Abstract
Objective
To perform a systematic review and meta-analysis to estimate the effect of endometriosis on preterm birth (PB) risk.
Methods
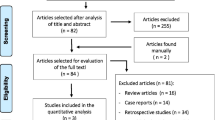
Searches were conducted in PubMed-MEDLINE, Embase, Scopus, Web of Science, Cochrane Library, Google Scholar, and SciELO for studies published in all languages from inception through April 2017. We included cohort studies evaluating pregnant women with and without endometriosis and conception either by spontaneous conception (SC) or with assisted reproductive technology (ART). Primary outcome was PB (<37 weeks), and secondary outcomes were intrauterine growth restriction (IUGR), low birthweight, small for gestational age (SGA), and birthweight. Pooled odds ratios (ORs) and its 95% confidence interval (CI) were calculated as effects, and random-effects models were used for meta-analyses. Risk of bias was assessed with the Newcastle-Ottawa Scale, and heterogeneity of effects among studies was described with the I2 statistic.
Results
We identified 9 cohort studies including a total of 1 496 715 pregnancies (13 798 with endometriosis diagnosis). In women with endometriosis, the PB risk was significantly increased in both SC (OR: 1.59; 95% CI: 1.32-1.90) and ART (OR: 1.43; 95% CI: 1.14-1.79). The SGA risk was increased in women with endometriosis (OR: 1.16; 95% CI: 1.05-1.28), while the IUGR and low birthweight risks and birthweight were not affected by endometriosis.
Conclusion
Endometriosis is associated with increased PB risk in both SC and women who obtained pregnancy using ART. Prospective studies evaluating relevant outcomes are needed to confirm these results.
Similar content being viewed by others
References
Petraglia F, Arcuri F, de Ziegler D, Chapron C. Inflammation: a link between endometriosis and preterm birth. Fertil Steril. 2012;98(1):36–40.
Brosens I, Pijnenborg R, Benagiano G. Defective myometrial spiral artery remodelling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta. 2013;34(2):100–105.
Tu FF, Du H, Goldstein GP, Beaumont JL, Zhou Y, Brown WJ. The influence of prior oral contraceptive use on risk of endome-triosis is conditional on parity. Fertil Steril. 2014;101(6):1697–1704.
Ahn SH, Khalaj K, Young SL, Lessey BA, Koti M, Tayade C. Immune-inflammation gene signatures in endometriosis patients. Fertil Steril. 2016;106(6):1420–1431.e7.
Barbara G, Facchin F, Buggio L, et al. What is known and unknown about the association between endometriosis and sexual functioning: a systematic review of the literature. Reprod Sci. 2017;24(12):1566–1576.
Mishra VV, Bandwal P, Agarwal R, Aggarwal R. Prevalence, clinical and laparoscopic features of endometriosis among infertile women. J Obstet Gynaecol India. 2017;67(3):208–212.
Guler I, Erdem A, Oguz Y, et al. The impact of laparoscopic surgery of peritoneal endometriosis and endometrioma on the outcome of ICSI cycles. Syst Biol Reprod Med. 2017;63(5):324–330.
Vercellini P, Parazzini F, Pietropaolo G, Cipriani S, Frattaruolo MP, Fedele L. Pregnancy outcome in women with peritoneal, ovarian and rectovaginal endometriosis: a retrospective cohort study. BJOG. 2012;119(12):1538–1543.
Exacoustos C, Lauriola I, Lazzeri L, De Felice G, Zupi E. Complications during pregnancy and delivery in women with untreated rectovaginal deep infiltrating endometriosis. Fertil Steril. 2016;106(5):1129–1135.e1.
Jacques M, Freour T, Barriere P, Ploteau S. Adverse pregnancy and neo-natal outcomes after assisted reproductive treatment in patients with pelvic endometriosis: a case-control study. Reprod Biomed Online. 2016;32(6):626–634.
Leone Roberti Maggiore U, Ferrero S, Mangili G, et al. A systematic review on endometriosis during pregnancy: diagnosis, misdiagnosis, complications and outcomes. Hum Reprod Update. 2016;22(1):70–103.
Macer ML, Taylor HS. Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin North Am. 2012;39(4):535–549.
Palomba S, Homburg R, Santagni S, La Sala GB, Orvieto R. Risk of adverse pregnancy and perinatal outcomes after high technology in fertility treatment: a comprehensive systematic review. Reprod Biol Endocrinol. 2016;14(1):76.
Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril. 2012;98(4):922–928.
Hamdan M, Omar SZ, Dunselman G, Cheong Y. Influence of endometriosis on assisted reproductive technology outcomes: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(1):79–88.
Qin J, Liu X, Sheng X, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril. 2016;105(1):73–85.e1-6.
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341.
Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Ottawa, Canada: Ottawa Health Research Institute; 2011. http://www.ohri.ca/programs/clinical_epidemiology/ oxford.htm. Accessed 18 August 2017
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions; 2011. http://training.cochrane.org/hand book. Accessed 18 August 2017
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple graphical test. BMJ. 1997;315(7109):629–634.
Cochrane Collaboration. Review Manager (RevMan), Version 5. 2. Copenhagen: The Nordic Cochrane Centre; 2011.
Carassou-Maillan A, Pouly JL, Mulliez A, et al. Adverse pregnancy outcomes after Assisted Reproduction Technology in women with endometriosis [in French]. Gynecol Obstet Fertil. 2014;42(4):210–215.
Fernando S, Breheny S, Jaques AM, Halliday JL, Baker G, Healy D. Preterm birth, ovarian endometriomata, and assisted reproduction technologies. Fertil Steril. 2009;91(2):325–330.
Fujii T, Wada-Hiraike O, Nagamatsu T, et al. Assisted reproductive technology pregnancy complications are significantly associated with endometriosis severity before conception: a retrospective cohort study. Reprod Biol Endocrinol. 2016;14(1):73.
Glavind MT, Forman A, Arendt LH, Nielsen K, Henriksen TB. Endometriosis and pregnancy complications: a Danish cohort study. Fertil Steril. 2017;107(1):160–166.
Kuivasaari-Pirinen P, Raatikainen K, Hippeläinen M, Heinonen S. Adverse outcomes of IVF/ICSI pregnancies vary depending on aetiology of infertility. ISRN Obstet Gynecol. 2012;2012:451915.
Mannini L, Sorbi F, Noci I, et al. New adverse obstetrics outcomes associated with endometriosis: a retrospective cohort study. Arch Gynecol Obstet. 2017;295(1):141–151.
Mekaru K, Masamoto H, Sugiyama H, et al. Endometriosis and pregnancy outcome: are pregnancies complicated by endometrio-sis a high-risk group? Eur J Obstet Gynecol Reprod Biol. 2014;172:36–39.
Stephansson O, Kieler H, Granath F, Falconer H. Endometriosis, assisted reproduction technology, and risk of adverse pregnancy outcome. Hum Reprod. 2009;24(9):2341–2347.
Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H. Adverse pregnancy and birth outcomes associated with underlying diagnosis with and without assisted reproductive technology treatment. Fertil Steril. 2015;103(6):1438–1445.
Maignien C, Santulli P, Gayet V, et al. Prognostic factors for assisted reproductive technology in women with endometriosis-related infertility. Am J Obstet Gynecol. 2017;216(3):280.e1–280.e9.
Park JS, Park CW, Lockwood CJ, Norwitz ER. Role of cytokines in preterm labor and birth. Minerva Ginecol. 2005;57(4):349–366.
Romero R, Dey SK, Fisher SJ. Preterm labor: one syndrome, many causes. Science. 2014;345(6198):760–765.
Holzman C, Lin X, Senagore P, Chung H. Histologic chorioam-nionitis and preterm delivery. Am J Epidemiol. 2007;166(7):786–794.
Munrós J, Martínez-Zamora MA, Tàssies D, et al. Total circulating microparticle levels are increased in patients with deep infiltrating endometriosis. Hum Reprod. 2017;32(2):325–331.
Sikora J, Smycz-Kubańska M, Mielczarek-Palacz A, Kondera-Anasz Z. Abnormal peritoneal regulation of chemokine activa-tion—the role of IL-8 in pathogenesis of endometriosis. Am J Reprod Immunol. 2017;77(4). doi:10.1111/aji.12622.
Vannuccini S, Clifton VL, Fraser IS, et al. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum Reprod Update. 2016;22(1):104–115.
Tanaka Y, Mori T, Ito F, et al. Exacerbation of endometriosis due to regulatory T cell dysfunction. J Clin Endocrinol Metab. 2017;102(9):3206–3217.
Exacoustos C, Luciano D, Corbett B, et al. The uterine junctional zone: a 3-dimensional ultrasound study of patients with endome-triosis. Am J Obstet Gynecol. 2013;209(3):248.e1-7.
Benagiano G, Brosens I, Habiba M. Structural and molecular features of the endomyometrium in endometriosis and adenomyo-sis. Hum Reprod Update. 2014;20(3):386–402.
Roux P, Perrin J, Mancini J, Agostini A, Boubli L, Courbiere B. Factors associated with a poor prognosis for the IVF-ICSI live birth rate in women with rAFS stage III and IV endometriosis. J Assist Reprod Genet. 2017;34(7):921–928.
Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67(5):817–821.
Matalliotakis IM, Cakmak H, Mahutte N, Fragouli Y, Arici A, Sakkas D. Women with advanced-stage endometriosis and previous surgery respond less well to gonadotropin stimulation, but have similar IVF implantation and delivery rates compared with women with tubal factor infertility. Fertil Steril. 2007;88(6):1568–1572.
Marianowski P, Dąbrowski FA, Zygula A, Wielgoś M, Szymusik I. Do we pay enough attention to culture conditions in context of perinatal outcome after in vitro fertilization? Up-to-date literature review. Bio Med Res Int. 2016;2016:3285179.
Wennberg AL, Opdahl S, Bergh C, et al. Effect of maternal age on maternal and neonatal outcomes after assisted reproductive technology. Fertil Steril. 2016;106(5):1142–1149.e14.
Pinborg A, Wennerholm UB, Romundstad LB, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19(2):87–104.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-López, F.R., Villagrasa-Boli, P., Muñoz-Olarte, M. et al. Association Between Endometriosis and Preterm Birth in Women With Spontaneous Conception or Using Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of Cohort Studies. Reprod. Sci. 25, 311–319 (2018). https://doi.org/10.1177/1933719117749760
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719117749760