Abstract
When it comes to studying the effect of food bioactives on gut health, one of the essential steps that needs to be assessed is characterizing specific effects of the bioactives on the physical barrier of the lumen, the gastrointestinal tissue. In addition to studying the effects on transport function (e.g. by using Ussing chambers or cell culture systems), it is of great interest to evaluate the effects on morphology, cell biology, gene expression, and relevant functions of different cell types that are resident in the gastrointestinal (GI) tract. An ideal near-physiological model should contain a mixture of different GI epithelial cells (e.g. Paneth cells, goblet cells, absorptive and hormone secretive epithelial cells), which can be cultured indefinitely. Recently, the culture and applications of long-term primary multi-cellular cluster structures gastrointestinal organoids (or enteroids) have been demonstrated, and within the last 5 years the number of researchers that commonly use this tissue culture model has increased rapidly. This multi-cellular system may be a promising addition for existing ex vivo and alternative for animal models for testing effects of food bioactives on the intestinal tissue, and could provide a model for pre-screening of compounds prior to moving to the large scale testing systems. Moreover, intestinal organoids can be cultured from different species (e.g. human, pig and mouse). In this chapter we will focus on organoids cultured from mouse and pig crypt cells. We will give a short overview on how to isolate, culture, incubate, and apply them in different research fields.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Gastrointestinal Organoids
Several attempts have been made to isolate the proliferative regions of the intestinal epithelium from different species (e.g. mouse, porcine, human) (Pageot et al. 2000; Agopian et al. 2009). Proliferative regions of the intestinal epithelium consist of the transit amplifying cells, which are undifferentiated progenitor cells that can differentiate into all different epithelial cells of the intestinal epithelium. Initially cultured intestinal tissue contained crypt and villus domains, resembling the intestinal epithelial architecture present in vivo. However, these cultured intestinal tissue pieces from the intestinal epithelial could be maintained in culture for up to several days at maximum, and thus were not self-renewing.
The need for a self-sustaining, long-term GI model remained. The big breakthrough came when Dr. Hans Clevers and colleagues, for the first time, identified the intestinal stem cells by thorough lineage tracing experiments (Barker et al. 2007). These experiments were performed over a period of 60 days in mice, and confirmed the presence of Lgr5 (marker for adult stem cells)-positive stem cells in small intestinal and colonic crypts. These stem cells are able to differentiate in to all intestinal epithelial cells (enterocytes, Paneth cells, Goblet cells, enteroendocrine cells, but also stem and progenitor cells), as shown in vivo and in culture where these Lgr5-positive cells formed so-called ‘mini-guts’ or ‘organoids’ (Sato et al. 2009) (Fig. 22.1). Secretion of mucins into the luminal space and lysozyme production by Panneth cells illustrate the functionality of this epithelium (McCracken et al. 2011).
Schematic image of an intestinal organoid. All epithelial cell types normally present in vivo are also present in the cultured intestinal organoids, as indicated by different colored cells. Figure adapted from Roeselers et al. (2013)
The discovery of these stem cells opened a new world of the possibilities for GI culture methods, by manipulation of these cells. The great potential of these now self-sustaining ‘mini-guts’ in the field of transplantation and regenerative medicine was immediately evident, and soon engraftment of intestinal organoids in mice was successfully performed (Yui et al. 2012; Shaker and Rubin 2012). So far, the human organoid transplantation has not been performed in humans yet, although human intestinal organoids can be cultured and maintained in culture for some time now (Sato et al. 2011a).
Recently human organoids cultured from induced pluripotent stem cells (iPSCs) have been transplanted into mice (in vivo), where intestinal adaptive capacity as well as epithelial function (peptide uptake and permeability) have been demonstrated in the transplants (Watson et al. 2014). In addition, Clevers and colleagues (University Medical Center Utrecht, the Netherlands), proposed treatment for children suffering from a rare gastrointestinal disease (microvillus inclusion disease) by transplantation of stem-cell derived organoids (Wiegerinck et al. 2014), but the outcomes of these studies have not been published yet. Intestinal organoids have been applied to study cystic fibrosis by using primary organoids from cystic fibrosis patients. This model facilitates diagnosis, functional studies, drug development and personalized medicine approaches in cystic fibrosis (Dekkers et al. 2012).
Recently, we have demonstrated that intestinal organoids provide a powerful model for host–microbiome interaction studies (Lukovac et al. 2014). In this study we observed that specific gut bacteria and their metabolites differentially modulate epithelial transcription in mouse organoids (Lukovac et al. 2014).
2 General Protocol
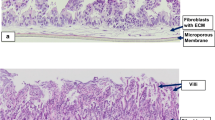
Isolation of mouse intestinal crypts and organoid culture, adapted from (Sato and Clevers 2013) is schematically represented in Fig. 22.2. A detailed protocol of the culture protocol is described below.
2.1 Small Intestinal Crypt Isolation
Thaw aliquots of Matrigel™ Basement Membrane Matrix (BD Biosciences) on ice before isolation and pre-incubate a 24-well plate in a CO2-incubator (5 % CO2, 37 °C). Matrigel™ is a solubilized gelatinous protein mixture and is derived from the Engelbreth–Holm–Swarm (EHS) mouse sarcoma cells. The extract resembles the complex extracellular environment found in many tissues and is commonly used as a substrate for culturing cells. At room temperature, Matrigel™ polymerizes into a three dimensional structure that is useful for both cell culture and studying cellular processes in three dimensions, including cell migration.
Isolate a piece of mouse small intestine (at least 5 cm) and open longitudinally. Wash the intestine with ice cold PBS until most of the luminal contents are cleared and scrape off the villi using a coverslip. After another washing with ice-cold PBS, cut the intestine into 2–4 mm pieces with scissors and transfer them to a 50-mL tube. Add 30 mL ice-cold PBS and wash the fragments by gently pipetting the fragments up and down with a 10 mL pipette and discard supernatant after settling down. Repeat this step 5–10 times until the supernatant is almost clear. Next, add 30 mL of ice-cold crypt isolation buffer (5 mM EDTA in PBS; one can also use higher EDTA concentration, up to 10 mM if yields are low) and gently rock the tube at 4 °C for 30 min. Keep pipetting up and down the tissue in solution every 10 min in order to release as much epithelium as possible. After settling down the fragments, the supernatant can be removed and 20 mL of ice-cold PBS can be added to wash the fragments using a pipet. Repeat this procedure when the fragments are settled down, in order to release most of the crypts, that will also settle down after some time. Villous fractions present in the supernatant are discarded and crypts fractions are passed through a 70-mm cell strainer and collected into 50 mL tube(s), after adding 5 % FBS to a crypt solution. Spin down the crypt fractions at 300×g 5 min and resuspend the pellets in 10 mL of ice-cold basal culture medium (advanced Dulbecco’s modified Eagle medium/F12 supplemented with penicillin/streptomycin, 10 mmol/L HEPES, Glutamax, 1 × N2, 1 × B27, and 1 mmol/L N-acetylcysteine). The suspension is transferred to a 15 mL Falcon tube and centrifuged at 150–200×g for 2 min, to remove single cells (mostly lymphocytes), which end up in the supernatant. This washing step should be repeated 2–3 times until most single cells are cleared. After the washing steps, the number of crypts can be calculated (take 10 μL of the crypts suspension and count numbers of crypts using a heamocytometer by inverted microscopy; the total number of crypts = the number of crypts counted × 1,000). It should be noted that at this point it is difficult to distinguish true crypts from other epithelial debris, hence the count is only a rough estimate.
2.2 Small Intestinal Organoid Culture
Centrifuge small intestinal crypts, and remove supernatant as much as possible to avoid dilution of Matrigel™ in the next step. Keep the tube at 4 °C and resuspend the crypts pellet in Matrigel™ (200–500 crypts/50 μL matrigel). Pipet 50 μL of the crypt-Matrigel™ suspension into the pre-warmed 24-well plate. The suspension should be applied on the center of the well so a hemispherical droplet can be formed. Transfer the plate back into the CO2 incubator (5 % CO2, 37 °C) as soon as possible after the seeding. Allow the Matrigel™ to solidify for 5–10 min and add 500 μL complete organoid culture medium per well. For preparation of the organoid culture medium (e.g. amount of growth factors) check Table 22.1. Place the 24-wells plate in a CO2-incubator and refresh the culture medium every 4–6 days.
2.3 Small Intestinal Organoid Passage
Crypt organoids can be passaged 7–14 days after seeding. Place the plate with organoids on ice to allow the matrigel to dissolve. Remove the culture medium and gently break up the Matrigel™ by pipetting with a 100–1,000 μL-pipette. Resuspend the organoids in 1–2 mL basal culture medium and transfer them to a 15 mL-tube. Gently disrupt the organoids using a fire-polished Pasteur pipette to remove released dead cells and single cells. Pellet everything by centrifuging at 300×g for 5 min, and wash the organoids afterwards with 10 mL basal culture medium. Pellet again at the same speed and add the correct amount of Matrigel™, namely 50 μL per well that you would like to plate. Count the “crypts/immature organoids” as described before (by hemocytometer) and pipet the Matrigel™ suspension with crypts (50 μL per well) into a new 24 culture plate and place the plate back in CO2 incubator (5 % CO2, 37 °C) to culture the organoids.
3 Monitoring Viability
Organoid culture and development across time after isolation, and post-passage can be verified using microscopy. Mainly, the dead cells of the organoid tissue will be visible in the central part of the organoid, corresponding to the intestinal lumen in vivo (these aggregates of dead cells can be visualized by microscopy as shown in Fig. 22.3 at day 5–7). Figure 22.3 shows a very simplified summary of a mouse intestinal crypt development into a mature organoid structure. Additional conformation of the viability of the organoids can be performed upon by the use of the LDH toxicity assay or the immunofluorescent staining procedures for viability markers (e.g. apoptotic caspase 3 staining), but the organoids have to be sampled destructively in order to perform this assay, thus this step can be only applied at the final stages of specific experiments. It should be noted that once growth, normal cell proliferation and differentiation stops, and organoids start to die, that this will immediately become visible, thus it is essential to monitor the organoid growth and proliferation on a daily basis.
Phase contrast images of a developing mouse intestinal crypt into a organoid in culture. (a) immature organoid in culture 0.5–1 day after crypt isolation; (b) mature organoid in culture 3–5 days after crypt isolation; (c) mature organoid in culture 5–14 days after crypt isolation, ready to be passaged (note the accumulated debris of dead cells in the lumen of the organoid). This morphology is representative for other species as well [image adapted from Lukovac et al. (2014)]
Culture and maintenance of intestinal organoids, relies on the presence and activity of mature (intestinal) stem cells. Even though intestinal organoids can be isolated and cultured from human induced pluripotent stem cells (iPPS), as described by McCracken et al. (2011), most studies culture organoids from mature stem cells from the intestinal crypt regions. The reason for this is that this method described is relatively elaborative and it takes much longer to mature the intestinal organoids in culture compared to the other method based on the organoid culture from adult intestinal cells. For a detailed protocol of iPPS-based culture of the intestinal tissue we refer to McCracken et al. (2011). As mentioned previously, lineage studies confirmed the stem cell hierarchy in intestinal organoids, either by fast cycling Lgr5+- or slowly cycling Bmi1+-stem cell activity (Sangiorgi and Capecchi 2008; Sato et al. 2009). Stem cell-based organoid cultures are an attractive model due to the presence of the self-renewing capacity; they can be passaged every 5–7 days. In addition, the structure and hierarchy of the mature organoids (after 5–7 days of culturing), highly resembles the in vivo intestinal epithelium (Fig. 22.1). Similar to the intestinal epithelium, stem cells and highly proliferative transit amplifying cells reside in the crypt-like domain of the organoids (Fig. 22.1). Differentiated cell types reside in the villus-region of the organoids and include enterocytes, goblet cells, Paneth cells, and enteroendocrine cells. These cells can be identified using immunohistochemistry with intestinal epithelial cell-specific markers.
4 General Advantages and Limitations of Intestinal Organoid Systems
Despite the described significant advances in culturing organoids, this system has some limitations. A major advantage of intestinal models in which an apical to basolateral polarity is preserved is the possibility to characterize epithelial transport mechanisms and barrier integrity upon exposure to microorganisms and microbial components. Indeed intestinal organoids consist of polarised, columnar epithelia. However, the inwards orientation of the epithelia (i.e. villi protrude into the lumen of the organoids) makes the apical side relatively inaccessible for direct experimental stimulation (Fig. 22.1).
Also, the organoids lack several essential components of the living digestive tract, such as the enteric nervous system, the vascular system, lymphatic systems and functional adaptive and innate immune systems. Additionally, the 3D architecture is not as regular as seen in vivo, and the crypt-villus structures are variable in size and shape from one organoid to another.
Regardless of these drawbacks, this model offers great experimental utility for understanding and modeling human intestinal development, physiology, and host–microbe interactions. Indeed, this model has several other advantages, such as a long-term culturing, broad range host species and GI tract compartments (stomach, ileum, colon) and gene manipulation possibilities (Koo et al. 2011). Moreover, this system provides a viable starting point for the development of screening platforms for pharmaceutical and food compounds.
Further expansion of this system will lead to broader application range and expansion of the read out possibilities. One example is transition of the existing system towards a structure with the apical/luminal compartment exposed on the outer site of the organoids, which will make the apical site of the organoids experimentally more accessible. Furthermore, this system might be a promising tool in studies on epithelial interactions with food bioactive in individual subjects, as it has been demonstrated that organoids can be cultured from human intestinal biopsy samples (Sato et al. 2011b).
References
Agopian VG, Chen DC, Avansino JR, Stelzner M (2009) Intestinal stem cell organoid transplantation generates neomucosa in dogs. J Gastrointest Surg 13:971–982
Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, Clevers H (2007) Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 449:1003–1007
Carmon KS, Gong X, Lin Q, Thomas A, Liu Q (2011) R-spondins function as ligands of the orphan receptors LGR4 and LGR5 to regulate Wnt/beta-catenin signaling. Proc Natl Acad Sci U S A 108:11452–11457
Dekkers JF, Wiegerinck CL, de Jonge HR, de Jong NWM, Bijvelds MJC, Nieuwenhuis EES, van den Brink S, Clevers H, van der Ent CK, Middendorp S (2012) WS14.5 a functional CFTR assay using primary cystic fibrosis intestinal organoids. J Cyst Fibros 11:S32
Koo B-K, Stange DE, Sato T, Karthaus W, Farin HF, Huch M, van Es JH, Clevers H (2011) Controlled gene expression in primary Lgr5 organoid cultures. Nat Methods 9:81–83
Lukovac S, Belzer C, Pellis L, Keijser BJ, de Vos WM, Montijn RC, Roeselers G (2014) Differential modulation by Akkermansia muciniphila and Faecalibacterium prausnitzii of host peripheral lipid metabolism and histone acetylation in mouse gut organoids. mBio 5(4):e01438-14
McCracken KW, Howell JC, Wells JM, Spence JR (2011) Generating human intestinal tissue from pluripotent stem cells in vitro. Nat Protoc 6:1920–1928. doi:10.1038/nprot.2011.410
Pageot LP, Perreault N, Basora N, Francoeur C, Magny P, Beaulieu JF (2000) Human cell models to study small intestinal functions: recapitulation of the crypt-villus axis. Microsc Res Tech 49:394–406
Roeselers G, Ponomarenko M, Lukovac S, Wortelboer HM (2013) Ex vivo systems to study host–microbiota interactions in the gastrointestinal tract. Best Pract Res Clin Gastroenterol 27:101–113
Sangiorgi E, Capecchi MR (2008) Bmi1 is expressed in vivo in intestinal stem cells. Nat Genet 40:915–920
Sato T, Clevers H (2013) Primary mouse small intestinal epithelial cell cultures. Methods Mol Biol 945:319–328. doi:10.1007/978-1-62703-125-7_19
Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, van Es JH, Abo A, Kujala P, Peters PJ, Clevers H (2009) Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459:262–265
Sato T, Stange DE, Ferrante M, Vries RGJ, Van Es JH, Van Den Brink S, Van Houdt WJ, Pronk A, Van Gorp J, Siersema PD, Clevers H (2011a) Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology 141:1762–1772. doi:10.1053/j.gastro.2011.07.050
Sato T, van Es JH, Snippert HJ, Stange DE, Vries RG, van den Born M, Barker N, Shroyer NF, van de Wetering M, Clevers H (2011b) Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature 469:415–418
Shaker A, Rubin DC (2012) Stem cells: one step closer to gut repair. Nature 485:181–182. doi:10.1038/485181a
Watson CL, Mahe MM, Múnera J, Howell JC, Sundaram N, Poling HM, Schweitzer JI, Vallance JE, Mayhew CN, Sun Y, Grabowski G, Finkbeiner SR, Spence JR, Shroyer NF, Wells JM, Helmrath MA (2014) An in vivo model of human small intestine using pluripotent stem cells. Nat Med. doi:10.1038/nm.3737
Wiegerinck CL, Janecke AR, Schneeberger K, Vogel GF, Van Haaften-Visser DY, Escher JC, Adam R, Thöni CE, Pfaller K, Jordan AJ, Weis CA, Nijman IJ, Monroe GR, Van Hasselt PM, Cutz E, Klumperman J, Clevers H, Nieuwenhuis EES, Houwen RHJ, Van Haaften G, Hess MW, Huber LA, Stapelbroek JM, Müller T, Middendorp S (2014) Loss of syntaxin 3 causes variant microvillus inclusion disease. Gastroenterology. doi:10.1053/j.gastro.2014.04.002
Yui S, Nakamura T, Sato T, Nemoto Y, Mizutani T, Zheng X, Ichinose S, Nagaishi T, Okamoto R, Tsuchiya K, Clevers H, Watanabe M (2012) Functional engraftment of colon epithelium expanded in vitro from a single adult Lgr5+ stem cell. Nat Med 18:618–623
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this chapter
Cite this chapter
Lukovac, S., Roeselers, G. (2015). Intestinal Crypt Organoids as Experimental Models. In: Verhoeckx, K., et al. The Impact of Food Bioactives on Health. Springer, Cham. https://doi.org/10.1007/978-3-319-16104-4_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-16104-4_22
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15791-7
Online ISBN: 978-3-319-16104-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)