Unveiling the Pharmacological and Nanotechnological Facets of Daidzein: Present State-of-the-Art and Future Perspectives
Abstract
:1. Introduction
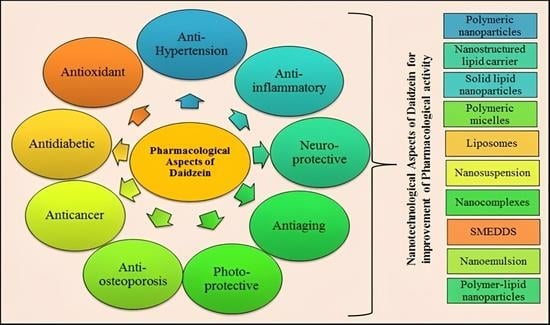
2. Physicochemical Properties and Pharmacokinetics Profile of Daidzein
3. Mechanism of Action and Pharmacological Applications of Daidzein
3.1. Anticancer Activity
3.2. Cardiovascular Diseases
3.3. Anti-Osteoporosis Activity
3.4. Antidiabetic Activity
3.5. Antioxidant Activity
3.6. Anti-Inflammatory Activity
3.7. Neuroprotective Activity
4. Outline of Nanotechnological Aspects Explored for Daidzein in Therapeutics
4.1. Polymeric Nanoparticles
4.2. Solid Lipid Nanoparticles
4.3. Nanostructured Lipid Carriers
4.4. Polymeric Micelles
4.5. Nanosuspension
4.6. Nanoemulsion
4.7. Liposomes
4.8. Self-Micro Emulsifying Drug Delivery System (SMEDDS)
5. Clinical Status of Daidzein
6. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Karunamoorthi, K.; Jegajeevanram, K.; Vijayalakshmi, J.; Mengistie, E. Traditional medicinal plants: A source of phytotherapeutic modality in resource-constrained health care settings. J. Evid. Based. Complement. Altern. Med. 2013, 18, 67–74. [Google Scholar] [CrossRef]
- Verma, S.; Singh, S.P. Current and future status of herbal medicines. Vet. World 2008, 1, 347. [Google Scholar] [CrossRef]
- Foghis, M.; Bungau, S.G.; Bungau, A.F.; Vesa, C.M.; Purza, A.L.; Tarce, A.G.; Tit, D.M.; Pallag, A.; Behl, T.; Hassan, S.S.U.; et al. Plants-based medicine implication in the evolution of chronic liver diseases. Biomed. Pharmacother. 2023, 158, 114207. [Google Scholar] [CrossRef]
- Patle, D.; Vyas, M.; Khatik, G.L. A review on natural products and herbs used in the management of diabetes. Curr. Diabetes Rev. 2021, 17, 186–197. [Google Scholar] [PubMed]
- Gitea, M.A.; Bungau, S.G.; Gitea, D.; Pasca, B.M.; Purza, A.L.; Radu, A.-F. Evaluation of the Phytochemistry–Therapeutic Activity Relationship for Grape Seeds Oil. Life 2023, 13, 178. [Google Scholar] [CrossRef] [PubMed]
- Vijayalakshmi, R.; Ravindhran, R. Preliminary comparative phytochemical screening of root extracts of Diospyrus ferrea (Wild.) Bakh and Aerva lanata (L.) Juss. Ex Schultes. Asian J. Plant Sci. Res. 2011, 2, 581–587. [Google Scholar]
- Nandagoapalan, V.; Doss, A.; Marimuthu, C. Phytochemical analysis of some traditional medicinal plants. Biosci. Discov. 2016, 7, 17–20. [Google Scholar]
- Yadav, M.; Chatterji, S.; Gupta, S.K.; Watal, G. Preliminary phytochemical screening of six medicinal plants used in traditional medicine. Int. J. Pharm. Pharm. Sci. 2014, 6, 539–542. [Google Scholar]
- Pal, D.; Verma, P. Flavonoids: A powerful and abundant source of antioxidants. Int. J. Pharm. Pharm. Sci. 2013, 5, 95–98. [Google Scholar]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, e47. [Google Scholar] [CrossRef] [PubMed]
- Ku, Y.-S.; Ng, M.-S.; Cheng, S.-S.; Lo, A.W.-Y.; Xiao, Z.; Shin, T.-S.; Chung, G.; Lam, H.-M. Understanding the composition, biosynthesis, accumulation and transport of flavonoids in crops for the promotion of crops as healthy sources of flavonoids for human consumption. Nutrients 2020, 12, 1717. [Google Scholar] [CrossRef] [PubMed]
- Górniak, I.; Bartoszewski, R.; Króliczewski, J. Comprehensive review of antimicrobial activities of plant flavonoids. Phytochem. Rev. 2019, 18, 241–272. [Google Scholar] [CrossRef]
- Sivasankarapillai, V.S.; Nair, R.M.K.; Rahdar, A.; Bungau, S.; Zaha, D.C.; Aleya, L.; Tit, D.M. Overview of the anticancer activity of withaferin A, an active constituent of the Indian ginseng Withania somnifera. Environ. Sci. Pollut. Res. Int. 2020, 27, 26025–26035. [Google Scholar] [CrossRef] [PubMed]
- Khuntia, A.; Martorell, M.; Ilango, K.; Bungau, S.G.; Radu, A.-F.; Behl, T.; Sharifi-Rad, J. Theoretical evaluation of Cleome species’ bioactive compounds and therapeutic potential: A literature review. Biomed. Pharmacother. 2022, 151, 113161. [Google Scholar] [CrossRef]
- Bellavia, D.; Dimarco, E.; Costa, V.; Carina, V.; De Luca, A.; Raimondi, L.; Fini, M.; Gentile, C.; Caradonna, F.; Giavaresi, G. Flavonoids in bone erosive diseases: Perspectives in osteoporosis treatment. Trends Endocrinol. Metab. 2021, 32, 76–94. [Google Scholar] [CrossRef] [PubMed]
- Caro-Ordieres, T.; Marín-Royo, G.; Opazo-Ríos, L.; Jiménez-Castilla, L.; Moreno, J.A.; Gómez-Guerrero, C.; Egido, J. The coming age of flavonoids in the treatment of diabetic complications. J. Clin. Med. 2020, 9, 346. [Google Scholar] [CrossRef]
- Bungau, S.; Vesa, C.M.; Abid, A.; Behl, T.; Tit, D.M.; Purza, A.L.; Pasca, B.; Todan, L.M.; Endres, L. Withaferin A—A Promising Phytochemical Compound with Multiple Results in Dermatological Diseases. Molecules 2021, 26, 2407. [Google Scholar] [CrossRef] [PubMed]
- Behl, T.; Bungau, S.; Kumar, K.; Zengin, G.; Khan, F.; Kumar, A.; Kaur, R.; Venkatachalam, T.; Tit, D.M.; Vesa, C.M.; et al. Pleotropic Effects of Polyphenols in Cardiovascular System. Biomed. Pharmacother. 2020, 130, 110714. [Google Scholar] [CrossRef]
- Domaszewska-Szostek, A.; Puzianowska-Kuźnicka, M.; Kuryłowicz, A. Flavonoids in skin senescence prevention and treatment. Int. J. Mol. Sci. 2021, 22, 6814. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, C.; Frankenfeld, C.L.; Lampe, J.W. Gut bacterial metabolism of the soy isoflavone daidzein: Exploring the relevance to human health. Exp. Biol. Med. 2005, 230, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.-Y.; Ye, Y.; Xiao, L.; Rahman, K.; Xia, W.; Zhang, H. Daidzein: A review of pharmacological effects. Afr. J. Tradit. Complement. Altern. Med. 2016, 13, 117–132. [Google Scholar] [CrossRef]
- Alshehri, M.M.; Sharifi-Rad, J.; Herrera-Bravo, J.; Jara, E.L.; Salazar, L.A.; Kregiel, D.; Uprety, Y.; Akram, M.; Iqbal, M.; Martorell, M. Therapeutic potential of isoflavones with an emphasis on daidzein. Oxid. Med. Cell. Longev. 2021, 2021, 6331630. [Google Scholar] [CrossRef] [PubMed]
- Nan, G.; Shi, J.; Huang, Y.; Sun, J.; Lv, J.; Yang, G.; Li, Y. Dissociation constants and solubilities of daidzein and genistein in different solvents. J. Chem. Eng. Data 2014, 59, 1304–1311. [Google Scholar] [CrossRef]
- Huang, Z.-R.; Hung, C.-F.; Lin, Y.-K.; Fang, J.-Y. In vitro and in vivo evaluation of topical delivery and potential dermal use of soy isoflavones genistein and daidzein. Int. J. Pharm. 2008, 364, 36–44. [Google Scholar] [CrossRef]
- Qiu, F.; Chen, X.; Song, B.; Zhong, D.; Liu, C. Influence of dosage forms on pharmacokinetics of daidzein and its main metabolite daidzein-7-O-glucuronide in rats. Acta Pharmacol. Sin. 2005, 26, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Zhao, X.; Li, J.; Shen, Q. The comparison of different daidzein-PLGA nanoparticles in increasing its oral bioavailability. Int. J. Nanomed. 2012, 7, 559. [Google Scholar]
- Kaplan, A.B.U.; Öztürk, N.; Çetin, M.; Vural, I.; Özer, T.Ö. The nanosuspension formulations of daidzein: Preparation and in vitro characterization. Turk. J. Pharm. Sci. 2022, 19, 84. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, Y.; Chadha, K.; Chadha, R.; Karan, M. Daidzein cocrystals: An opportunity to improve its biopharmaceutical parameters. Heliyon 2019, 5, e02669. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Huang, Y.; Gao, F.; Bu, H.; Gu, W.; Li, Y. Daidzein–phospholipid complex loaded lipid nanocarriers improved oral absorption: In vitro characteristics and in vivo behavior in rats. Nanoscale 2011, 3, 1780–1787. [Google Scholar] [CrossRef] [PubMed]
- Sirotkin, A.V.; Alwasel, S.H.; Harrath, A.H. The influence of plant isoflavones daidzein and equol on female reproductive processes. Pharmaceuticals 2021, 14, 373. [Google Scholar] [CrossRef] [PubMed]
- Kwiecień, A.; Ruda-Kucerova, J.; Kamiński, K.; Babinska, Z.; Popiołek, I.; Szczubiałka, K.; Nowakowska, M.; Walczak, M. Improved pharmacokinetics and tissue uptake of complexed daidzein in rats. Pharmaceutics 2020, 12, 162. [Google Scholar] [CrossRef] [PubMed]
- Amawi, H.; Ashby, C.R.; Tiwari, A.K. Cancer chemoprevention through dietary flavonoids: What’s limiting? Chin. J. Cancer 2017, 36, 50. [Google Scholar] [CrossRef]
- Rafii, F. The role of colonic bacteria in the metabolism of the natural isoflavone daidzin to equol. Metabolites 2015, 5, 56–73. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Choue, R. Plasma pharmacokinetics and urinary excretion of isoflavones after ingestion of soy products with different aglycone/glucoside ratios in South Korean women. Nutr. Res. Pract. 2013, 7, 393–399. [Google Scholar] [CrossRef]
- Ahmed, T.; Javed, S.; Tariq, A.; Onofrio, G.; Daglia, M.; Nabavi, S.F.; Nabavi, S.M. Daidzein and its effects on brain. Curr. Med. Chem. 2017, 24, 365–375. [Google Scholar]
- Xiao, B.-X.; Feng, L.; Cao, F.-R.; Pan, R.-L.; Liao, Y.-H.; Liu, X.-M.; Chang, Q. Pharmacokinetic profiles of the five isoflavonoids from Pueraria lobata roots in the CSF and plasma of rats. J. Ethnopharmacol. 2016, 184, 22–29. [Google Scholar] [CrossRef]
- Laddha, A.P.; Murugesan, S.; Kulkarni, Y.A. In-vivo and in-silico toxicity studies of daidzein: An isoflavone from soy. Drug Chem. Toxicol. 2022, 45, 1408–1416. [Google Scholar] [CrossRef]
- Sarasquete, C.; Úbeda-Manzanaro, M.; Ortiz-Delgado, J.B. Toxicity and non-harmful effects of the soya isoflavones, genistein and daidzein, in embryos of the zebrafish, Danio rerio. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2018, 211, 57–67. [Google Scholar] [CrossRef]
- Foti, P.; Erba, D.; Spadafranca, A.; Ciappellano, S.; Bresciani, J.; Testolin, G. Daidzein is absorbed by passive transport in isolated small intestine of rats. Nutr. Res. 2006, 26, 284–288. [Google Scholar] [CrossRef]
- Setchell, K.D.R.; Zhao, X.; Shoaf, S.E.; Ragland, K. The pharmacokinetics of S-(-) equol administered as SE5-OH tablets to healthy postmenopausal women. J. Nutr. 2009, 139, 2037–2043. [Google Scholar] [CrossRef] [PubMed]
- Setchell, K.D.R.; Clerici, C. Equol: Pharmacokinetics and biological actions. J. Nutr. 2010, 140, 1363S–1368S. [Google Scholar] [CrossRef]
- Chu, H.; Li, J.; Liu, T.; Miao, N.; Zhang, W. Anticancer effects of Daidzein against the human melanoma cell lines involves cell cycle arrest, autophagy and deactivation of PI3K/AKT signalling pathways. J. BUON Off. J. Balk. Union Oncol. 2021, 26, 290. [Google Scholar]
- Yu, Z.; Yang, L.; Deng, S.; Liang, M. Daidzein ameliorates LPS-induced hepatocyte injury by inhibiting inflammation and oxidative stress. Eur. J. Pharmacol. 2020, 885, 173399. [Google Scholar] [CrossRef]
- Inoue, Y.; Yoshida, M.; Ezawa, T.; Tanikawa, T.; Arce, F.; See, G.L.; Tomita, J.; Suzuki, M.; Oguchi, T. Inclusion Complexes of Daidzein with Cyclodextrin-Based Metal–Organic Framework-1 Enhance Its Solubility and Antioxidant Capacity. AAPS PharmSciTech 2022, 23, 2. [Google Scholar] [CrossRef]
- Laddha, A.P.; Kulkarni, Y.A. Daidzein ameliorates diabetic retinopathy in experimental animals. Life Sci. 2021, 265, 118779. [Google Scholar] [CrossRef] [PubMed]
- Herwana, E.; Pusparini, P.; Graciela, A. High dietary daidzein intake lowers cholesterol levels among post-menopausal women. Universa Med. 2020, 39, 47–54. [Google Scholar] [CrossRef]
- Laddha, A.P.; Kulkarni, Y.A. Daidzein mitigates myocardial injury in streptozotocin-induced diabetes in rats. Life Sci. 2021, 284, 119664. [Google Scholar] [CrossRef]
- Li, Y.; Li, Z.; Liu, S.; Su, Y.; Li, Y. Cardiotonic Activity of Daidzein Against Doxorubicin-lnduced Congestive Cardiac Failure in Rats. Curr. Top. Nutraceutical Res. 2022, 20, 106–113. [Google Scholar]
- Rawat, S.; Pathak, S.; Gupta, G.; Singh, S.K.; Singh, H.; Mishra, A.; Gilhotra, R. Recent updates on daidzein against oxidative stress and cancer. EXCLI J. 2019, 18, 950. [Google Scholar]
- Amaral, C.; Toloi, M.R.T.; Vasconcelos, L.D.; Fonseca, M.J.V.; Correia-da-Silva, G.; Teixeira, N. The role of soybean extracts and isoflavones in hormone-dependent breast cancer: Aromatase activity and biological effects. Food Funct. 2017, 8, 3064–3074. [Google Scholar] [CrossRef]
- Meng, H.; Fu, G.; Shen, J.; Shen, K.; Xu, Z.; Wang, Y.; Jin, B.; Pan, H. Ameliorative effect of daidzein on cisplatin-induced nephrotoxicity in mice via modulation of inflammation, oxidative stress, and cell death. Oxid. Med. Cell. Longev. 2017, 2017, 3140680. [Google Scholar] [CrossRef]
- Magee, P.J.; Allsopp, P.; Samaletdin, A.; Rowland, I.R. Daidzein, R-(+) equol and S-(−) equol inhibit the invasion of MDA-MB-231 breast cancer cells potentially via the down-regulation of matrix metalloproteinase-2. Eur. J. Nutr. 2014, 53, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Shu, F.; Zeng, Y.; Meng, X.; Wang, B.; Diao, L.; Wang, L.; Wan, J.; Zhu, J.; Wang, J. Daidzein supplementation decreases serum triglyceride and uric acid concentrations in hypercholesterolemic adults with the effect on triglycerides being greater in those with the GA compared with the GG genotype of ESR-β Rsa I. J. Nutr. 2014, 144, 49–54. [Google Scholar] [CrossRef]
- Sun, J.; Sun, W.J.; Li, Z.Y.; Li, L.; Wang, Y.; Zhao, Y.; Wang, C.; Yu, L.R.; Li, L.Z.; Zhang, Y.L. Daidzein increases OPG/RANKL ratio and suppresses IL-6 in MG-63 osteoblast cells. Int. Immunopharmacol. 2016, 40, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Bitto, A. Oxidative stress: Harms and benefits for human health. Oxidative Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Q.U.; Ali, A.H.M.; Mukhtar, S.; Alsharif, M.A.; Parveen, H.; Sabere, A.S.M.; Nawi, M.S.M.; Khatib, A.; Siddiqui, M.J.; Umar, A. Medicinal potential of isoflavonoids: Polyphenols that may cure diabetes. Molecules 2020, 25, 5491. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.E.; Lee, K.W.; Byun, S.; Jung, S.K.; Song, N.; Lim, S.H.; Heo, Y.-S.; Kim, J.E.; Kang, N.J.; Kim, B.Y. 7,3′,4′-Trihydroxyisoflavone, a metabolite of the soy isoflavone daidzein, suppresses ultraviolet B-induced skin cancer by targeting Cot and MKK4. J. Biol. Chem. 2011, 286, 14246–14256. [Google Scholar] [CrossRef]
- Velentzis, L.S.; Woodside, J.V.; Cantwell, M.M.; Leathem, A.J.; Keshtgar, M.R. Do phytoestrogens reduce the risk of breast cancer and breast cancer recurrence? What clinicians need to know. Eur. J. Cancer 2008, 44, 1799–1806. [Google Scholar] [CrossRef]
- Liu, M.M.; Huang, Y.; Wang, J. Developing phytoestrogens for breast cancer prevention. Anti-Cancer Agents Med. Chem. (Former. Curr. Med. Chem. Agents) 2012, 12, 1306–1313. [Google Scholar] [CrossRef]
- Abotaleb, M.; Samuel, S.M.; Varghese, E.; Varghese, S.; Kubatka, P.; Liskova, A.; Büsselberg, D. Flavonoids in cancer and apoptosis. Cancers 2018, 11, 28. [Google Scholar] [CrossRef]
- Bao, C.; Namgung, H.; Lee, J.; Park, H.-C.; Ko, J.; Moon, H.; Ko, H.W.; Lee, H.J. Daidzein suppresses tumor necrosis factor-α induced migration and invasion by inhibiting hedgehog/Gli1 signaling in human breast cancer cells. J. Agric. Food Chem. 2014, 62, 3759–3767. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Agarwal, R. Natural flavonoids targeting deregulated cell cycle progression in cancer cells. Curr. Drug Targets 2006, 7, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.J.; Kim, G.-H. Daidzein causes cell cycle arrest at the G1 and G2/M phases in human breast cancer MCF-7 and MDA-MB-453 cells. Phytomedicine 2008, 15, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Xu, H.; Hu, X.; Ma, W.; Zhang, J.; Li, Y.; Yu, M.; Zhang, Y.; Li, X.; Ye, X. Synergetic inhibition of daidzein and regular exercise on breast cancer in bearing-4T1 mice by regulating NK cells and apoptosis pathway. Life Sci. 2020, 245, 117387. [Google Scholar] [CrossRef] [PubMed]
- Rabiau, N.; Kossaï, M.; Braud, M.; Chalabi, N.; Satih, S.; Bignon, Y.-J.; Bernard-Gallon, D.J. Genistein and daidzein act on a panel of genes implicated in cell cycle and angiogenesis by polymerase chain reaction arrays in human prostate cancer cell lines. Cancer Epidemiol. 2010, 34, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.M.; Xiao, B.X.; Liu, D.H.; Grant, M.; Zhang, S.; Lai, Y.F.; Guo, Y.B.; Liu, Q. Biphasic effect of daidzein on cell growth of human colon cancer cells. Food Chem. Toxicol. 2004, 42, 1641–1646. [Google Scholar] [CrossRef]
- Gheorghe, G.; Toth, P.P.; Bungau, S.; Behl, T.; Ilie, M.; Stoian, A.P.; Bratu, O.G.; Bacalbasa, N.; Rus, M.; Diaconu, C.C. Cardiovascular Risk and Statin Therapy Considerations in Women. Diagnostics 2020, 10, 483. [Google Scholar] [CrossRef] [PubMed]
- Reckelhoff, J.F. Sex steroids, cardiovascular disease, and hypertension: Unanswered questions and some speculations. Hypertension 2005, 45, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.L.; Serock, M.R.; Khalil, R.A. Experimental benefits of sex hormones on vascular function and the outcome of hormone therapy in cardiovascular disease. Curr. Cardiol. Rev. 2008, 4, 309–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, H.; Guo, W.; Han, J.; Li, X.-A. Role of caveolin-1 and caveolae signaling in endotoxemia and sepsis. Life Sci. 2013, 93, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Maxfield, F.R.; van Meer, G. Cholesterol, the central lipid of mammalian cells. Curr. Opin. Cell Biol. 2010, 22, 422–429. [Google Scholar] [CrossRef]
- Sandhu, S.K.; Hampson, G. The pathogenesis, diagnosis, investigation and management of osteoporosis. J. Clin. Pathol. 2011, 64, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Tit, D.M.; Bungau, S.; Iovan, C.; Cseppento, D.C.N.; Endres, L.; Sava, C.; Sabau, A.M.; Furau, G.; Furau, C. Effects of the Hormone Replacement Therapy and of Soy Isoflavones on Bone Resorption in Postmenopause. J. Clin. Med. 2018, 7, 297. [Google Scholar] [CrossRef] [PubMed]
- Kruger, M.C.; Wolber, F.M. Osteoporosis: Modern paradigms for last century’s bones. Nutrients 2016, 8, 376. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Yu, B.; Tang, D.; Li, S.; Wu, Y. Daidzein promotes osteoblast proliferation and differentiation in OCT1 cells through stimulating the activation of BMP-2/Smads pathway. Genet. Mol. Res. 2016, 15, gmr.15028792. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Sugimoto, E. Stimulatory effect of genistein and daidzein on protein synthesis in osteoblastic MC3T3-E1 cells: Activation of aminoacyl-tRNA synthetase. Mol. Cell. Biochem. 2000, 214, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Kaveeshwar, S.A.; Cornwall, J. The current state of diabetes mellitus in India. Australas. Med. J. 2014, 7, 45. [Google Scholar] [CrossRef] [PubMed]
- Iorga, R.A.; Bacalbasa, N.; Carsote, M.; Bratu, O.G.; Stanescu, A.M.A.; Bungau, S.; Pantis, C.; Diaconu, C.C. Metabolic and cardiovascular benefits of GLP-1 agonists, besides the hypoglycemic effect (Review). Exp. Ther. Med. 2020, 20, 2396–2400. [Google Scholar] [CrossRef] [PubMed]
- Das, D.; Sarkar, S.; Bordoloi, J.; Wann, S.B.; Kalita, J.; Manna, P. Daidzein, its effects on impaired glucose and lipid metabolism and vascular inflammation associated with type 2 diabetes. Biofactors 2018, 44, 407–417. [Google Scholar] [CrossRef]
- Tian, D.; Liu, J.; Liu, N.; Wang, R.; Ai, Y.; Jin, L.; Li, F.; Wei, P.; Li, Z.; Wang, C. Daidzin decreases blood glucose and lipid in streptozotocin-induced diabetic mice. Trop. J. Pharm. Res. 2016, 15, 2435–2443. [Google Scholar] [CrossRef]
- Liang, J.; Tian, Y.-X.; Fu, L.-M.; Wang, T.-H.; Li, H.-J.; Wang, P.; Han, R.-M.; Zhang, J.-P.; Skibsted, L.H. Daidzein as an antioxidant of lipid: Effects of the microenvironment in relation to chemical structure. J. Agric. Food Chem. 2008, 56, 10376–10383. [Google Scholar] [CrossRef] [PubMed]
- Kampkötter, A.; Chovolou, Y.; Kulawik, A.; Röhrdanz, E.; Weber, N.; Proksch, P.; Wätjen, W. Isoflavone daidzein possesses no antioxidant activities in cell-free assays but induces the antioxidant enzyme catalase. Nutr. Res. 2008, 28, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Toda, S.; Shirataki, Y. Comparison of antioxidative and chelating effects of daidzein and daidzin on protein oxidative modification by copper in vitro. Biol. Trace Elem. Res. 2001, 79, 83–89. [Google Scholar] [CrossRef]
- Barton, G.M. A calculated response: Control of inflammation by the innate immune system. J. Clin. Investig. 2008, 118, 413–420. [Google Scholar] [CrossRef]
- Yu, J.; Bi, X.; Yu, B.; Chen, D. Isoflavones: Anti-inflammatory benefit and possible caveats. Nutrients 2016, 8, 361. [Google Scholar] [CrossRef]
- Zhang, H.; Kovacs-Nolan, J.; Kodera, T.; Eto, Y.; Mine, Y. γ-Glutamyl cysteine and γ-glutamyl valine inhibit TNF-α signaling in intestinal epithelial cells and reduce inflammation in a mouse model of colitis via allosteric activation of the calcium-sensing receptor. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2015, 1852, 792–804. [Google Scholar] [CrossRef]
- Birben, E.; Sahiner, U.M.; Sackesen, C.; Erzurum, S.; Kalayci, O. Oxidative stress and antioxidant defense. World Allergy Organ. J. 2012, 5, 9–19. [Google Scholar] [CrossRef]
- Choi, E.J.; Kim, G. The antioxidant activity of daidzein metabolites, O-desmethylangolensin and equol, in HepG2 cells. Mol. Med. Rep. 2014, 9, 328–332. [Google Scholar] [CrossRef]
- Sharma, V.; Nath, D.; Gautam, S.; Radu, A.-F.; Behl, T.; Bungau, S.G.; Vesa, C.M. Reviewing the Traditional/Modern Uses, Phytochemistry, Essential Oils/Extracts and Pharmacology of Embelia ribes Burm. Antioxidants 2022, 11, 1359. [Google Scholar] [CrossRef]
- Cheatwood, J.L.; Emerick, A.J.; Kartje, G.L. Neuronal plasticity and functional recovery after ischemic stroke. Top. Stroke Rehabil. 2008, 15, 42–50. [Google Scholar] [CrossRef]
- Stout, J.M.; Knapp, A.N.; Banz, W.J.; Wallace, D.G.; Cheatwood, J.L. Subcutaneous daidzein administration enhances recovery of skilled ladder rung walking performance following stroke in rats. Behav. Brain Res. 2013, 256, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Hurtado, O.; Ballesteros, I.; Cuartero, M.I.; Moraga, A.; Pradillo, J.M.; Ramírez-Franco, J.; Bartolomé-Martín, D.; Pascual, D.; Torres, M.; Sánchez-Prieto, J. Daidzein has neuroprotective effects through ligand-binding-independent PPARγ activation. Neurochem. Int. 2012, 61, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Bordet, R.; Gelé, P.; Duriez, P.; Fruchart, J.C. PPARs: A new target for neuroprotection. J. Neurol. Neurosurg. Psychiatry 2006, 77, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Tai, F.; Zeng, S.; Zhang, X. Effects of perinatal daidzein exposure on subsequent behavior and central estrogen receptor α expression in the adult male mouse. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 43, 157–167. [Google Scholar] [CrossRef]
- Atiq, A.; Shal, B.; Naveed, M.; Khan, A.; Ali, J.; Zeeshan, S.; Al-Sharari, S.D.; Kim, Y.S.; Khan, S. Diadzein ameliorates 5-fluorouracil-induced intestinal mucositis by suppressing oxidative stress and inflammatory mediators in rodents. Eur. J. Pharmacol. 2019, 843, 292–306. [Google Scholar] [CrossRef]
- Kim, D.H.; Jung, H.A.; Park, S.J.; Kim, J.M.; Lee, S.; Choi, J.S.; Cheong, J.H.; Ko, K.H.; Ryu, J.H. The effects of daidzin and its aglycon, daidzein, on the scopolamineinduced memory impairment in male mice. Arch. Pharm. Res. 2010, 33, 1685–1690. [Google Scholar] [CrossRef]
- Guo, Y.; Wu, G.; Su, X.; Yang, H.; Zhang, J. Antiobesity action of a daidzein derivative on male obese mice induced by a high-fat diet. Nutr. Res. 2009, 29, 656–663. [Google Scholar] [CrossRef]
- Goel, R.; Chaudhary, R. Effect of daidzein on Parkinson disease induced by reserpine in rats. Braz. J. Pharm. Sci. 2020, 56, 1–7. [Google Scholar] [CrossRef]
- Woodman, O.L.; Boujaoude, M. Chronic treatment of male rats with daidzein and 17β-oestradiol induces the contribution of EDHF to endothelium-dependent relaxation. Br. J. Pharmacol. 2004, 141, 322–328. [Google Scholar] [CrossRef] [Green Version]
- Ko, Y.-H.; Kim, S.Y.; Lee, S.-Y.; Jang, C.-G. 6,7,4′-Trihydroxyisoflavone, a major metabolite of daidzein, improves learning and memory via the cholinergic system and the p-CREB/BDNF signaling pathway in mice. Eur. J. Pharmacol. 2018, 826, 140–147. [Google Scholar] [CrossRef]
- Park, M.-H.; Ju, J.-W. Daidzein inhibits carbohydrate digestive enzymes in vitro and alleviates postprandial hyperglycemia in diabetic mice. Eur. J. Pharmacol. 2013, 712, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Yang, X.; Liu, J.; Li, K. Effects of daidzein sulfates on blood pressure and artery of rats. Basic Clin. Pharmacol. Toxicol. 2006, 99, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Singh, M.; Sharma, P.L. Ameliorative effect of daidzein: A caveolin-1 inhibitor in vascular endothelium dysfunction induced by ovariectomy. Indian J. Exp. Biol. 2012, 50, 28–34. [Google Scholar] [PubMed]
- Choi, E.J. The prooxidant, rather than antioxidant, acts of daidzein in vivo and in vitro: Daidzein suppresses glutathione metabolism. Eur. J. Pharmacol. 2006, 542, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Zeng, S.; Tai, F.; Zhai, P.; Yuan, A.; Jia, R.; Zhang, X. Effect of daidzein on anxiety, social behavior and spatial learning in male Balb/cJ mice. Pharmacol. Biochem. Behav. 2010, 96, 16–23. [Google Scholar] [CrossRef]
- Farhana, A.; Veeresh, B.; Rao, R. Protective Role of Diadzein in L-Arginine-Induced Acute pancreatitis in Rats. YMER Digit. 2022, 21, 451–460. [Google Scholar] [CrossRef]
- Sakamoto, Y.; Naka, A.; Ohara, N.; Kondo, K.; Iida, K. Daidzein regulates proinflammatory adipokines thereby improving obesity-related inflammation through PPARγ. Mol. Nutr. Food Res. 2014, 58, 718–726. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Xu, J.; Guo, T.L. Isoflavone daidzein regulates immune responses in the B6C3F1 and non-obese diabetic (NOD) mice. Int. Immunopharmacol. 2019, 71, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Alò, R.; Fazzari, G.; Zizza, M.; Avolio, E.; Di Vito, A.; Bruno, R.; Cuda, G.; Barni, T.; Canonaco, M.; Facciolo, R.M. Daidzein Pro-cognitive Effects Coincided with Changes of Brain Neurotensin1 Receptor and Interleukin-10 Expression Levels in Obese Hamsters. Neurotox. Res. 2021, 39, 645–657. [Google Scholar] [CrossRef] [PubMed]
- Crespillo, A.; Alonso, M.; Vida, M.; Pavón, F.J.; Serrano, A.; Rivera, P.; Romero-Zerbo, Y.; Fernández-Llebrez, P.; Martínez, A.; Pérez-Valero, V. Reduction of body weight, liver steatosis and expression of stearoyl-CoA desaturase 1 by the isoflavone daidzein in diet-induced obesity. Br. J. Pharmacol. 2011, 164, 1899–1915. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.H.; Park, J.S.; Jung, J.W.; Byun, K.W.; Kang, K.S.; Lee, Y.S. Daidzein supplementation prevents non-alcoholic fatty liver disease through alternation of hepatic gene expression profiles and adipocyte metabolism. Int. J. Obes. 2011, 35, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Mohamad-Shahi, M.; Karandish, M.; Haidari, F.; Omidian, K.; Fatemi-Tabatabayei, S.-R.; Rafiei, H. Effect of daidzein-low-calorie diet on body weight, serum levels of glucose, resistin, and high sensitive C-reactive protein in high fat, high calorie diet induced rats. Saudi. Med. J. 2012, 33, 70–75. [Google Scholar] [PubMed]
- Park, S.A.; Choi, M.-S.; Cho, S.-Y.; Seo, J.-S.; Jung, U.J.; Kim, M.-J.; Sung, M.-K.; Park, Y.B.; Lee, M.-K. Genistein and daidzein modulate hepatic glucose and lipid regulating enzyme activities in C57BL/KsJ-db/db mice. Life Sci. 2006, 79, 1207–1213. [Google Scholar] [CrossRef]
- Tomar, A.; Kaushik, S.; Khan, S.I.; Bisht, K.; Nag, T.C.; Arya, D.S.; Bhatia, J. The dietary isoflavone daidzein mitigates oxidative stress, apoptosis, and inflammation in CDDP-induced kidney injury in rats: Impact of the MAPK signaling pathway. J. Biochem. Mol. Toxicol. 2020, 34, e22431. [Google Scholar] [CrossRef] [PubMed]
- Alshamrani, M. Broad-Spectrum Theranostics and Biomedical Application of Functionalized Nanomaterials. Polymers 2022, 14, 1221. [Google Scholar] [CrossRef]
- Riehemann, K.; Schneider, S.W.; Luger, T.A.; Godin, B.; Ferrari, M.; Fuchs, H. Nanomedicine—Challenge and perspectives. Angew. Chem. Int. Ed. 2009, 48, 872–897. [Google Scholar] [CrossRef] [PubMed]
- Boulaiz, H.; Alvarez, P.J.; Ramirez, A.; Marchal, J.A.; Prados, J.; Rodríguez-Serrano, F.; Perán, M.; Melguizo, C.; Aranega, A. Nanomedicine: Application areas and development prospects. Int. J. Mol. Sci. 2011, 12, 3303–3321. [Google Scholar] [CrossRef] [PubMed]
- Pison, U.; Welte, T.; Giersig, M.; Groneberg, D.A. Nanomedicine for respiratory diseases. Eur. J. Pharmacol. 2006, 533, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Zou, T.; Gu, L. TPGS emulsified zein nanoparticles enhanced oral bioavailability of daidzin: In vitro characteristics and in vivo performance. Mol. Pharm. 2013, 10, 2062–2070. [Google Scholar] [CrossRef] [PubMed]
- Ozakar, R.S.; Cetin, M.; Taghizadehghalehjoughi, A.; Hacimuftuoglu, A. Preparation and In Vitro Evaluation of Daidzein-Loaded Nanoparticulate Systems. Eurasia Proc. Health Environ. Life Sci. 2021, 1, 1–12. [Google Scholar]
- Gao, Y.; Gu, W.; Chen, L.; Xu, Z.; Li, Y. The role of daidzein-loaded sterically stabilized solid lipid nanoparticles in therapy for cardio-cerebrovascular diseases. Biomaterials 2008, 29, 4129–4136. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Fan, X.; Shen, Q. Daidzein-loaded nanostructured lipid carriers-PLGA nanofibers for transdermal delivery. Int. J. Pharm. 2016, 501, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Wusiman, Z.; Sun, L.; Zuo, T.; Yin, Y.; Yang, X.; Shen, Q. Core–shell-type polymer–lipid nanoparticles for the transdermal delivery of daidzein. Micro Nano Lett. 2018, 13, 1363–1366. [Google Scholar] [CrossRef]
- Zhang, Z.; Huang, Y.; Gao, F.; Gao, Z.; Bu, H.; Gu, W.; Li, Y. A self-assembled nanodelivery system enhances the oral bioavailability of daidzein: In vitro characteristics and in vivo performance. Nanomedicine 2011, 6, 1365–1379. [Google Scholar] [CrossRef]
- Wang, H.; Xiao, Y.; Wang, H.; Sang, Z.; Han, X.; Ren, S.; Du, R.; Shi, X.; Xie, Y. Development of daidzein nanosuspensions: Preparation, characterization, in vitro evaluation, and pharmacokinetic analysis. Int. J. Pharm. 2019, 566, 67–76. [Google Scholar] [CrossRef]
- Lv, L.; Fu, C.; Zhang, F.; Wang, S. Thermally-induced whey protein isolate-daidzein co-assemblies: Protein-based nanocomplexes as an inhibitor of precipitation/crystallization for hydrophobic drug. Food Chem. 2019, 275, 273–281. [Google Scholar] [CrossRef]
- Kaplan, A.B.U.; Cetin, M.; Orgul, D.; Taghizadehghalehjoughi, A.; Hacımuftuoglu, A.; Hekimoglu, S. Formulation and in vitro evaluation of topical nanoemulsion and nanoemulsion-based gels containing daidzein. J. Drug Deliv. Sci. Technol. 2019, 52, 189–203. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, W.; Wang, J.; Liu, H.; Chen, Y. Preparation and pharmacokinetic study of Daidzein Long-circulating liposomes. Nanoscale Res. Lett. 2019, 14, 321. [Google Scholar] [CrossRef]
- Shen, Q.; Li, X.; Yuan, D.; Jia, W. Enhanced oral bioavailability of daidzein by self-microemulsifying drug delivery system. Chem. Pharm. Bull. 2010, 58, 639–643. [Google Scholar] [CrossRef]
- DeFrates, K.; Markiewicz, T.; Gallo, P.; Rack, A.; Weyhmiller, A.; Jarmusik, B.; Hu, X. Protein polymer-based nanoparticles: Fabrication and medical applications. Int. J. Mol. Sci. 2018, 19, 1717. [Google Scholar] [CrossRef] [Green Version]
- Zielińska, A.; Carreiró, F.; Oliveira, A.M.; Neves, A.; Pires, B.; Venkatesh, D.N.; Durazzo, A.; Lucarini, M.; Eder, P.; Silva, A.M. Polymeric nanoparticles: Production, characterization, toxicology and ecotoxicology. Molecules 2020, 25, 3731. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.M.; Valencia, P.M.; Zhang, L.; Langer, R.; Farokhzad, O.C. Polymeric nanoparticles for drug delivery. In Cancer Nanotechnology; Springer: Berlin/Heidelberg, Germany, 2010; pp. 163–175. [Google Scholar]
- Rao, J.P.; Geckeler, K.E. Polymer nanoparticles: Preparation techniques and size-control parameters. Prog. Polym. Sci. 2011, 36, 887–913. [Google Scholar] [CrossRef]
- Vauthier, C.; Bouchemal, K. Methods for the preparation and manufacture of polymeric nanoparticles. Pharm. Res. 2009, 26, 1025–1058. [Google Scholar] [CrossRef] [PubMed]
- Nagavarma, B.V.N.; Yadav, H.K.S.; Ayaz, A.; Vasudha, L.S.; Shivakumar, H.G. Different techniques for preparation of polymeric nanoparticles-a review. Asian J. Pharm. Clin. Res. 2012, 5, 16–23. [Google Scholar]
- Lingayat, V.J.; Zarekar, N.S.; Shendge, R.S. Solid lipid nanoparticles: A review. Nanosci. Nanotechnol. Res. 2017, 4, 67–72. [Google Scholar]
- Yadav, N.; Khatak, S.; Sara, U.V.S. Solid lipid nanoparticles-a review. Int. J. Appl. Pharm. 2013, 5, 8–18. [Google Scholar]
- Üner, M.; Yener, G. Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives. Int. J. Nanomed. 2007, 2, 289. [Google Scholar]
- Pizzol, C.D.; Filippin-Monteiro, F.B.; Restrepo, J.A.S.; Pittella, F.; Silva, A.H.; de Souza, P.A.; de Campos, A.M.; Creczynski-Pasa, T.B. Influence of surfactant and lipid type on the physicochemical properties and biocompatibility of solid lipid nanoparticles. Int. J. Environ. Res. Public Health 2014, 11, 8581–8596. [Google Scholar] [CrossRef]
- Duong, V.-A.; Nguyen, T.-T.-L.; Maeng, H.-J. Preparation of solid lipid nanoparticles and nanostructured lipid carriers for drug delivery and the effects of preparation parameters of solvent injection method. Molecules 2020, 25, 4781. [Google Scholar] [CrossRef]
- Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured lipid carriers for delivery of chemotherapeutics: A review. Pharmaceutics 2020, 12, 288. [Google Scholar] [CrossRef]
- Mukherjee, S.; Ray, S.; Thakur, R.S. Solid lipid nanoparticles: A modern formulation approach in drug delivery system. Indian J. Pharm. Sci. 2009, 71, 349. [Google Scholar] [CrossRef]
- Patel, D.K.; Tripathy, S.; Nair, S.K.; Kesharwani, R. Nanostructured lipid carrier (Nlc) a modern approach for topical delivery: A review. World J. Pharm. Pharm. Sci. 2013, 2, 921–938. [Google Scholar]
- Li, Q.; Cai, T.; Huang, Y.; Xia, X.; Cole, S.P.C.; Cai, Y. A review of the structure, preparation, and application of NLCs, PNPs, and PLNs. Nanomaterials 2017, 7, 122. [Google Scholar] [CrossRef] [PubMed]
- Gomaa, E.; Fathi, H.A.; Eissa, N.G.; Elsabahy, M. Methods for preparation of nanostructured lipid carriers. Methods 2022, 199, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Movassaghian, S.; Merkel, O.M.; Torchilin, V.P. Applications of polymer micelles for imaging and drug delivery. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2015, 7, 691–707. [Google Scholar] [CrossRef]
- Nishiyama, N.; Kataoka, K. Current state, achievements, and future prospects of polymeric micelles as nanocarriers for drug and gene delivery. Pharmacol. Ther. 2006, 112, 630–648. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.R.; Agrawal, Y.K. Nanosuspension: An approach to enhance solubility of drugs. J. Adv. Pharm. Technol. Res. 2011, 2, 81. [Google Scholar]
- Krishna, K.B.; Prabhakar, C. A review on nanosuspensions in drug delivery. Int. J. Pharma. Bio Sci. 2011, 2, 549–558. [Google Scholar]
- Lakshmi, P.; Kumar, G.A. Nanosuspension technology: A review. Int. J. Pharm. Pharm. Sci. 2010, 2, 35–40. [Google Scholar]
- Patravale, V.B.; Date, A.A.; Kulkarni, R.M. Nanosuspensions: A promising drug delivery strategy. J. Pharm. Pharmacol. 2004, 56, 827–840. [Google Scholar] [CrossRef]
- Patel, M.; Shah, A.; Patel, N.M.; Patel, M.R.; Patel, K.R. Nanosuspension: A novel approach for drug delivery system. Jpsbr 2011, 1, 1–10. [Google Scholar]
- Patel, R.P.; Joshi, J.R. An overview on nanoemulsion: A novel approach. Int. J. Pharm. Sci. Res. 2012, 3, 4640. [Google Scholar]
- Nikam, T.H.; Patil, M.P.; Patil, S.S.; Vadnere, G.P.; Lodhi, S. Nanoemulsion: A brief review on development and application in Parenteral Drug Delivery. Adv. Pharm. J. 2018, 3, 43–54. [Google Scholar] [CrossRef]
- Jaiswal, M.; Dudhe, R.; Sharma, P.K. Nanoemulsion: An advanced mode of drug delivery system. 3 Biotech 2015, 5, 123–127. [Google Scholar] [CrossRef]
- Sharma, N.; Bansal, M.; Visht, S.; Sharma, P.K.; Kulkarni, G.T. Nanoemulsion: A new concept of delivery system. Chron. Young Sci. 2010, 1, 2–6. [Google Scholar]
- Bozzuto, G.; Molinari, A. Liposomes as nanomedical devices. Int. J. Nanomed. 2015, 10, 975. [Google Scholar] [CrossRef]
- Maherani, B.; Arab-Tehrany, E.; Mozafari, M.R.; Gaiani, C.; Linder, M. Liposomes: A review of manufacturing techniques and targeting strategies. Curr. Nanosci. 2011, 7, 436–452. [Google Scholar] [CrossRef]
- Salimi, A. Liposomes as a novel drug delivery system: Fundamental and pharmaceutical application. Asian J. Pharm. 2018, 12, S31–S41. [Google Scholar]
- Gbian, D.L.; Omri, A. Current and novel therapeutic strategies for the management of cystic fibrosis. Expert Opin. Drug Deliv. 2021, 18, 535–552. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef]
- Kyatanwar, A.U.; Jadhav, K.R.; Kadam, V.J. Self micro-emulsifying drug delivery system (SMEDDS). J. Pharm. Res. 2010, 3, 75–83. [Google Scholar]
- Patel, D.; Sawant, K.K. Self micro-emulsifying drug delivery system: Formulation development and biopharmaceutical evaluation of lipophilic drugs. Curr. Drug Deliv. 2009, 6, 419–424. [Google Scholar] [CrossRef]
- Gurram, A.K.; Deshpande, P.B.; Kar, S.S.; Nayak, U.Y.; Udupa, N.; Reddy, M.S. Role of components in the formation of self-microemulsifying drug delivery systems. Indian J. Pharm. Sci. 2015, 77, 249. [Google Scholar] [PubMed] [Green Version]
- Clinical Trials Assessing the Medical Role of Daidzein. U.S. National Library of Medicine. Available online: https://clinicaltrials.gov/ (accessed on 12 December 2022).



| Profile | Description |
|---|---|
| Physicochemical characteristics | |
| Source | In Soy products |
| Empirical Formula | C15H10O4 |
| Molecular Weight | 254.54 g/mol |
| Solubility | Sparingly soluble in aqueous buffers; soluble in organic solvents like ethanol, dimethyl sulfoxide and dimethyl formamide. |
| Partition coefficient | 2.55 |
| Physical appearance | Pale yellow prisms |
| Melting point | 315 ± 5 °C |
| ƛmax (Lambda maximum) | 250 nm |
| Pharmacokinetics | |
| Absorption | Research showed that DAI exhibits passive, unsaturable transport absorption mechanism predominantly from distal part of small intestine of rats in comparison to proximal and medial parts. This was found that total DAI intestinal absorption was approximately 6% in 60 min [39] |
| Distribution | Volume of distribution: 336.25 L; Clearance rate: 30.09 L/h [37,38] |
| Metabolism | DAI is converted by the body to its aglycone form (without the glucose side chain) [40]; the main metabolite of DAI was found daidzein-7-O-glucuronide [25] |
| Excretion | Approximately, between 30 and 40 percent of DAI is excreted in urine [41] |
| Route | Disease | Dose/Duration | Outcomes | Animal Model | Ref. |
|---|---|---|---|---|---|
| i.p. | Oxidative stress | 200 mg/kg for 2 days | Effective in reducing glutathione reserve, glutathione peroxidase activity and superoxide dismutase’s activity | Mice | [51] |
| i.p. | Inflammation | 1, 5, 10 mg/kg once a day for 7 days | DAI produced significant anti mucosity activity at 10 mg/kg against 5-Fluorouracil induced mucositis | Mice | [95] |
| p.o. | Memory impairment | 5 mg/kg | Administration of DAI acts on estrogen receptor to improve the memory loss condition | Mice | [96] |
| p.o. | Obesity | 50 and 100 mg/kg for 30 consecutive days | Reduced the body and white adipose tissue weight of obese mice and ameliorated the hyperlipoidemia induced by high fat diet | Mice | [97] |
| p.o. | Parkinson | 50, 100 mg/kg per day for 5 days | Significant improvement in neuronal degeneration in brain tissue | Rats | [98] |
| s.c. | Cardiovascular | 200 mg/day for 7 days | Effective in enhancement of endothelial dependent relaxation | Rats | [99] |
| p.o. | Memory impairment | 5 kg/mg | Improvement in the dysfunction due to scopolamine and enhanced learning capacity as compared to control group | Mice | [100] |
| p.o. | Diabetes | 10 mg/kg | Potential antidiabetic activity showed via inhibitory effect on α-glucosidase and α-amylase | Mice | [101] |
| p.o. | Blood pressure | 20 mg/kg for 2 weeks daily | Induced hypotensive and vasodilator effects by inhibiting Ca2+ influx | Rats | [102] |
| s.c. | Ovariectomy | 0.2, 0.4 and 0.8 mg/kg per day for 1 week | Improved vascular endothelial dysfunction by inhibiting caveolin-1 and activation of PI3K-PKB/Akt pathway | Rats | [103] |
| p.o. | Diabetic retinopathy | 25, 50, 100 mg/kg for 28 days | Prevented from the damage of retina in hyperglycemia condition by reducing oxidative stress | Rats | [45] |
| p.o. | Neuroprotective | 2 or 20 mg/day for 4 weeks | DAI significantly decreased the concentration of malondialdehyde and act as pro-oxidant | Rats | [104] |
| p.o. | Anxiety | 200 mg/kg | Long-term DAI ingestion produced considerable impact on social behavior, mood, and locomotion | Mice | [105] |
| i.p. | Inflammation | 10 mg/kg/day | Significantly reduced the severity of L-arginine-induced acute pancreatitis while the anti-inflammatory and strong antioxidative properties are responsible for improvement | Rats | [106] |
| p.o. | Inflammation | 1.0 g/kg chow for 12 weeks | Effective in decreasing MCP-1, TNF-α, and increased expression of adiponectin | Mice | [107] |
| p.o. | Immunomodulation | 20 mg/kg biweekly | Significantly reduced IgG1 production, while increased the T-helper cells | Mice | [108] |
| p.o. | Neuroprotective | 200 mg/kg for 15 days | Study showed neuroprotective effect when interacted with the receptor neurotensin1 and interleukin-10 pathways | Rats | [109] |
| i.p. | Obesity | 50 mg/kg for 14 days | Significantly reduced body weight in rats and, as well, ameliorate the condition of hyperlipidemia, which can partially explain the anti-steatotic, cholesterol-lowering and insulin sensitizing effects | Rats | [110] |
| p.o. | Fatty liver | 0.1 g per kg diet for 12 weeks | Effective in inhibiting the adiposity by the upregulation of genes involved in fatty acid β-oxidation and the anti-adipogenesis | Mice | [111] |
| p.o. | Diabetes | 50 mg/kg for 4 weeks | Demonstrated that it is effective in decreasing blood glucose level and no effect on resistin level | Rats | [112] |
| p.o. | Diabetes | 0.2 g/kg for 6 weeks | Effectively act as anti-hyperglycemic through the activation of glucokinase and inhibition of G6Pase, PEPCK, FAS, β-oxidation, and CPT in the liver | Mice | [113] |
| i.p. | Oxidative stress | 100 mg/kg for 11 days | Effective in imparting protection against the nephrotoxic effect | Rats | [114] |
| Technique | Excipients | Study Outcomes | Ref. |
|---|---|---|---|
| Polymeric nanoparticles | |||
| Solvent evaporation method | Poly (lactic-co-glycolic), Phosphatidylcholine, Hydroxypropyl-β-cyclodextrin | Relative bioavailability of phospholipid complex based PLGA nanoparticles improved by 5.57 while cyclodextrin complex based PLGA nanoparticles showed 8.85-fold enhancement of relative bioavailability in comparison to DAI suspension at dosage of 10 mg/kg in Sprague Dawley rats via p.o. administration | [26] |
| Antisolvent method | Zein, Coumarin-6, TPGS-1000 | Cmax and AUC0–12h was increased by 2.64-fold and 2.4-fold, respectively as compared to daidzin solution on p.o. administration of zein nanoparticles in mice | [119] |
| Emulsion solvent diffusion method | PLGA, Polyvinyl alcohol | Nanoparticles exhibited sustained drug release. Neurotoxic effects at high dosages of DAI (200 µM and 300 µM) was decreased while maintaining cytotoxic effects on U87MG glioma cell lines | [120] |
| Solid lipid nanoparticles | |||
| Hot homogenization method | Egg phosphatidylcholine, Compritol 800, polyethylene glycol, phosphatidylethanolamine | AUC0–∞ from i.v. administration of DAI NPs and free DAI was found 83.62 ± 1.89 µg·h/mL and 28.29 ± 1.29 µg·h/mL, respectively, which illustrated bioavailability enhancement in Sprague Dawley rats. SLNs (i.v.) exhibited superior result on CVS of Beagle dogs via reduction of myocardial oxygen consumption and coronary resistance in heart in contrast to DAI suspension (p.o.) or i.v. solution. SLNs also revealed superlative action on cerebrovascular system through enhancing cerebral blood flow and decreasing cerebrovascular resistance in Beagle dogs | [121] |
| Nanostructured lipid carriers | |||
| Emulsification and low temperature solidification method | Azone, lecithin, Triethanolamine, Capric triglyceride, Tetrahydrofuran | NLC-nanofibers achieved high permeation of 21.71 μg/cm2 at 60 h using rat skin which was 3.78-folds greater than pure drug | [122] |
| Film homogenization technique | Glycerol monostearate, Sodium oleate, Soybean phospholipids | AUC0-t from NLCs was increased by 6.87-times while from phospholipid complexes was enhanced 3.62-folds in comparison to pure DAI in rat model and therefore, NLCs were found effective nanocarriers to increase oral absorption of poorly absorbed lipophilic and hydrophilic compounds | [29] |
| Polymer-lipid nanoparticles | |||
| Emulsification method | PLGA, egg lecithin, azone, tween 20 | In vivo skin retention study using rat skin showed that steady state flux (Jss) from polymer-azone-lipid NPs was enhanced 1.44-folds and 6.01-folds in comparison to polymer-lipid-NPs and DAI solution | [123] |
| Micelles | |||
| Solvent evaporation technique | Lecithin, sodium bile | Intestinal absorption of DAI from lecithin micelles was significantly improved in Sprague Dawley rats and AUC0-t value in rats receiving micelles treatment was twenty times higher than that of free DAI solution | [124] |
| Nanosuspension | |||
| Precipitation-high pressure homogenization method | TPGS, carboxylated chitosan, Poloxamer 188, PVP-K30, Cremophor, PEG 600, β cyclodextrin, Soy lecithin, sodium dodecyl sulphate | In vivo pharmacokinetic study of nanosuspension formulations in Sprague Dawley rats illustrated bioavailability enhancement by 1.63 to 2.19 times than crude drug suspension via p.o administration at 14 mg/kg dose | [125] |
| Media milling techniques | Pluronic, sodium dodecyl sulphate, PVP-K30 | The saturation solubility and dissolution rate of DAI was increased through fabrication of nanosuspension. Enhanced cytotoxicity effect was observed in RG2-GBM tumor cells | [27] |
| Nanocomplexes | |||
| Thermal treatment | Whey protein isolate | Effectively inhibited crystallization, induced 2-fold solubility enhancement and increased DAI stability | [126] |
| Nanoemulsion | |||
| High-pressure homogenization | Lipoid S100, Tween 80, sodium dodecyl sulfate, Fetal bovine Serum, Ethyl oleate | Cell viability assay using melanoma cell lines (SKMEL30) revealed that nanoemulsion induced significant cell death in comparison to pure DAI (p < 0.05) for 48 h of incubation period. However, insignificant (p > 0.05) cytotoxic effects were shown by nanoemulsion in human dermal fibroblast (PCS-201-012, normal) cell lines in comparison to DAI solutions and blank formulations for 24 and 48 h of incubation period | [127] |
| Liposomes | |||
| Ultrasonication and lipid film hydration | Soybean phosphatidylcholine, cholesterol, DSPE-mPEG2000 | In vivo pharmacokinetic of liposome in Sprague Dawley rats demonstrated that t1/2, MRT0-t and AUC0-t of DAI increased by 1.8-, 1.6- and 2.5-fold in comparison to free DAI | [128] |
| Self-Micro Emulsifying Drug Delivery System | |||
| Emulsification | Cremophor RH 40, Tween 80, Polyethylene glycol 400 | The dissolution rate of SMEDDS was significantly enhanced in contrast to tablets. In vivo pharmacokinetic study in Sprague Dawley rats revealed that AUC0-12h from SMEDDS and DAI suspension (10 mg/kg, p.o.) were 954.32 ± 158.30 ng/mL·min and 380.98 ± 67.59 ng/mL·min, respectively which showed 2.5-fold amplification in bioavailability. | [129] |
| Study Tile | Sponsor | Condition | Study Type/Allocation/Intervention Model | NCT no. |
|---|---|---|---|---|
| Whole soy and DAI on reduction of blood pressure in postmenopausal Chinese women | Chinese University of Hong Kong | Hypertension | Interventional/Randomized/Parallel assignment | 01270737 |
| Effects of soy isoflavones on menopausal hot flashes | Beth Israel Deaconess Medical Center | Menopausal symptoms | Interventional/Randomized/Parallel assignment | 00179556 |
| Effect of two different isoflavone supplement preparations on gene-expression in postmenopausal women (ISOII) | Wageningen University | Post menopause | Interventional/Randomized/Crossover assignment | 01556737 |
| The effects of soy isoflavones to improve the metabolism of glucose and lipids | Sun Yat-sen University | Type 2 diabetes mellitus | Interventional/Randomized/Parallel Assignment | 00951912 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, S.; Grewal, S.; Sharma, N.; Behl, T.; Gupta, S.; Anwer, M.K.; Vargas-De-La-Cruz, C.; Mohan, S.; Bungau, S.G.; Bumbu, A. Unveiling the Pharmacological and Nanotechnological Facets of Daidzein: Present State-of-the-Art and Future Perspectives. Molecules 2023, 28, 1765. https://doi.org/10.3390/molecules28041765
Singh S, Grewal S, Sharma N, Behl T, Gupta S, Anwer MK, Vargas-De-La-Cruz C, Mohan S, Bungau SG, Bumbu A. Unveiling the Pharmacological and Nanotechnological Facets of Daidzein: Present State-of-the-Art and Future Perspectives. Molecules. 2023; 28(4):1765. https://doi.org/10.3390/molecules28041765
Chicago/Turabian StyleSingh, Sukhbir, Sonam Grewal, Neelam Sharma, Tapan Behl, Sumeet Gupta, Md. Khalid Anwer, Celia Vargas-De-La-Cruz, Syam Mohan, Simona Gabriela Bungau, and Adrian Bumbu. 2023. "Unveiling the Pharmacological and Nanotechnological Facets of Daidzein: Present State-of-the-Art and Future Perspectives" Molecules 28, no. 4: 1765. https://doi.org/10.3390/molecules28041765