Key Points
-
Preventive dental screening reduces the incidence of MRONJ/BRONJ.
-
A cross-service cross-healthcare boundary preventive pathway was developed.
-
Alternative ways of delivering specialist led MRONJ/BRONJ preventive services can be successful with a robust clinical governance framework.
Abstract
Introduction Bisphosphonates and denosumab reduce the risk of skeletal events in some malignancies (for example, breast, myeloma). These drugs carry a significant risk of a difficult-to-manage side effect of medication related osteonecrosis of the jaw (MRONJ). Preventive dental screening and treatment reduces the incidence of MRONJ. A managed clinical network (MCN) has been used to provide a MRONJ risk reduction pathway. A 360 degree survey was undertaken to assess the effectiveness of the pathway.
Aim The aim of the 360 degree survey was to evaluate if this preventive pathway fulfilled its aims based on patient and stakeholder responses.
Method A multidisciplinary, cross-service, cross-health board MRONJ preventive pathway has been developed. A 360 degree feedback survey of patients and other stakeholders was undertaken.
Results Overall, this survey revealed high levels of satisfaction across patients, oncologists, community dental services, general dental services, and hospital managers.
Conclusion Alternative ways of delivering MRONJ preventive pathways can be developed and assessed using iterative stakeholder feedback aided by a robust clinical governance framework.
Similar content being viewed by others
Introduction
Medication related osteonecrosis of the jaw (MRONJ) is a rare complication associated with some drugs. The condition has undergone changes in nomenclature. It was first reported by Marx (2003) as bisphosphonate related osteonecrosis of the jaw (BRONJ)1 and later referred to as anti-resorptive agent related osteonecrosis of the jaw (ARONJ).2 BRONJ (BONJ) is defined as exposed, necrotic bone in the maxilla or mandible that has persisted for more than eight weeks in patients taking bisphosphonates and where there has been no history of radiation therapy to the jaw.3 The change in nomenclature to MRONJ was justified to accommodate the growing number of osteonecrosis cases involving the maxilla and mandible associated with other anti-resorptive and anti-angiogenic therapies.4
Patients who take bisphosphonates or denosumab as part of treatment for a malignant condition are among those who are at a higher risk of developing osteonecrosis of the jaw (ONJ).4 There are varying reports of incidence rates ranging from 1.5%5 to 28%.6
There is normally a greater urgency for initiating such drug therapy in patients with malignancy in comparison to the other patient groups. These drugs help to reduce the risk of significant skeletal morbidity associated with malignancy7.
Dental risk factors for developing MRONJ include dental extractions, dento-alveolar surgery and trauma from dentures in the higher risk groups. MRONJ symptoms include delayed healing following a dental extraction or other oral surgery, pain, soft tissue infection and swelling, numbness, paraesthesia or exposed bone.
The American Association of Oral and Maxillofacial Surgeons (AAOMS) has recommended stage specific treatment recommendations for MRONJ.4 These range from conservative management to surgical debridement or wide excision. Ristow et al.8 argue for surgical treatment as this has superior results. While MRONJ can be treated, management of MRONJ is complicated. It remains difficult to treat because drug cessation does always not cure the problem, as the drugs remains bound in bone for several months9 (denosumab) to several years10 (bisphosphonates). Medical and surgical treatment for MRONJ is invasive, expensive and can adversely impact on patients' quality of life.
Preventive dental screening and treatment reduces the incidence of MRONJ.11
There was no previous pathway in the authors' health board for oncologists to refer patients for dental screening before commencing drug therapy. The Hospital Dental Services (HDS) could not provide timely screening unless there was a significant increase in resources. Dentists in general practice did not have timely information regarding the oncological treatment or specific guidance on screening these patients.
There were some serious concerns about the status quo including:
-
1
Patients suffering with MRONJ in the middle of oncology therapies
-
2
A lack of timely and effective communication between oncologists and dentists
-
3
Failures in communication in relation to this group of patients across three different health boards who referred to the same maxillofacial unit
-
4
Lack of access to dental care for unregistered patients in the MRONJ risk groups
-
5
Difficulties in identifying and treating established MRONJ cases in a timely manner due to inflexible patient administration systems
-
6
Clinical governance issues
-
7
Possible medico-legal issues.
Multi-professional discussions among the local Clinical Governance group and Special Care Dentistry Managed Clinical Network led to the development of an MRONJ risk reduction pathway. The consensus within the groups was to target patients who were undergoing treatment for a malignant condition as the highest priority group initially.
Aim
The MRONJ risk reduction pathway aimed to
-
1
Enable rapid access high quality preventive dental treatment and improve access to services locally for patients undergoing drug therapy for some cancers, who were at a higher risk of developing MRONJ
-
2
Enable timely and effective communication between oncologists, maxillofacial surgeons and dentists across three health boards. Dentists involved in the pathway work in all three arms of the services, ie:
-
General dental services (GDS)
-
Community dental services (CDS) and
-
Hospital dental services (HDS)
-
1
Reduce reliance on secondary care dental services; but within a robust clinical governance framework.
Method
Setting
The health boards (HB) involved included Abertawe Bro Morgannwg University (ABMU), Hywel Dda and Powys. ABMU is referred to as the primary HB in the report of the survey below. The specialist maxillofacial unit in the primary HB is the referral centre for all cases of MRONJ across all three HBs. The maxillofacial unit comprises consultants and specialists in maxillofacial surgery, restorative dentistry, orthodontics and special care dentistry. Special care dentistry services are delivered in close collaboration with the community dental services in the primary HB.
A multidisciplinary, cross-service, cross-health board MRONJ preventive pathway was initiated in 2012 and developed over two years. The overarching strategy was to enable oncologists to refer patients to their own dentists locally for dental screening and/or dental treatment before drug therapy that increased the risk of MRONJ. A vital part of the strategy was to enable this to be done in a timely way within a supportive specialist led framework.
The following groups and organisations were approached for feedback during pathway development:
-
Maxillofacial unit directorate within the primary HB
-
Oncology directorates within the primary HB
-
Special care dentistry managed clinical network representatives across all arms of the dental services (that is, HDS, CDS and HDS) across two health boards (ABMU and Hywel Dda)
-
Clinical governance group in the primary HB
-
An indemnifying body regarding medico-legal aspects of the pathway
-
Clinical online information network pathway development group within the primary HB.
A job plan was revised in order to establish the role of a part-time Band 512 oncology coordinator within the maxillofacial unit to serve as a central point of contact in the primary HB. The oncology coordinator also facilitated communication in a similar manner for head and neck oncology patients.
Access to dental care remains a major barrier to enabling care. Therefore, particular attention was paid to removing this barrier and mechanisms were put in place to enable dental care for those patients who were not registered with a dentist. This was accomplished by networked care with the community dental services in three health boards. Protocols for urgent referrals from dentists to secondary care for opinion/ treatment were formalised. This was supported by customised postgraduate training and resource packs for CDS dentists, GDS dentists and oncology teams across all three HBs.
Once the pathway was well established in the primary HB, it was cascaded in a similar manner to two neighbouring HBs who have smaller patient numbers, in accordance with the 1,000 lives methodology.13
An anonymised 360 degree stakeholder survey was undertaken in 2015 after the pathway had been functional for one year. This was facilitated by the Patient Experience Unit in the primary HB.
Results
-
A total of 99 referrals for dental screening were generated by oncologists in the period September 2014 to November 2015, for patients awaiting IV bisphosphonate or denosumab therapy
-
Referrals were received from haematology and oncology departments in three different HBs
-
Two patients were unable to attend dental screening due to ill health
-
Seventy-five (75%) patients were screened in the GDS. Thirty-seven (49%) of these did not require any further dental treatment before drug therapy commenced
-
Eight (8%) patients were screened in CDS in the ABMU (primary) HB
-
Seven (7%) patients were screened in the CDS in Hywel Dda and one (1%) patient was screened in the CDS in Powys HB
-
Only 8% of patients who were referred by oncologists needed to be seen within secondary care in the HDS
-
Over 90% of patients were satisfied with the new pathway
-
All CDS dentists and 75% of GDS dentists were satisfied with the new pathway
-
All oncologists were satisfied with the new pathway.
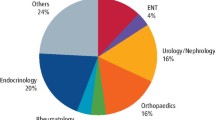
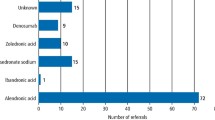
Results can be seen in Figures 1,2,3,4. Only 8% of patients referred for screening needed to be seen in the Hospital Dental Services. The remaining 92% were screened and managed in the General Dental Services and Community Dental Services. Overall, 83% of patients were very satisfied with their dental treatment. Nearly 88% of GDS dentists expressed satisfaction at providing treatment for high risk of MRONJ patients.
Examples of literal comments from patients:
'I have regular checkups; appointments are always easy to walk'
'I found it difficult to find a place in dental practices'
'I am in a dental insurance scheme'
'Having moved to Llanelli from Pontypridd I found I could not get on an NHS, because I have cancer I was seen in the _____(a CDS clinic- authors own comment).'
'Make all NHS dental services as good as good as private one'
'Dentists keep changing, I find this frustrating.'
'We are in a private dentist so we don't wait long but other people in different system would have to wait longer. Treatment doesn't always start straight away.'
'Very satisfied with treatment with oncology and dental treatment, keep up the good work.'
Discussion
Intravenous bisphosphonates are anti-resorptive medications used to manage cancer related conditions including hypercalcaemia of malignancy, skeletal related events associated with bony metastases in the context of solid tumours such as breast cancer, prostate cancer and lung cancers and for management of lytic lesions in the setting of multiple myeloma.14 RANK ligand inhibitor (denosumab) is an anti-resorptive agent that is also effective in reducing skeletal related events in relation to metastatic bone disease from solid tumours.15 In contrast to bisphosphonates, RANK ligand inhibitors do not bind to bone and their effects on bony remodelling are mostly diminished within six months of treatment cessation.4 Both these drugs are also widely used in smaller doses for the management of osteoporosis.16,17
Anti-angiogenic medications are novel medications that have demonstrated efficacy in the treatment of gastro-intestinal tumours, renal cell carcinomas, neuro-endocrine tumours and others.
These drugs carry a significant risk of a difficult-to-manage side effect of MRONJ. The AAOMS position paper gives a detailed analysis of the estimation of risk based on several factors.4 Overall, the risk of osteonecrosis of the jaw (ONJ) among cancer patients exposed to zolendronate and denosumab is 50-100 times higher than those exposed to placebo. In contrast, the risk of developing ONJ in osteoporotic patients exposed to oral, IV bisphosphonates or denosumab for the management of osteoporosis is real but remains very low. Concomitant use of corticosteroids is associated with an increased risk of MRONJ.
This particular patient group was targeted for the risk reduction pathway, as they are the highest risk group to develop ONJ and have the maximum pressures on patients and clinicians for undertaking drug therapy urgently. Success rates for conservative treatment of MRONJ range from 20% to 50%. Therapy success of 85% is estimated for surgical approaches to management of MRONJ. It remains to be seen if this preventive pathway reduces the incidence of MRONJ in this unit.
There is limited evidence on similar MRONJ preventive pathways in the rest of the UK. Taylor et al. (2013)19 reported on the screening protocol at King's College Hospital It would appear that patients taking bisphosphonates were referred by colleagues to a bisphosphonate clinic by colleagues in other departments within the dental hospital and also by oncology, rheumatology, orthopaedic out-patients, GMPs (general medical practitioners) and GDPs. Patients were assessed by a multidisciplinary specialist team including two oral surgeons and two consultants in restorative dentistry. The assessment, investigations, treatment planning and any necessary treatment was undertaken in the hospital. This provided valuable information on the incidence and risk factors associated with BRONJ. Patel et al. (2015)20 have reported a service review of a specialist screening clinic before intravenous bisphosphonates for cancer. The high treatment needs in the group of patients is highlighted, along with the need to prioritise certain sub-groups with poor life-expectancy for symptom relief. The authors report that they did not follow patients to review if their dental status remained healthy. The issue with access to care is highlighted. While the specialist service provided the necessary treatment before drug therapy, it would appear that access to continuing care outside the hospital dental services may have remained a problematic issue. This service review also highlights that some patients with a 'regular GDP' were assessed by their own dentist.
There are an estimated 150 new prescriptions per year in ABMU HB for intravenous bisphosphonates and denosumab as part of the treatment of cancer. A total of 99 referrals were made for dental assessment during the observation period. This information was accessible through the pharmacy's ChemoCare software.21 This was a 66% referral rate during the initial phase of implementation. The oncology teams at ABMU HB now have a 100% referral rate due to incorporation of the pathway with the Chemocare software In addition, there is a retrospective cohort of patients who have been prescribed these drugs. A specialist screening clinic would have necessitated considerable investment in clinical resources. In the absence of such resources, this pathway provided a novel approach to provide dental screening and prevention along with continuing care in a specialist led framework. Invariably, there are situations where a GDS or CDS dentist may require specialist advice or treatment from a hospital based specialist. This was addressed by a local agreement to see this higher risk group of patients within six weeks of referral for treatment planning and treatment. Ideally, this period should be shorter, but current resources only enable this minimum period. This merits further improvements in the referral process.
Patel et al. (2015)20 suggest that some of these patients may have additional needs such as wheelchair users. Dental surgeries must comply with the Equality act (2010).22 Therefore, this in itself should not pose a barrier to accessing care. They also highlight the concern that some GDPs may not have the knowledge or confidence to treat medically complex patients in primary care. Our survey revealed that 92% of patients in this sample were screened by GDS/CDS dentists. It would appear that this particular patient cohort can largely be managed within the GDS/CDS despite their medical complexity. Additionally, in the majority of cases, the dental assessment and treatment itself is within the everyday remit of GDPs' provided clear local guidance and specialist support is easily accessible. In addition, if a patient has been in a continuing care arrangement, the dentist and patient are likely to be aware of any teeth of dubious prognosis that have been monitored. The well informed and supported dentist can now be in a position to discuss the risks and benefits of an extraction before drug therapy and even undertake the necessary treatment. This pathway allows for urgent referral for advice, treatment planning or treatment where the complexity of care exceeds the knowledge, skills or confidence of the referring practitioner. This preventive pathway also considers this need for ongoing and continuing care. There is an embedded mechanism for the patients without a 'regular' dentist to be stabilised within the CDS/HDS and then move on to a shared care arrangement or GDS/CDS care.
There is national guidance on undertaking extractions in the high risk MRONJ group.3 In addition, local guidance was also disseminated with details including risk assessment, antibiotic prophylaxis and referral pathways. The oncology coordinator continues to act as a central point of contact. There is some evidence from nursing research literature to support the vital role played by a coordinator in the care of children with complex needs and in the discharge process.23,24,25 The success of this pathway relies heavily on the oncology coordinator. In our opinion, key requisites for this role would include excellent communication skills, organisational skills and an understanding of audit methodology.
The South Wales Managed Clinical Network in Special Care Dentistry26 was crucial in enabling access to care for those patients who did not have their own dentist. Managed clinical networks are linked groups of health professionals from primary, secondary and tertiary care, working in a coordinated manner, unconstrained by existing professional and trust/health authority boundaries, to ensure equitable provision of high quality and clinically effective services.27
Further improvements were made in the pathway as part of an iterative process of improvement by incorporating the referral letter from haematologists within the ChemoCare system and enabling electronic copies of the referral form to be sent to the oncology coordinator.
In addition, the maxillofacial unit has developed protocols to measure the incidence of MRONJ complication. Some of the literal comments from patients also gave a realistic picture of how patients perceive different types of dental service and areas for improvement.
This risk reduction pathway incorporates the principles of prudent healthcare,28 ie:
-
1
Care for those with the greatest health need first
-
2
Do only what is needed and do no harm
-
3
Reduce inappropriate variation through evidence-based approaches.
Conclusion
Certain drug therapies used in some cancer patients have a high risk of causing a complication of MRONJ which can adversely affect quality of life. This is difficult, invasive and expensive to treat. Dental screening and treatment before commencing such drug therapy can reduce the risk of MRONJ.2 An innovative collaborative, cross-service, cross health board MRONJ risk reduction pathway has been developed and been shown to work seamlessly across organisations. This patient and stakeholder survey reported high levels of satisfaction with the new MRONJ preventive pathway. There was reduced reliance on secondary care services and reduced disruption of oncology treatment schedules. This MRONJ risk reduction pathway provides timely access to dental care locally for patients with high risk treatment needs, within a robust clinical governance framework.
References
Marx R E . Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115–1117.
Hellstein J W, Adler R A, Edwards B et al. Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: Executive summary of recommendations from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2011; 142: 1243–1251.
Scottish Dental Clinical Effectiveness Programme. Oral Health Management of Patients Prescribed Bisphosphonates. Dundee: NHS Education for Scotland 2011.
Ruggiero S L, Dodson T B, Fantasia J et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the Jaw 2014 update. J Oral Maxillofac Surg 2014; 72: 1938–1956.
Ibrahim T, Barbanti F, Giorgio-Marrano G et al. Osteonecrosis of the jaw in patients with bone metastases treated with bisphosphonates a retrospective study. Oncologist 2008; 13: 330–336.
Boonyapakorn T, Schirmer I, Reichart P A, Sturm I, Massenkeil G . Bisphosphonate induced osteonecrosis of the jaws: prospective study of 80 patients with multiple myeloma and other malignancies. Oral Oncol 2008; 44: 857–869.
Ramaswamy B, Shapiro C L . Bisphosphonates in the prevention and treatment of bone metastases. Oncology (Williston Park) 2003; 17: 1261–1270.
Ristow O, Otto S, Troeltzsch M, Hohlweg-Majert B, Pautke C . Treatment perspectives for medication related Osteonecrosis of the jaw (MRONJ). J Craniomaxillofac Surg 2015; 43: 290–293.
Bekker P J, Holloway D L, Rasmussen A S et al. A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res 2004; 19: 1059–1066.
Lin J H . Bisphosphonates: a review of their pharmacokinetic properties. Bone 1996; 18: 75–85.
Ripamonti C I, Maniezzo M, Campa T et al. Decreased occurrence of osteonecrosis of the jaw after implementation of dental preventive measures in solid tumour patients with bony metastases treated with bisphosphonates. The experience of the National Cancer institute of Milan. Ann Oncol 2009; 20: 137–145.
Agenda for change - NHS pay rates. Available at: https://www.healthcareers.nhs.uk/about/careers-nhs/nhs-pay-and-benefits/agenda-change-pay-rates (accessed 21/2/17).
1000 lives. Improving Quality Together. Available at http://www.1000livesplus.wales.nhs.uk/iqt (accessed 21/2/17).
Hillner B E, Ingle J N, Chlebowski R T et al. American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 2003; 21: 4042–4057.
Stopeck A, Body J J, Fujiwara Y et al. Denosumab versus zoledronic acid for the treatment of breast cancer patients with bone metastases: results of a randomised phase 3 study. Eur J Cancer Supplements (EJC supplements) 2009; 7: 2–3.
Watts N B . Bisphosphonate treatment of osteoporosis. In: Osteoporosis. pp 459–473. Humana Press, 2003.
Cummings S R, San Martin J, Mc Clung M R et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Eng J Med 2009; 361: 756–765.
Graziani F, Vescovi P, Campisi G et al. Resective surgical approach shows a high performance in the managemernt of advanced cases of bisphoshphonate related osteonecrosis of the jaws: a restrospective survey of 347 cases. J Oral Maxillofac Surg 2012; 70: 2501–2507.
Taylor T, Bryant C, Popat S . A study of 225 patients on bisphosphonates presenting to the bisphosphonate clinic at King's college hospital. Br Dent J 2013; 214: E18.
Patel D, Burke M, Shahabi Z, Kerr B . A service review investigating dental extractions in a specialist screening clinic before intravenous bisphosphonates for patients with cancer. J Disabil Oral Health 2015; 16: 54–58.
CIS Oncology. ChemoCare. Available at: http://www.cis-healthcare.com/about_cis/ (accessed 21/2/17).
Equality Act 2010, c.15 (Eng.).
Tait T, Beattie A, Dejnega S . Service coordination: a successful model for the delivery of multi-professional services for children with complex needs. NT Res 2002; 7: 19–32.
Day M R, McCarthy G, Coffey A . Discharge planning: the role of the discharge coordinator. Nurs Older People 2009; 21: 26–32.
Spears J . The role of the discharge coordinator in oncology. Cancer Nursing Practice 2014; 13: 21–26.
Special Care Dentistry in Wales implementation plan 2011. (Wales).
Baker C D, Lorimer A R . Cardiology: The development of a managed clinical network. Br Med J 2000; 321: 1152–1153.
Simply prudent healthcare. Bevan Commission 2013 (Wales).
Acknowledgements
The authors wish to thank the oncologists, haematologists, members of the Clinical Governance group, SCD MCN, Maxillofacial unit, and dentists in the CDS and GDS in all three health boards for their feedback and commitment to the pathway.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Muthukrishnan, A., Al-Ismail, S., Bertelli, G. et al. MRONJ risk reduction pathway - 360 degree survey. Br Dent J 222, 386–390 (2017). https://doi.org/10.1038/sj.bdj.2017.225
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.225