Abstract
The aim of this work was to investigate differences between depressed subjects (PG) and non-depressed healthy control participants (HCG) with regard to fatigue dimensions and inflammation. For this purpose, 43 participants in the PG and 51 participants in the HCG were included in the study. IL-6, IL-1β, TNF-α, IFN-γ, and CRP were assessed in venous blood samples. Fatigue and depression were assessed using the FIS-D and BDI-FS questionnaires. Main results showed higher BDI-FS values in PG. Moreover, PG showed mean differences for fatigue dimensions when compared to the HCG. For the pro-inflammatory markers, a moderate group effect was found between PG and HCG which was mainly caused by IL-6. Correlations between TNF-α and BDI-FS, TNF-α and cognitive fatigue, TNF-α and psychosocial fatigue were found within the PG. In the HCG, correlations were found between IL-6, TNF-α and somatic fatigue, as well as IL-6 and cognitive fatigue. Significant correlations were found between the psychological variables in both groups. All results were controlled for the confounding variables gender, age, BMI and multiple comparisons. These results suggest the presence of inflammation in both depression and fatigue. However, each correlates with different pro-inflammatory parameters, suggesting a biological heterogeneity.
Similar content being viewed by others
Introduction
Depression is a mental health disorder, which is present in 27% of the world population and it is associated with a high DALY-metric1,2. The clinical features are predominantly lowering of mood, reduction of energy, and decrease in activity3. Among other symptoms, marked tiredness after even minimum effort is common3.
Well regarded models for depression frequently involve a stress-induced change in behavior. According to these models, stress activates different hypothalamic regions, which promotes higher concentrations of pro-inflammatory cytokines4,5. Two animal studies in mice have shown that higher levels of pro-inflammatory cytokines can lead to memory deficits and depressive mood symptoms6,7. This statement was corroborated in two studies who demonstrated a relationship between IL-1β and depressive disorders8 as well as with cognitive performance9.
Another consequence of the stress caused by overactivation of the hypothalamus is fatigue5, which it has been described as a diminished ability to initiate or maintain activity or to maintain attention10,11. Fatigue is considered either a common nonspecific symptom or a syndrome and until today there is no uniform definition. To reach a possible definition, two reviews from Brurberg et al. and Watanabe et al. proposed an dimensional approach for fatigue12,13, which include three important dimensions: somatic (e.g. musculoskeletal pain/tiredness), psychosocial (e.g. restrained social activity due to fatigue or mood impairment), and cognitive complains (e.g. decreased ability to maintain attention, memory impairment)12,13.
Following this dimensional approach, many conditions were associated with different dimensions of fatigue, including: drugs, deficiency diseases (i.e. iron-deficiency anemia), depression, anxiety disorders, burnout and chronic fatigue syndrome14,15. Interestingly, other conditions that also present fatigue are related strongly to inflammation as well (e.g. tumor-related fatigue, organ failure, chronic infectious diseases, endocrine diseases and autoimmune diseases, etc.)14,15. For instance, patients with chronic diseases such as rheumatoid arthritis16 or chronic kidney disease17 develop a persistent somatic and psychosocial fatigue that impairs the ability to perform daily activities. Additionally, it was demonstrated in patients with chronic kidney disease that higher levels of pro-inflammatory cytokines (i.e., IL-6) were associated with fatigue measured with the SF-36, which included mostly elements of the psychosocial and somatic fatigue dimensions17.
The presence of inflammation on perceived fatigue18 indicates possible dysregulation of the hypothalamic axis19. Such a deregulation also occurs in depressive disorders20,21, where fatigue is a common clinical manifestation. This has been shown in two studies in which higher cytokine levels and fatigue were correlated in patients with depressive symptoms21,22 and one study with healthy patients23. To our knowledge, however, there are no human studies on primary depression that relate inflammation to the above-mentioned fatigue dimensions.
To contribute to the evidence line for depression, which shows differences and possible correlations between fatigue and pro-inflammatory mechanisms in depression19,24,25,26, the main objectives of this study are (1) to examine whether the fatigue dimensions scores differ between participants with depression and non-depressed healthy control subjects, (2) to investigate whether the concentration of certain pro-inflammatory markers differ between the two groups, (3) to test whether there is a positive correlation between inflammation and the depression severity scores, and finally (4) the investigation of positive correlations between the values of fatigue dimensions and inflammation in participants with depression compared to non-depressed healthy control subjects.
Results
General characteristics of the sample
Baseline laboratory and clinical characteristics of the 94 participants included in the study are listed in Table 1. The sample consisted of about twice as many women as men. However, the ratio of men and women did not differ per group (Table 1). The age differed between the groups by about 1 year (median) with the IQR being slightly higher in the depression group (Table 1). More smokers were found in the patient group (p = 0.06, Cramer’s V = 0.21).
Pro-inflammatory markers: Fatigue dimensions and Depression
Fatigue dimensions (COG-F, SOM-F, PSY-F) and BDI-FS scores were analyzed using a MANCOVA. The grouping factor was status (PG and HCG), covariates were the pro-inflammatory markers (Table 3). There was a significant difference between the PG and HCG groups in the combined dependent psychological variables after control of the pro-inflammatory markers (F4,74 = 30.38, Wilks’ Λ = 0.38, p < 0.001, η2p = 0.62). Of all pro-inflammatory markers used as covariates, only IL-6 predicts fatigue and depression (F4,74 = 4.68, Wilks’ Λ = 0.80, p = 0.002, η2p = 0.20) (Table 3). The univariate tests showed differences for all fatigue dimensions and BDI-FS values between the groups PG and HCG (COG-F: F1,77 = 62.59, p < 0.001; SOM-F: F1,77 = 54.83, p < 0.001; PSY-F: F1,77 = 114.17, p < 0.001; BDI-FS TOT: F1,77 = 69.09, p < 0.001). Univariate tests for the covariate IL-6 concentrations showed a significant correlation with each of the fatigue dimensions (COG-F: F1,77 = 14.97, p < 0.001; SOM-F: F1,77 = 14.29, p < 0.001; PSY-F: F1,77 = 14.49, p < 0.001), but not with BDI-FSTOT (F1,77 = 1.46, p = 0.23).
Relationship between inflammation markers and age, gender and BMI
The confounding of age, gender and BMI with the fatigue dimensions as well as the BDI-FS values and also the pro-inflammatory markers were assessed with a MANCOVA. Here, too, the status was used as a grouping factor. The results of the analysis are shown in Table 4.
There was a significant difference between the PG and HCG groups in the combined dependent variables after controlling the influence of age, gender and BMI (F9,71 = 13.02, Wilks’ Λ = 0.38, p < 0.001, η2p = 0.62). All of the confounding variables showed a correlation with the dependent variables (gender: F9,71 = 2.94, p = 0.01, η2p = 0.27; age: F9,71 = 3.09, p = 0.003, η2p = 0.28, and BMI: F9,71 = 5.08, p < 0.001, η2p = 0.39).
In a further analysis with univariate tests, the status showed significant differences between PG and HCG for IL-6 (F1,79 = 4.95, p = 0.03), for all the fatigue dimensions (COG-F: F1,79 = 59.53, p < 0.001; SOM-F: F1,79 = 49.06, p < 0.001; PSY-F: F1,79 = 110.05, p < 0.001) and for BDI-FS total scores (F1,79 = 74.65, p < 0.001). The other cytokines showed no significant status differences in univariate tests (Table 4).
Regarding the univariate tests involving the confounds, gender correlated with the acute-phase protein CRP (F1,79 = 5.40, p = 0.02) and with the cognitive fatigue (COG-F: F1,79 = 7.15, p = 0.01). Age correlated only with IL-6 concentrations (F1,79 = 7.17, p = 0.01). Finally, BMI correlated with IL-6 (F1,79 = 8.52, p = 0.01), CRP (F1,79 = 26.67, p < 0.001), somatic fatigue (SOM-F: F1,79 = 5.31, p = 0.02) and psychological fatigue (PSY-F: F1,79 = 7.26, p = 0.01).
Correlations within groups between pro-inflammatory markers, fatigue scores and BDI-FS total scores
Pairwise correlations between all psychological variables and the five assessed pro-inflammatory markers’ concentrations were calculated separately for each group.
Based on the effects of age, gender and BMI on the proinflammatory markers, fatigue dimensions and overall BDI-FS values, this proportion of the variance was removed before the correlation analysis. The p-values of the correlation analysis were Bonferroni adjusted by setting the p-value threshold correction for 5 (i.e. the number of pro-inflammatory markers in this study) multiple comparisons (p(α=0.05) = 0.01).
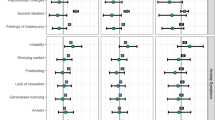
Different correlation patterns were found between the two groups. In the PG, TNF-α concentrations correlated with the COG-F scores (Spearman’s ρ = 0.36, p = 0.0095, CI95 [0.11, 1]) and with the PSY-F scores (Spearman’s ρ = 0.40, p = 0.004, CI95 [0.16, 1]). In the HCG, the cytokine IL-6 correlated with the COG-F scores (Spearman’s ρ = 0.34, p = 0.007, CI95 [0.12, 1]) and SOM-F scores (Spearman’s ρ = 0.37, p = 0.004, CI95 [0.15, 1]), and TNF-α correlated with the SOM-F scores (Spearman’s ρ = 0.34, p = 0.007, CI95 [0.12, 1]).
Correlations between the cytokine concentrations and the BDI-FS total scores
The BDI-FS scores correlated with TNF-α within the PG group (Spearman’s ρ = 0.47, p = 0.0008, CI95 [0.24, 1]), but not within HCG (Spearman’s ρ = −0.08, p = 0.70, CI95 [−0.30, 1]). All other pairwise correlations between cytokine correlations and BDI-FS have not exceeded the critical p-threshold.
Differences between depression and fatigue in the correlation analysis
We consider the question of whether fatigue can be distinguished from depression by examining the correlation patterns with the pro-inflammatory markers. A two-block stepwise regression model was performed. The first block considered the total BDI-FS values, the second block the fatigue values. This regression model was only calculated for the PG group, as this group presented a pro-inflammatory marker (i.e. TNF-α) that correlated with both depression and two fatigue dimensions (COG-F and PSY-F). The first model, which consisted only of block 1 (TNF-α x BDI-FS total scores), explained 10.9% of the TNF-α variance (R2 = 0.109, p = 0.037). When the second block with the COG-F values was added, no significant changes compared to the previous model were observed (R2 = 0.136, ΔR2 = 0.027, p = 0.267). Comparable results were obtained with PSY-F instead of COF-F (PSY-F: R2 = 0.133, ΔR2 = 0.024, p = 0.297).
Discussion
Differences between groups of depressed and non-depressed participants
The recruitment strategy was successful in terms of significantly higher BDI-FS values in the group of depressed study participants. All fatigue values, psychological, cognitive and somatic fatigue were also higher in depressed people. These results are consistent with the assumption that fatigue is a predominant symptom of depressive disorders27. A study evaluating excessive daytime sleepiness and fatigue in depressed patients showed significant differences in fatigue dimensions between patients and healthy controls28.
The results of fatigue dimensions and depression scores compared to the proinflammatory markers, which are shown in Table 3, show that the IL-6 concentrations differed between the fatigue dimensions, but not in the total depression scores. The finding that the IL-6 concentrations are different for all fatigue dimensions is consistent with the literature on the inflammatory components upon fatigue17,19,29,30.
Table 4 shows that the IL-6 concentrations differed between depressed and non-depressed participants. This result is consistent with two meta-analyses from human studies that reported significant differences of peripheral IL-6 levels in patients with depressive disorders compared to healthy controls31,32. However, the results obtained in Table 3 showed that all fatigue values, but not the total depression values, explained the IL-6 concentration differences. Therefore, fatigue could contribute to explain the pro-inflammatory components in depression. One plausible explanation for this could be that stress triggers HPA activation, which produces larger amounts of ACTH, which in turn stimulates increased cortisol production in the adrenal cortex and therefore promotes the release of IL-6 in the blood4,33,34. The released peripheral IL-6 could act directly on the adrenal cortex cells. Stimulation with IL-6 leads to an increased production of glucocorticoids in the blood and an increase in ACTH receptors in the adrenal cortex35,36,37. As a result of these IL-6-promoted effects in the CNS, the concentrations of glucocorticoids in depression could be increased38,39,40,41,42,43 and contributing finally to the development of several clinical manifestations of mood disorders, such as fatigue43.
Regarding the model processed in Table 4, confounding factors’ analysis showed interestingly an influence of BMI on somatic and psychosocial fatigue. This is consistent with studies showing that people with a higher BMI (e.g. obese adults) report a higher level of mental fatigue as well as insufficient physical activity and sleepiness due to fatigue44. Gender only had an impact on cognitive fatigue. This can possibly be seen in the context of the results of a German study on general population in which women showed higher scores for mental fatigue45.
The model presented in Table 4 also showed that the selected covariates (gender, age and BMI) had also remarkable influence. In terms of gender, CRP acute phase protein was different between men and women. Other studies have also found that CRP is slightly higher with age and gender46. As expected from the literature47, IL-6 increased with age and BMI. The latter also showed a correlation with CRP. This is also in line with the literature, which indicates mild inflammation due to a large amount of metabolic stress such as obesity48,49,50.
Correlations within groups of depressed or non-depressed participants
Within each group, correlations between depression and all fatigue dimensions were on a similar and significant level. Only the correlation between depression and psychosocial fatigue in the patient group was definitely higher. These results support the commonly reported relationship between depression and fatigue on the subjective level. However, it should be borne in mind that the correlations are not strong enough to provide reliable evidence that depression and fatigue are the same (see, for example, the step-by-step regression with two blocks in Chapter 3.4). This is also supported by the correlation pattern of the pro-inflammatory markers with the psychological variables. Positive correlations of the pro-inflammatory cytokine TNF-α with psychosocial and cognitive fatigue as well as with the severity of the depression were found in depressed, but not in non-depressed participants. Interestingly, TNF-α was positively associated with somatic fatigue and IL-6 with somatic and cognitive fatigue in the non-depressed healthy controls group. A positive relationship between TNF-α and depressive symptoms51 has been reported earlier in the literature. In a study with systemic lupus erythematosus, a pro-inflammatory autoimmune disease, a higher TNF-α value was also associated with stronger depressive symptoms. This relationship is also supported by results that show increased gene expression in the TNF family in depressed subjects and negative correlations with cognitive efficiency52. When the results are viewed from the perspective of the effect of TNF-α on the CNS, TNF-α (like IL-6) is an inflammatory cytokine that is produced by macrophages36,37, that can actively cross the blood-brain barrier53, having a direct influence on the HPA16. This increases cortisol production and thus contributes to depression psychopathology43. In addition, TNF-α has a dose-dependent relationship to basal cortisol production. The more TNF-α is produced, the more cortisol is produced54,55. This dose-dependent relationship may also affect the relationship between TNF-α and the severity of the depression and, in this study, the BDI values.
Some studies have reported the relationship between cytokine concentrations and fatigue19. TNF-α is generally increased in chronic fatigue syndrome or fatigue56, in chronic kidney disease IL-6 is positively correlated with fatigue17.
TNF-α and IL-6 are both inflammatory cytokines that are produced by macrophages and increase cortisol levels in humans57. Glucocorticoids are not only involved in the development of muscle weakness, cognitive dysfunction, sleep disorders and a strong feeling of illness, but also in a changed mood. These clinical symptoms are more or less synonymous with fatigue and its dimensions, namely the somatic (e.g. muscle weakness), the cognitive (e.g. reduced attention and memory) and the psychosocial (e.g. high level of illness, sleepiness, fatigue) dimension.
The results of this study show different correlation patterns in the groups of depressed and non-depressed participants. The psychosocial fatigue component correlated with inflammation in the group of depressed participants, probably because this component is more common in depression58,59,60,61. On the other hand, the somatic fatigue component correlated with the inflammation in the group of non-depressed participants who by definition had no mood disorders62.
However, the dimensions of cognitive fatigue and inflammation correlated in both groups. This could mean that the correlation between pro-inflammatory cytokines (TNF-α in depressed participants, IL-6 in non-depressed participants) and cognitive fatigue symptoms may not be affected by depression. In many diseases without a primary mental component, cognitive fatigue symptoms also correlate with pro-inflammatory cytokines16,29,63,64.
Finally, the fatigue dimensions correlated in the HCG with various cytokines - TNF-α with cognitive fatigue as well as TNF-α and IL-6 with cognitive and somatic fatigue (see Table 5). Although they are different cytokines, both are produced by the macrophage and induce similar effects in the human body57.
Limitations
As always, the sample size could be larger to generalize the results beyond the context of the study. However, the power obtained from this study with 94 participants was 1-β = 0.91, value that overcome the 1-β = 0.80 threshold. The sample size for the study design used should therefore be sufficient to examine the expected effects.
The higher number of women compared to men in both groups examined could have influenced the results. In Germany, the ratio of women to men treated for depression is approximately 2: 165,66. This relationship is also reflected in this study.
As expected, there were many very low BDI depression scores in the group of non-depressed participants, which led to a positively skewed distribution. Somehow surprisingly, no floor effects were seen for the fatigue values. However, IL-1β was positively skewed in both groups, TNF-α only in the group of depressed participants. This skewness was mainly due to the occurrence of some higher values. Rank correlation analyzes were therefore calculated where possible. However, MANCOVA’s results could be slightly affected.
CRP data being labeled as maximum values by the ‘absorbance plate reader’ in nine participants hat to be excluded from analysis (nPG = 4, nHGC = 5). CRP is an acute phase protein with anti-inflammatory effects, but is mainly non-specific, levels could be elevated and not necessarily be correlated with inflammatory processes49.
Smoking can affect cytokine levels. Therefore, smoking behavior was treated as a confounding factor, but it did not appear to affect the results of the current study.
Future directions
There are several points of interest for future studies. Proinflammatory markers were sampled from the plasma but not obtained from CSF. It would be of advantage validate the results with central cytokine concentrations. Future studies could include cortisol and ACTH, both influenced by cytokines in the regulation of HPA activity, in the study of inflammation, depression, and fatigue. As always, longitudinal studies of cytokine levels in depression and fatigue-related illnesses are worthwhile to primarily determine whether cytokine levels are more likely in emergencies or in acute situations. In this research area, it is certainly an important goal to investigate whether the (first) onset of depression is also related to changes in the cytokine concentration and whether there is a connection between deregulation of HPA, inflammation and depressive symptoms. The extension of the methods to in vivo magnetic resonance spectroscopy would be of interest to establish a connection between the hypothalamic activity and the cytokine concentrations in the peripheral plasma or in the CSF.
Conclusions
At the subjective self-assessment level, the study showed a clear difference in all dimensions of fatigue in depressed compared to non-depressed participants. The fatigue dimensions, but not the severity of the depression, showed differences in IL-6 concentrations. The pro-inflammatory cytokine IL-6 was also increased in participants with depression. Correlations within groups showed that the severity of depression determined by the BDI-FS was positively associated with TNF-α in depressed, but not in non-depressed participants. In addition, TNF-α correlated with psychological and cognitive fatigue within the group of depressed participants, but not in the control group. The correlation pattern was different in the group of non-depressed participants. IL-6 correlated with cognitive and somatic fatigue, TNF-α correlated only with somatic fatigue. In summary, correlations of fatigue and inflammation were found in both groups, but not equally for every dimension of fatigue in each of the groups. This could mean that the correlation between inflammatory cytokines and fatigue symptoms is not necessarily influenced by depression and therefore fatigue and depression are overlapping constructs, but are not identical. Future studies could include cortisol and ACTH, both of which are affected by cytokines in regulating HPA activity to address this issue.
Methods
Study design
A case-control study was conducted. 43 patients diagnosed with depression or depressive episode (DE) as defined by ICD-10 (PG) and 51 healthy controls (HCG; community sample), aged between 18 and 65 years, were included in the study. Groups were matched by age and gender. Data collection was performed between November 2018 and September 2019. In the PG, volunteers with DE but without concomitant psychotic episode were included. Patients having another comorbid psychiatric disease (i.e. bipolar disorder, personality disorder, adaptation syndrome and post-traumatic stress disorder) were included as long as a DE was present and predominant during the last 6 months. Exclusion criterion for both PG and HCG were insufficient German language knowledge, somatic or cognitive limitations that did not allow participation, particularly visual or auditory limitations. Individuals could not participate if they suffered from acute or chronic disease or illness of any type, particularly related to infection, except depression. Latter were assigned to the patient’s group. Demographic data are shown in Table 1.
Participants or legal authorized representatives were informed about the procedure and gave written informed consent of participation. All experimental procedures were in accordance with the Declaration of Helsinki and were approved by the local ethics committee of the Justus-Liebig University (JLU) medical faculty. The study complies with the APA ethical standards.
Data collection
Blood Sampling
3 mL fasting venous blood samples were collected between 8:00 am and 12:00 pm with EDTA K blood sample tubes (S-Monovette 2.7 mL K3E tube with 1.6 mg EDTA/mL, SARSTEDT AG & Co. KG, Nümbrecht, Germany) and then centrifuged at 4 °C with 1100 × g for 15 minutes. After centrifugation, the plasma was collected, divided into two 0.5 mL aliquots and immediately stored at −20 °C. Every 4 weeks, the blood samples were collectively delivered to an university research facility, which was about 30 km away, and stored at −80 °C for further use.
Levels of IL-6, IL-1β, C-reactive Protein (CRP), Tumor necrosis factor-alpha (TNF-α) and Interferon-gamma (IFN-γ) were measured using ELISA (Quantikine ELISA kits, R&D Systems Inc., Minneapolis, Minnesota, United States of America) with the detection limits of: IL-6 = 3.13 pg/mL, IL-1β = 3.9 pg/mL, CRP = 0.78 ng/mL, TNF-α = 15.6 pg/mL and IFN-γ = 15.6 pg/mL. Intra- and inter-precision values were <10%.
IL-1β values below the ELISA detection limit (one participant) were considered to be zero pg/mL and included in the analysis. Maximum plasma values (indicated by the software as ‘>Max’) for IL-6 (one participant), CRP (nine participants) and IL-1β (one participants) were reported and excluded from the analysis.
Pro-inflammatory markers’ concentrations were calculated using the Tecan Reader and Magellan Reader Software (Tecan Group Ltd., Männedorf, Switzerland). For the parameter calculation, the Marquardt’s 4-parameter estimation method was used.
Depression
DE as defined according to the diagnostic criteria from the International Statistical Classification of Diseases and Related Health Problems, 10th version (ICD-10)3. The presence of a DE was diagnosed in the psychiatric department of the University Hospital of Giessen and Marburg (Location - Giessen), by clinical experts.
The Beck Depression Inventory – Fast Screening, German Version (BDI-FS)67 was applied for scoring the severity of the DE. The BDI-FS provides scores in the range between 0–21. The highest score indicates a high load of depressive burden. The instrument has good internal consistence (Cronbach’s α = 0.84) and a convergent validity with the PHQ-9 of r = 0.67, including that it was validated to a representative German sample (n = 2467). If necessary, the cut-off definitions recommended in the manual were used (cut-off = 5). The categories used were labeled as minimal (0 to 3 points), mild (4 to 8 points), moderate (9 to 12 points), and severe (13 to 21 points).
Fatigue dimensions
The extent of fatigue was assessed on the subjective level. The subjective ratings of fatigue were recorded applying the Fatigue Impact Scale – German Version (FIS-D68) in both groups. The FIS-D measures the impact of fatigue on Health-Related Quality of Life68. The FIS-D consists of three sub-scales, which represent a three-dimensional structure of fatigue. These dimensions include a psychosocial dimension (or PSY-F, 20 questions, maximum score 80 points), a somatic dimension (or SOM-F, 10 questions, maximum score 40 points) and a cognitive dimension (or COG-F, 10 questions, maximum score 40 points). The maximum score that can be acquired is 160 points (4 for each item). As defined in the FIS-D manual, the cut-off values for increased fatigue are over 20 points for the psychosocial dimension, over 10 points for the somatic or cognitive dimension, and over 40 points for the full test.
Statistical Analysis
Statistical analyses were performed using SPSS version 24.0 (Statistical Package for the Social Sciences, International Business Machines Corporation, New York, United States of America) and JASP version 0.11.1 (Jeffreys’s Amazing Statistic Program, The University of Amsterdam, Amsterdam, The Netherlands).
Quantitative variables approximately fitting a normal distribution are specified in the text as mean ± standard deviation (M ± SD), those with a non-normal distribution were expressed as median (Me) with percentile 75 (Q3) and percentile 25 (Q1) and the interquartile range (Q3–Q1; IQR). Categorical variables were specified with numbers and in some cases quotient values. For obtaining results with two decimals, data was rounded to the next decimal. Values smaller than 0.001 were denotated as <0.001 and values greater than one million were expressed in scientific notation.
To improve readability, the data was organized in tables. General sample information is listed in Table 1 and information regarding psychological and immunological parameters is displayed in Table 2.
Table 1 also shows the group difference statistics. The Student t-test was used for continuous, parametrically distributed data. Otherwise, the U-Mann-Whitney test was used. For group differences in categorical data, χ2 or the exact Fisher test was calculated. Then homogeneity between groups (i.e. PG = HCG) was assumed if the bilateral p-value was greater than a threshold value of 0.05.
Regarding the information for the effect sizes on the Table 1, Cohen’s d (for parametrical distributed data), Eta-Square (for non-parametrical distributed data), and Cramer’s V (for categorical data). Cohen’s d thresholds were defined as low = 0.2, medium = 0.5, high = 0.8. For the Cramer’s V effect size, we used the following thresholds: very low 0 to 0.1, low 0.1 to 0.3, medium 0.3 to 0.5 and high up to 0.5. For the non-parametrical data, Eta-Square (ES) was used under the following formula: η2 = Z2/N-1. The effects were defined as weak whenever ES ≤ 0.04; ES was defined as medium when 0.04 < ES ≤ 0.36 and as strong when ES > 0.36.
For the mean comparisons between the groups, two multivariate analyses of covariance (MANCOVA) were computed, one for the psychological variables (PSY-F, COG-F, SOM-F) and the other for the pro-inflammatory cytokines IL-6, IL-1β, TNF-α, IFN-γ, and CRP. Gender, age, and BMI were included in both models as covariates. These results are shown in Tables 3 and 4. The mean differences between groups were flagged ‘significant’ if the two-tailed-p-value was smaller as 0.05. Partial eta-square values were calculated for the effect sizes. For the multivariate tests, the partial ES was calculated using the following formula: η2p = (df1 * F)/[(df1 * F) + df2]69,70. For the univariate test, the partial ES was calculated using the following formula: η2p = (SSeffect)/[SSeffect + SSerror]69,70. The effects for both partial ES formulae were defined as following: very small (η2p < 0.01), small (0.01 ≤ η2p < 0.06), moderate (0.06 ≤ η2p < 0.14) and large (η2p ≥ 0.14)69,70.
For the correlation matrices within each group, Spearman rank correlations (Spearman’s ρ) between all variables including the total BDI-FS score were calculated. All variables were previously adjusted for the influence of the confounding factors gender, age, smoking-behavior, medication intake, and BMI. For this purpose, a linear model was calculated for each variable with the confounding factors as predictors for both groups separately. The residuals were used as new variables. According to the hypothesis that the higher the pro-inflammatory cytokine concentrations, the higher the fatigue dimension or the depression values, only positive correlations were considered and therefore one-sided tests were calculated. In order to take multiple testing into account, corresponding p-values were compared with the threshold value at α = 0.05, which Bonferroni was adjusted by the number of pro-inflammatory markers. In this way, a threshold value of p = 0.01 was obtained, which was defined as significant for this method.
Ethical Approval and Consent to participate
This study was approved by the ethic committee of the JLU medical faculty (Annex 1). Additionally, this study is part of a big project to investigate inflammatory factors and fatigue in patients with depression and multiple sclerosis. The code of this project in the ethic committee is AZ 81/18. Attached is the ethical approval and the informed consents (Annex 2, Annex 3) in its original language (German).
Data availability
The data that support the findings of this study are not publicly available due to the approved law of data protection from the European Union but are available from the corresponding author on strictly grounded reasonable requests.
References
World Health Organization. Depression and Other Common Mental Disorders. Institutes Heal. Natl., doi:CC BY-NC-SA 3.0 IGO (2017).
Wang, J. et al. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open 7, e017173 (2017).
World Health Organization. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research (1993).
Gądek-Michalska, A. & Bugajski, J. Interleukin-1 (IL-1) in stress-induced activation of limbic-hypothalamic-pituitary adrenal axis. Pharmacol. Reports 62, 969–982 (2010).
Henn, F. A. & Vollmayr, B. Stress models of depression: Forming genetically vulnerable strains. Neuroscience and Biobehavioral Reviews, https://doi.org/10.1016/j.neubiorev.2005.03.019 (2005).
Gui, W.-S. et al. Interleukin-1β overproduction is a common cause for neuropathic pain, memory deficit, and depression following peripheral nerve injury in rodents. Mol. Pain 12, 174480691664678 (2016).
Li, M. et al. Lentivirus-mediated interleukin-1β (IL-1β) knock-down in the hippocampus alleviates lipopolysaccharide (LPS)-induced memory deficits and anxiety- and depression-like behaviors in mice. J. Neuroinflammation 14, 1–12 (2017).
Rossi, S. et al. Neuroinflammation drives anxiety and depression in relapsing-remitting multiple sclerosis. Neurology 89, 1338–1347 (2017).
Diniz, B. S., Teixeira, A. L., Talib, L., Gattaz, W. F. & Forlenza, O. V. Interleukin-1β Serum Levels is Increased in Antidepressant-Free Elderly Depressed Patients. Am. J. Geriatr. Psychiatry 18, 172–176 (2010).
Markowitz, A. J. & Rabow, M. W. Palliative Management of Fatigue at the Close of Life: “It Feels Like My Body Is Just Worn Out”. JAMA 298, 217 (2007).
Yennurajalingam, S. & Bruera, E. Palliative Management of Fatigue at the Close of Life. JAMA 297, 295 (2007).
Brurberg, K. G., Fønhus, M. S., Larun, L., Flottorp, S. & Malterud, K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 4, e003973 (2014).
Watanabe, Y., Evengård, B., Natelson, B. H., Jason, L. A. & Kuratsune, H. Fatigue science for human health. Fatigue Science for Human Health, https://doi.org/10.1007/978-4-431-73464-2 (2008).
Scheibenbogen, C. et al. Chronisches Fatigue-Syndrom. Heutige Vorstellung zur Pathogenese, Diagnostik und Therapie. Tagliche Prax. (2014).
Matura, L. A., Malone, S., Jaime-Lara, R. & Riegel, B. A Systematic Review of Biological Mechanisms of Fatigue in Chronic Illness. Biol. Res. Nurs. 20, 410–421 (2018).
Nerurkar, L., Siebert, S., McInnes, I. B. & Cavanagh, J. Rheumatoid arthritis and depression: an inflammatory perspective. The Lancet Psychiatry 6, 164–173 (2019).
Bossola, M., Di Stasio, E., Giungi, S., Rosa, F. & Tazza, L. Fatigue Is Associated With Serum Interleukin-6 Levels and Symptoms of Depression in Patients on Chronic Hemodialysis. J. Pain Symptom Manage. 49, 578–585 (2015).
Bower, J. E. et al. Inflammation and Behavioral Symptoms After Breast Cancer Treatment: Do Fatigue, Depression, and Sleep Disturbance Share a Common Underlying Mechanism? J. Clin. Oncol. 29, 3517–3522 (2011).
Langgartner, D., Lowry, C. A. & Reber, S. O. Old Friends, immunoregulation, and stress resilience. Pflugers Archiv European Journal of Physiology, https://doi.org/10.1007/s00424-018-2228-7 (2019).
Raison, C. L. & Miller, A. H. Is Depression an Inflammatory Disorder? Curr. Psychiatry Rep. 13, 467–475 (2011).
Johannsen, A., Rylander, G., Söder, B. & Marie, Å. Dental Plaque, Gingival Inflammation, and Elevated Levels of Interleukin-6 and Cortisol in Gingival Crevicular Fluid From Women With Stress-Related Depression and Exhaustion. J. Periodontol. 77, 1403–1409 (2006).
Schrepf, A. et al. Cortisol and inflammatory processes in ovarian cancer patients following primary treatment: Relationships with depression, fatigue, and disability. Brain. Behav. Immun. 30, S126–S134 (2013).
Lim, W., Hong, S., Nelesen, R. & Dimsdale, J. E. The Association of Obesity, Cytokine Levels, and Depressive Symptoms With Diverse Measures of Fatigue in Healthy Subjects. Arch. Intern. Med. 165, 910 (2005).
Felger, J. C. & Lotrich, F. E. Inflammatory cytokines in depression: Neurobiological mechanisms and therapeutic implications. Neuroscience 246, 199–229 (2013).
Katsarou, Z. et al. Immune factors or depression? Fatigue correlates in Parkinson’s disease|?Factores inmunes o depresi?n? La fatiga relacionada con la enfermedad de Parkinson. Rev. Neurol. 45, 725–728 (2007).
Bull, S. J. et al. Functional polymorphisms in the interleukin-6 and serotonin transporter genes, and depression and fatigue induced by interferon-alpha and ribavirin treatment. Mol. Psychiatry 14, 1095–104 (2009).
Gaudiano, B. A., Young, D., Chelminski, I. & Zimmerman, M. Depressive symptom profiles and severity patterns in outpatients with psychotic vs nonpsychotic major depression. Compr. Psychiatry, https://doi.org/10.1016/j.comppsych.2008.02.007 (2008).
Shen, J. et al. Excessive daytime sleepiness and fatigue in depressed patients and therapeutic response of a sedating antidepressant. J. Affect. Disord. 134, 421–426 (2011).
Meyers, C. A., Albitar, M. & Estey, E. Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer, https://doi.org/10.1002/cncr.21234 (2005).
Cho, H. J., Kivimäki, M., Bower, J. E. & Irwin, M. R. Association of C-reactive protein and interleukin-6 with new-onset fatigue in the Whitehall II prospective cohort study. Psychol. Med. 43, 1773–1783 (2013).
Köhler, C. A. et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr. Scand. 135, 373–387 (2017).
Haapakoski, R., Mathieu, J., Ebmeier, K. P., Alenius, H. & Kivimäki, M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain. Behav. Immun. 49, 206–215 (2015).
Koelsch, S. et al. The impact of acute stress on hormones and cytokines, and how their recovery is affected by music-evoked positive mood. Sci. Rep., https://doi.org/10.1038/srep23008 (2016).
Cohen, S., Doyle, W. J. & Skoner, D. P. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosom. Med., https://doi.org/10.1097/00006842-199903000-00009 (1999).
Belluardo, N. Capítulo 36 - Interacciones entre el sístema nervioso y el sístema imunitario. In Fisiología Médica (Fiorenzo Conti, compilador) 707–711 (McGraw Hill, 2010).
Akdis, M. et al. Interleukins (from IL-1 to IL-38), interferons, transforming growth factor β, and TNF-α: Receptors, functions, and roles in diseases. J. Allergy Clin. Immunol. 138, 984–1010 (2016).
Akdis, M. et al. Interleukins, from 1 to 37, and interferon-γ: Receptors, functions, and roles in diseases. J. Allergy Clin. Immunol. 127, 701–721.e70 (2011).
Aswar, U., Chepurwar, S., Shintre, S. & Aswar, M. Telmisartan attenuates diabetes induced depression in rats. Pharmacol. Reports 69, 358–364 (2017).
Lenczowski, M. J. P. et al. Central administration of rat IL-6 induces HPA activation and fever but not sickness behavior in rats. Am. J. Physiol. Integr. Comp. Physiol. 276, R652–R658 (1999).
Raber, J., O’Shea, R. D., Bloom, F. E. & Campbell, I. L. Modulation of Hypothalamic–Pituitary–Adrenal Function by Transgenic Expression of Interleukin-6 in the CNS of Mice. J. Neurosci. 17, 9473–9480 (1997).
Himmerich, H. et al. Stress-induced cytokine changes in rats. Eur. Cytokine Netw. 24, 97–103 (2013).
Armario, A., Hernández, J., Bluethmann, H. & Hidalgo, J. IL-6 deficiency leads to increased emotionality in mice: evidence in transgenic mice carrying a null mutation for IL-6. J. Neuroimmunol. 92, 160–169 (1998).
Kiecolt-Glaser, J. K. & Glaser, R. Depression and immune function central pathways to morbidity and mortality. In Journal of Psychosomatic Research, https://doi.org/10.1016/S0022-3999(02)00309-4 (2002).
Vgontzas, A. N., Bixler, E. O. & Chorousos, G. P. Obesity-Related Sleepiness and Fatigue: The Role of the Stress System and Cytokines. Ann. N. Y. Acad. Sci. 1083, 329–344 (2006).
Schwarz, R., Krauss, O. & Hinz, A. Fatigue in the general population. Onkologie, https://doi.org/10.1159/000069834 (2003).
Woloshin, S. & Schwartz, L. M. Distribution of C-Reactive Protein Values in the United States. N. Engl. J. Med. 352, 1611–1613 (2005).
Maggio, M., Guralnik, J. M., Longo, D. L. & Ferrucci, L. Interleukin-6 in Aging and Chronic Disease: A Magnificent Pathway. Journals Gerontol. Ser. A 61, 575–584 (2006).
Slade, G. D. et al. Relationship between periodontal disease and C-reactive protein among adults in the atherosclerosis risk in communities study. Arch. Intern. Med., https://doi.org/10.1001/archinte.163.10.1172 (2003).
Kushner, I., Rzewnicki, D. & Samols, D. What does minor elevation of C-reactive protein signify? American Journal of Medicine, https://doi.org/10.1016/j.amjmed.2005.06.057 (2006).
Giles, J. T. et al. Association of body fat with C-reactive protein in rheumatoid arthritis. Arthritis Rheum., https://doi.org/10.1002/art.23766 (2008).
Berthold-Losleben, M. & Himmerich, H. The TNF-α System: Functional Aspects in Depression, Narcolepsy and Psychopharmacology. Curr. Neuropharmacol. 6, 193–202 (2008).
Bobińska, K., Gałecka, E., Szemraj, J., Gałecki, P. & Talarowska, M. Is there a link between TNF gene expression and cognitive deficits in depression? Acta Biochim. Pol. 64 (2017).
Pan, W. et al. Cytokine Signaling Modulates BBB Function. Curr Pharm Des. 17, 3729–3740 (2014).
Mikhaylova, I. V., Kuulasmaa, T., Jääskeläinen, J. & Voutilainen, R. Tumor necrosis factor-α regulates steroidogenesis, apoptosis, and cell viability in the human adrenocortical cell line NCI-H295R. Endocrinology, https://doi.org/10.1210/en.2006-0726 (2007).
Warren, E. J. et al. Coincidental changes in behavior and plasma cortisol in unrestrained pigs after intracerebroventricular injection of tumor necrosis factor-α. Endocrinology https://doi.org/10.1210/endo.138.6.5180 (1997).
Moss, R. B., Mercandetti, A. & Vojdani, A. TNF-alpha and chronic fatigue syndrome. J. Clin. Immunol. (1999).
Menon, R., Allen, C., Forbes, S., Hunt, D. & Lewis, H. Haematology and immunology. In MRCP Part 2: 450 BOFs, https://doi.org/10.5005/jp/books/11984_5 (2013).
Demyttenaere, K., De Fruyt, J. & Stahl, S. M. The many faces of fatigue in major depressive disorder. Int. J. Neuropsychopharmacol. 8, 93–105 (2005).
Norheim, K. B., Jonsson, G. & Omdal, R. Biological mechanisms of chronic fatigue. Rheumatology (Oxford, England), https://doi.org/10.1093/rheumatology/keq454 (2011).
Christensen, L. & Duncan, K. Distinguishing depressed from nondepressed individuals using energy and psychosocial variables. J. Consult. Clin. Psychol. 63, 495–498 (1995).
Lewinsohn, P. M., Hoberman, H. M. & Rosenbaum, M. A prospective study of risk factors for unipolar depression. J. Abnorm. Psychol. 97, 251–264 (1988).
Couch, Y., Xie, Q., Lundberg, L., Sharp, T. & Anthony, D. C. A model of post-infection fatigue is associated with increased TNF and 5-HT2A receptor expression in mice. PLoS One 10, 1–16 (2015).
Gold, S. M. et al. Endocrine and immune substrates of depressive symptoms and fatigue in multiple sclerosis patients with comorbid major depression. J. Neurol. Neurosurg. Psychiatry 82, 814–818 (2011).
Davis, M. C. et al. Chronic stress and regulation of cellular markers of inflammation in rheumatoid arthritis: Implications for fatigue. Brain. Behav. Immun. 22, 24–32 (2008).
Härter, M., Berger, M., Schneider, F. & Ollenschläger, G. S3 Praxisleitlinien in Psychiatrie und Psychotherapie Nationale VersorgungsLeitlinie Unipolare Depression. Nervenheilkunde (2010).
Robert Koch Institut. RKI - Gesundheit A-Z - Robert Koch-Institut zum Weltgesundheitstag 2017: Daten und Fakten zu Depressionen. (2017). Available at: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GesundAZ/Content/D/Depression/Daten_Fakten/daten_fakten_depressionen_inhalt.html (Accessed: 28th November 2019).
Kliem, S., Mößle, T., Zenger, M. & Brähler, E. Reliability and validity of the beck depression inventory-fast screen for medical patients in the general German population. J. Affect. Disord., https://doi.org/10.1016/j.jad.2013.11.024 (2014).
Häuser, W., Almouhtasseb, R., Muthny, F. A. & Grandt, D. Validierung der Deutschen Version der Fatigue Impact Scale FIS-D. Z. Gastroenterol. 41, 973–982 (2003).
Morris, P. E. & Fritz, C. O. Effect sizes in memory research. Memory, https://doi.org/10.1080/09658211.2013.763984 (2013).
Cambridge, U. of. Rules of thumb on magnitudes of effect sizes. 2019 Available at: http://imaging.mrc-cbu.cam.ac.uk/statswiki/FAQ/effectSize (Accessed: 21st February 2020).
Acknowledgements
This study is part of the doctoral thesis of Bruno Pedraz-Petrozzi, M.D. (Ph.D. student). The authors would like to thank Jil Seifert, M.Sc., for her involvement in the data collection and Bernd Hanewald, M.D., and his team for support in patient recruitment. We thank the Department of Internal Medicine and Rheumatology at the JLU for assistance in analyzing blood samples. Specially, we would like to thank Ms. Carina Scheiyäck and Ms. Mona Arnold from this department for supporting us in the procedure of blood sample analysis. This study was carried out with the support of DAAD (German Academic Exchange Service) and the Foundation “Immunität und Seele”. This study is part of the doctoral thesis (Ph.D.) of Mr. Bruno Pedraz-Petrozzi, M.D. Mr. Pedraz-Petrozzi have received a financial support from the German Exchange Academic Program (DAAD) for a Ph.D.-Program. This program included also the financial support of the project, that involved mainly material expenses and participants’ expenses for participation. Additionally, Mr. Pedraz-Petrozzi contacted the owner of the “Immunität und Seele” foundation, that awarded this project and supported financially the assessment of ELISAs (inflammatory parameters). Both supporters have no role in the design of the study, data collection, analysis and interpretation of results.
Author information
Authors and Affiliations
Contributions
B.P.P. Information: Third-year doctoral candidate, medical doctor, Justus-Liebig University Giessen. Research Group Cognitive Neurosciences at the Center for Psychiatry and Psychotherapy in Giessen. Student at the Giessen Graduate Life Sciences School (GGL). Contribution: This is the corresponding author and BPP is responsible for everything concerning the submission process on behalf of all authors of the paper. Additionally, BPP wrote the introduction, methods, results, discussion and conclusions. Corrected the manuscript, did the data analysis and the literature search. E.N. Information: Second doctoral supervisor (co-supervisor) of BPP. Private Lecturer (Privatdozent) of the Department of Internal Medicine and Rheumatology, Campus Kerckhoff, JLU, Bad Nauheim, Germany. Co-supervisor of the doctoral thesis of Mr. BPP. Member of the Section 2, Infection and Immunity, Giessen Graduate Life Sciences School (GGL). Contribution: Corrected the manuscript, helped with the data analysis, mentored the methods (specifically in molecular biology matters) and helped with the discussion of the paper, proofreading and paper mentoring. G.S. Information: Principal doctoral supervisor of BPP. Professor at the Faculty of Medicine and Psychology from the Justus-Liebig University, Giessen. Group Leader of the Cognitive neuroscience working group. Member of the Section 5, Neurosciences, Giessen Graduate Life Sciences School (GGL). Contribution: Corrected the manuscript for the resubmission, helped with the data analysis, mentored the methods (specifically in topics that corresponded to depression and fatigue) and helped with the discussion, proofreading and paper mentoring.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pedraz-Petrozzi, B., Neumann, E. & Sammer, G. Pro-inflammatory markers and fatigue in patients with depression: A case-control study. Sci Rep 10, 9494 (2020). https://doi.org/10.1038/s41598-020-66532-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66532-6
This article is cited by
-
Effects of left anodal transcranial direct current stimulation on hypothalamic–pituitary–adrenal axis activity in depression: a randomized controlled pilot trial
Scientific Reports (2023)
-
Acupuncture improves immunity and fatigue after chemotherapy in breast cancer patients by inhibiting the Leptin/AMPK signaling pathway
Supportive Care in Cancer (2023)
-
Factors associated with habitual sleep duration in US adults with hypertension: a cross-sectional study of the 2015–2018 National Health and Nutrition Examination Survey
BMC Public Health (2022)
-
Fractional anisotropy and peripheral cytokine concentrations in outpatients with depressive episode: a diffusion tensor imaging observational study
Scientific Reports (2022)
-
Exploring the links among inflammation and gut microbiome with psychoneurological symptoms and gastrointestinal toxicities in gynecologic cancers: a systematic review
Supportive Care in Cancer (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.