brazilian foods and food preparations complementary to the Dietsys program were added when complete data about them were available from Brazilian tables18. Participants’ daily alcohol consumption was considered as none, low (≤31 g) and high (>31 g). The sodium intake considered only the existing amount of sodium in the consumed foods and was categorized as: <2000, 2000–2500, and >2500 mg/d. The number of cigarettes smoked per day was categorized as 0, 1–10, or >10.
Blood pressure was measured in triplicate19 using a 740 Omron digital sphygmomanometer (OMRON Healthcare Europe B.V., Hoofdorp, The Netherlands) with a single-size cuff that was adjusted to the arm circumference. One person made all measurements at 15-min intervals, with the participant resting in sitting position with the left arm at the height of the heart. The mean of the last two measurements was use in analysis. Individuals with a systolic blood pressure above 140 and/or a diastolic blood pressure above 90 were considered as hypertensive as were those individuals who were taking medications for hypertension.
Weight was measured with an adult electronic scale (Filizola®, Sao Paulo, Brazil) with 100 g precision. Height was measured to the nearest centimeter using a stadiometer, according to standard techniques15.
Ethical approval was given by all maternities and by the Research Ethics Committee of the University Hospital, Faculty of Medicine of Ribeirão Preto, University of São Paulo (protocol no. 7606/99). All participants provided their written informed consent to participate in this study. These consents were approved by the ethics committee and one copy was given to the participant and one copy was kept with the research team.
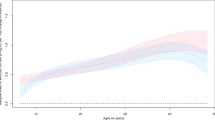
Mean and standard deviation were used to describe the Body Mass Index (BMI) and height according to sex and age. Systolic and diastolic blood pressure were described according to sex. Groups were compared using the t test. All variables were tested for normality.
BMI and height were standardized for age and sex using ANTHRO® and ANTHROPLUS®, which use the World Health Organization reference data. Since ANTHROPLUS® only goes to age 19 years, we considered the value at this age as the final adult height.
In order to eliminate the problem of collinearity among the three repeated measures of BMI or height, we computed conditional growth measures4, 20. These are calculated as the residuals from linear regressions of BMI and height at a given age and gender on all earlier measures of BMI and height. A positive residual indicates that a child grew more rapidly during the interval than would have been predicted based on its initial values and prior growth.
Frequencies were used to describe data according to the presence of hypertension or not in adulthood. Groups were compared through chi-square tests. We used Poisson regression to estimate incidence rate ratio (IRR) for HT and linear regression for systolic and diastolic BP21. To deal with missing data we chose to perform inverse probability weighting, weighting for all variables that were linked to loss of follow up from birth to adulthood22.
To avoid overadjustment covariates were selected with the aid of a directed acyclic graph (DAG)23 (Supporting Information Figure S1), following current practice in life course epidemiology, which highlights the risks of overadjustment by factors that might be intermediate in the pathways under consideration, and are therefore not confounders. Each variable was ordered according to its specific temporal relationship: pre-conception (maternal skin colour; occupation of the head of the family, maternal age and schooling); antenatal (child’s gender and maternal smoking during pregnancy); perinatal (maternal hypertension at delivery, type of delivery; BMI, length and gestational age); school age (type of school; BMI and height); adulthood (adult age, occupation of the head of the family; physical activity, smoking, alcohol consumption, sodium intake; blood pressure, BMI and height). Identifying temporal order facilitates understanding relationship between variables. We then built pathways based on temporality and theoretical assumptions. The resulting model was built upon these associations in a browser-based environment (http://www.dagitty.net). Adult risk factors for HT (physical activity, alcohol and sodium intake) did not fulfill the criteria do be considered confounders, because they are not antecedents of the exposures. This approach to deal with confounding covariates is increasingly being used24,25,26.
Since the final number of covariables was large, we double checked the results by bootstrapping the adjusted models to ensure results were robust (Supporting Information Tables S1 and S2).
Since gender differences in effects of adiposity on blood pressure have been reported27, interaction terms were tested between gender and all six growth parameters in the Poisson regression models. Finally, to check for a U-shape association between anthropometric variables and HT/blood pressure we included quadratic terms for each of the six growth parameters in the regression models (Supporting Information Table S3). Those that were significant were included in the tables. The STATA 10.1® statistical package was used for all analyses and significance level was set at 0.05.
Results
The studied sample differs in some aspects from the original birth cohort. Participants with low birth weight or low length at birth, born vaginally, from mothers with low schooling, smokers or low maternal age or whose heads of family were engaged in manual occupations were less likely to be followed-up (Table 1). Men had higher length at birth, higher blood pressure, higher BMI and height in adulthood and were more frequently hypertensive than women (Table 2). Preterm babies (6.1%) had a mean gestational age of 35.2 (sd 1.2). Eighteen mothers (1.6%) presented HT at delivery. Type of delivery (c-section), gender (males), smoking, greater alcohol and sodium intakes were associated with HT (Table 3).
Table 4 shows that neither birth length nor BMI at birth were associated with HT; at school age height and conditional height were positively associated with HT, with no association observed for BMI; adult BMI and height were associated with HT whether expressed in absolute or conditional units.
The associations of growth (BMI and height) in specific life stages with HT are shown in Table 5. The quadratic conditional-height from school-age to adulthood was significant only when it was not adjusted for the other anthropometric variables (model 1). In the final adjusted model 2, BMI at birth was inversely associated with HT (IRR = 0.79 [0.66–0.95]) and conditional BMI from school age to adulthood was positively associated with HT (IRR = 1.83 [1.55–2.16]). Conditional height from birth to school age was positively associated with HT (IRR = 1.40 [1.16–1.69]). Early adiposity accretion from birth to 9 years and late linear growth from 9 to 24 years were not associated with increased HT. The results are presented separately for men and women in the Supporting Information Table S4 (there was no statistically significant heterogeneity by sex).
Table 6 presents the results for systolic and diastolic BP. All variables except length at birth and conditional height between 9 and 24 years were positively associated with systolic and diastolic blood pressure (BMI at birth was inversely associated).
Discussion
We found that lower BMI at birth was associated with higher adult HT. Higher than expected height gain in the first decade of life was associated with adult HT but higher than expected gain in the second decade of life was not. On the other hand, higher than expected BMI gain in the second decade of life was associated with HT but higher than expected BMI gain during the first decade of life was not. Regarding BP, systolic and diastolic BP presented similar partterns: BMI at birth was associated inversely and BMI gains in the first 2 decades of life positively; linear accretion only in the first decade of life was associated with BP.
Our findings suggest that linear growth in early childhood, and increases in adiposity later in children, are important for risk of HT. The relationship between linear growth and later blood pressure has been studied less frequently than has the relationship between weight change in childhood and later blood pressure.
Faster growth has been related to a range of positive and adverse outcomes. Huang et al.28 showed the importance of postnatal weight gain on blood pressure in mid childhood. Adair et al.4 demonstrated the importance of separating the effect of weight growth and linear growth on adult outcomes: on one hand, rapid height gain in the first years of life was associated with increased schooling and final height. Conversely, greater than expected weight gain in later childhood was linked to obesity, increases in systolic blood pressure and glucose impairment. However, Adair et al. do not have an age period that dichotomizes at the immediate pre-pubertal period.
In the context of blood pressure, taller adults have higher BP, but reduced risk for CVD29. Should we favor a rapid growth of a small for gestational age babies? Which growth parameter is best?
Our study helps to clarify some of these issues. Inverse associations of BMI at birth with hypertension are evident in young adulthood. This is in line with amounting evidence2, 3. As was also seen in the ALSPAC study30 length at birth was not related to adult blood pressure. However, we found stronger associations with hypertension for height gain in the first decade of life and weight gain in the second decade of life than in this study. These associations are stronger and positive compared with the inverse association of BMI at birth with hypertension. This could suggest that postnatal growth is more strongly associated with hypertension than is prenatal growth7.
It has been pointed out that increases in relative body size are more predictive of adult blood pressure after age 11 years than in earlier childhood31. Moreover, there is evidence that growth in early life (first 48 months) has less influence in BP than growth from 48 months to adulthood32. Our results are also consistent with these strengthening associations of weight gain from birth to young adulthood with adult hypertension30, 31. As others had already seen33, higher than expected BMI gain seems to be deleterious to adult blood pressure and this association seems to amplify across infancy and adolescence until early adulthood. We found that higher than expected BMI gain in the second decade of life was associated with higher blood pressure whereas BMI gain in the first decade of life was not. In addition, with simultaneous adjustment for weight and length/height gain the associations of weight gain on systolic and diastolic blood pressure were of similar magnitude. In ALSPAC, however, associations of BMI gain on DBP were weaker than those with SBP7.
Since height is related to BP, why then is height change in the period from childhood to adulthood not associated with adult BP? As has been demonstrated elsewhere34 differences in adult height are already evident at the earlier time points. Our results are consistent with decreasing or even disappearing associations of height gain on adult hypertension because height gain was only moderately associated with SBP and not with DBP or hypertension in the second decade of life. In addition, association between height gain and SBP reduced from the first to the second decade of life. Thus, hypertension due to accelerated gains in height in early life seems not to persist through adult life. This decreasing or even vanishing association of height gain on adult hypertension seems to represent a physiological rather than a pathological effect. It might be explained by a mismatch between linear and renal/arteriolar growth and development35. It seems that in infancy and post-infancy, early linear growth spurts are not accompanied by similar developments in renal and arteriolar function, thus resulting in higher blood pressure. Our results suggest that this adaptative mechanism that results in higher blood pressure in early life due to the linear growth spurt are transient and do not track to adult life. In contrast, effects of BMI gain seem to persist and increase from birth to adulthood.
In agreement with our data, results from a pooled analysis of birth cohort studies from low and middle income countries also reported that height gains at age 2 years and mid-childhood but not in adulthood were associated with SBP4. However, Menezes reported that early length/height gains in the first four years of life are not associated with higher systolic blood pressure36.
It is important to note that in our study the association between height gain and diastolic blood pressure was only evident from birth to school age and was weaker than the corresponding association with systolic blood pressure. This is in contrast to ALSPAC data, in which diastolic BP at 10 years was not influenced by height growth7.
The present study has some strengths worth underlying: it is a population-based prospective birth cohort from a middle-income setting. The conditional modeling of height and BMI changes provides information on the relative contribution of BMI gain and linear growth in predicting adult blood pressure.
A limitation of this study is measurement error. Newborn length is not always precisely measured. We minimized the potential for error by standardizing data collection. Blood pressure assessed at one point in time may be elevated because of white coat syndrome. This would affect the whole sample, resulting in non-differential misclassification. Another limitation is that losses to follow-up may have generated a sample with better health and social conditions than the original subjects at birth. If we had had access to these less healthy and wealthy subjects our effect size would possibly be stronger. However, we performed inverse probability weighting to minimize this bias. An important limitation is that no data are available on growth from birth to 2 years34.
The independent association of growth patterns with adult hypertension, even after controlling for adult risk factors confirms that CVD prevention actions should not be restricted to adulthood. This evidence has been acknowledged by the United Nations heads of States and governments37.
In conclusion, postnatal growth seems to have more influence on hypertension than prenatal growth. Higher BP due to accelerated gains in height in early life seems to be an evidence for the first decade of life, but it does not track into the second one. Higher than expected fat accretion seems to be deleterious to adult blood pressure and its effect seems to be bigger in the second than in the first decade of life. Strategies for preventing fat accretion in the first and especially in the second decade of life are probably more important than strategies focusing on early mother and child nutrition to prevent hypertension in adulthood.
References
Balbus, J. M. et al. Early-life prevention of non-communicable diseases. Lancet. 381, 3–4 (2013).
Gamborg, M. et al. Birth weight and systolic blood pressure in adolescence and adulthood: meta-regression analysis of sex- and age-specific results from 20 Nordic studies. Am. J. Epidemiol. 166, 634–645 (2007).
Min, M. et al. Birth weight and subsequent blood pressure: a meta-analysis. Arch. Cardiovasc. Dis. 105, 99–113 (2012).
Adair, L. S. et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 382, 525–534 (2013).
WHO Technical Consultation Towards the Development of a Strategy for Promoting Optimal Fetal Development (2003: Geneva, Switzerland). Promoting optimal fetal development: report of a technical consultation. http://www.who.int/nutrition/publications/fetal_dev_report_EN.pdf?ua=1 (2014).
Regnault, N. et al. Components of height and blood pressure in childhood. Int. J. Epidemiol. 43, 149–159 (2014).
Jones, A. et al. Adipose and height growth through childhood and blood pressure status in a large prospective cohort study. Hypertension. 59, 919–925 (2012).
Ferraro, A. A. & Fernandes, M. T. B. Relationship between childhood growth and later outcomes. Nestlé Nutr. Inst. Workshop. Ser. 71, 191–197 (2013).
Barbieri, M. A. et al. Health in early adulthood: the contribution of the 1978/79 Ribeirão Preto birth cohort. Braz. J. Med. Biol. Res. 39, 1041–1055 (2006).
Cardoso, V. C. et al. Profile of three Brazilian birth cohort studies in Ribeirão Preto, SP and São Luís, MA. Braz. J. Med. Biol. Res. 40, 1165–1176 (2007).
Haeffner, L. S., Barbieri, M. A., Rona, R. J., Bettiol, H. & Silva, A. A. The relative strength of weight and length at birth in contrast to social factors as determinants of height at 18 years in Brazil. Ann. Hum. Biol. 29, 627–640 (2002).
Olsen, J. & Frische, G. Social differences in reproductive health. A study on birth weight, stillbirths and congenital malformations in Denmark. Scand. J. Soc. Med. 12, 90–97 (1993).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons (1987).
Davies, D. P. & Holding, R. E. Neonatometer: a new infant length measurer. Arch. Dis. Child. 47, 938–940 (1972).
Cameron, N. BASIC programs for the assessment of skeletal maturity and the prediction of adult height using the Tanner-Whitehouse method. Ann. Hum. Biol. 11, 261–264 (1984).
Pardini, R. et al. Validation of the International Physical Activity Questionaire (IPAQ-version 6): pilot study in Brazilian young adults. Rev. Bras. Ciên. e Mov. 9, 45–51 (2001).
Ribeiro, A. B. & Cardoso, M. A. Development of a food frequency questionnaire as a tool for programs of chronic diseases prevention. Rev. Nutr. Campinas. 15, 239–245 (2002).
Molina, M. C. et al. Food consumption by young adults living in Ribeirão Preto, SP, 2002/2004. Braz. J. Med. Biol. Res. 40, 1257–1266 (2007).
Hense, H. W. et al. Assessment of blood pressure measurement quality in the baseline surveys of the WHO MONICA project. J. Hum. Hypertens. 9, 935–946 (1995).
Keijzer-Veen, M. G. et al. A regression model with unexplained residuals was preferred in the analysis of the fetal origins of adult diseases hypothesis. J. Clin. Epidemiol. 58, 1320–1324 (2005).
Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 159, 702–706 (2004).
Härkänen, T., Kaikkonen, R., Virtala, E. & Koskinen, S. Inverse probability weighting and doubly robust methods in correcting the effects of non-response in the reimbursed medication and self-reported turnout estimates in the ATH survey. BMC Public Health. 14, 1150 (2014).
Textor, J., Hardt, J. & Knüppel, S. DAGitty: A Graphical Tool for Analyzing Causal Diagrams. Epidemiology. 5, 745 (2011).
Shah, A. D., Vittinghoff, E., Kandula, N. R., Srivastava, S. & Kanaya, A. Correlates of prediabetes and type II diabetes in US South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA)study. Ann. Epidemiol. 25, 77–83 (2015).
Bodén, R. et al. Higher mortality after myocardial infarction in patients with severe mental illness: a nationwide cohort study. J. Intern. Med. 277, 727–736 (2015).
Weisskopf, M. G., Kioumourtzoglou, M. A. & Roberts, A. L. Air Pollution and Autism Spectrum Disorders: Causal or Confounded? Curr. Environ. Health. Rep. 2, 430–439 (2015).
Huang, R. C. et al. Sex dimorphism in the relation between early adiposity and cardiometabolic risk in adolescents. J. Clin. Endocrinol. Metab. 97, E1014–E1097 (2012).
Huang, R. C. J. et al. Perinatal and childhood origins of cardiovascular disease. Int. J. Obes (Lond). 31, 236–244 (2007).
Leon, D. & Ben-Shlomo, Y. Preadult Influences on Cardiovascular Disease and Cancer. In: Kuh, D. & Ben-Schlomo, Y. eds A Life Course Approach to Chronic Disease Epidemiology. New York: Oxford University Pres, 45–77 (1997).
Hughes, A. R., Sherriff, A., Lawlor, D. A., Ness, A. R. & Reilly, J. J. Timing of excess weight gain in the Avon Longitudinal Study of Parents and Children (ALSPAC). Pediatrics. 127, e730–736 (2011).
Gamborg, M. et al. Life course path analysis of birth weight, childhood growth, and adult systolic blood pressure. Am. J. Epidemiol. 169, 1167–1178 (2009).
Adair, L. S. et al. Size at birth, weight gain in infancy and childhood, and adult blood pressure in 5 low- and middle-income-country cohorts: when does weight gain matter? Am. J. Clin. Nutr. 89, 1383–1392 (2009).
Huang, R. C., Burrows, S., Mori, T. A., Oddy, W. H. & Beilin, L. J. Lifecourse Adiposity and Blood Pressure Between Birth and 17 Years Old. Am. J. Hypertens. 28, 1056–1063 (2015).
Stein, A. D. et al. Growth patterns in early childhood and final attained stature: data from five birth cohorts from low- and middle-income countries. Am. J. Hum. Biol. 22, 353–359 (2010).
Weder, A. B. & Schork, N. J. Adaptation, allometry, and hypertension. Hypertension. 24, 145–156 (1994).
Menezes, A. M. et al. Adolescent blood pressure, body mass index and skin folds: sorting out the effects of early weight and length gains. J. Epidemiol. Commun. H. 66, 149–154 (2012).
United Nations, 2011. http://www.un.org/en/ga/ncdmeeting2011/pdf/NCD_draft_political_declaration.pdf (2013).
Acknowledgements
The authors wish to thank the interviewers and the mothers who kindly agreed to participate in the study. This work was supported by the São Paulo State Research Foundation (FAPESP) and by the Brazilian National Research Council (CNPq).
Author information
Authors and Affiliations
Contributions
Alexandre A. Ferraro - analyzed data and performed statistical analysis; wrote paper. Marco A. Barbieri - designed research; conducted research, provided essential materials. Antonio A. M. da Silva - designed research; performed statistical analysis; wrote paper. Carlos Grandi - provided essential materials; corrected draft. Viviane C. Cardoso - conducted research; provided essential materials. Aryeh D. Stein - provided essential materials; performed statistical analysis; corrected draft. Heloisa Bettiol - designed research; conducted research, provided essential materials.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferraro, A.A., Barbieri, M.A., da Silva, A.A.M. et al. Contributions of relative linear growth and adiposity accretion from birth to adulthood to adult hypertension. Sci Rep 7, 8928 (2017). https://doi.org/10.1038/s41598-017-09027-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-09027-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.