Abstract
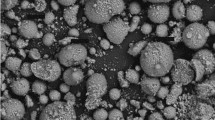
The association of macrophages engaged in polymethylmethacrylate (PMMA) particle phagocytosis with pockets of inflammatory cells is a pathognomonic feature of the aseptically loose interface not present at the well-fixed interface. The mechanism by which the presence of PMMA particles leads to cellular recruitment, bone resorption, and ultimate loosening is poorly understood. Granulocyte macrophage colony stimulating factor (GM-CSF) and interleukin 6 (IL-6), cytokines released by osteoblasts, stimulate the recruitment of macrophages into sites of inflammation. We show that exposure of macrophages to PMMA particles stimulated release of tumor necrosis factor (TNF), but no increase in prostaglandin E2 (PGE-2) or interleukin 1. Incubation of osteoblasts with conditioned medium from macrophages exposed to PMMA particles led to release of GMCSF, IL-6, and PGE-2. Incubation of the PMMA/macrophage medium with antibodies to TNF prior to osteoblast exposure inhibited release of GM-CSF, IL-6, and PGE-2 by the osteoblasts. Our data demonstrate that exposure of macrophages to PMMA particles leads to the release of TNF which then stimulates osteoblasts to produce GMCSF, IL-6, and PGE-2. Based upon the results of this study, we propose that the process of cellular recruitment in aseptic loosening is initiated when the mechanical failure of the cement mantle leads to the production of PMMA particles. These particles are phagocytized by macrophages leading to the production of TNF. TNF stimulates surrounding osteoblasts to produce GM-CSF, IL-6, and PGE-2 which leads to recruitment of macrophages and osteoclasts into the area of the bone-cement interface. The recruitment of these cells potentiates this process leading to bone resorption and ultimately, clinical loosening of prosthetic joint implants.
Similar content being viewed by others
References
Charnlev J (1970) The reaction of bone to self-curing acrylic cement. J. Bone Joint Surg 52B:340–353
Bell RS, Schatzker J, Fomasier VL, Goodman SB (1985) A study of implant failure in the Wagner resurfacing arthroplasty. J Bone Joint Surg 67A:1165–1175
Freeman MAR, Bradley GW, Revell PA (1982) Observations upon the interface between bone and polymethylmethacrylate cement. J Bone Joint Surg 64B:489–493
Goldring SR, Schiller AL, Roelke CM, O'Neil DA (1983) The synovial-like membrane at the bone-cement interface in loose total hip replacements and its proposed role in bone lysis. J Bone Joint Surg 64A:575–584
Pollice PF, Silverton S, Horowitz SM (1995) PMMA-stimulated macrophages increase rat osteoblast precursor recruitment through their effect on osteoblasts in vitro. J Orthop Res (in press)
Horowitz SM, Doty SB, Rapuano BP, Lane JM, Burstein AH (1994) Role of the macrophage and the osteoblast in aseptic loosening. Calcif Tissue Int 54:320–324
Horowitz SM, Doty SB, Lane JM, Burstein AH (1993) Studies of the mechanism by which the mechanical failure of polymethylmethacrylate leads to bone resorption. J Bone Joint Surg 75A:802–813
Horowitz MC, Jilka RL (1992) Colony-stimulating factors and bone remodeling. In: Gowen M (ed) Cytokines and bone metabolism. CRC Press, Boca Raton, pp 194–201
Lowik CWGM (1992) Differentiation inducing factors leukemia inhibitory factor and interluekin-6. In: Gowen M (ed) Cytokines and bone metabolism. CRC Press, Boca Raton, pp 300–324
Collins DA, Chambers TJ (1992) Prostaglandin E2 promotes osteoclast formation in murine hematopoietic cultures through an action on hematopoietic cells. J Bone Miner Res 7(5):555–561
Collins DA, Chambers TJ (1991) Effect of prostaglandins E1, E2, and F2 on osteoclast formation in mouse bone marrow cultures. J Bone Miner Res 6(2):157–164
Health JK, Saklatvala J, Meikle MC, Atkinson SJ, Reynolds JJ (1985) Pig interleukin 1 (catabolin) is a potent stimulator of bone resorption in vitro. Calcif Tissue Int 37:95–97
Klein DC, Raisz LR, (1970) Prostaglandins: stimulation of bone resorption in tissue culture. Endocrinology 86:1436–1440
Kurland JI, Bockman R, (1978) Prostaglandin E production by human blood monocytes and mouse peritoneal macrophages. J Exp Med. 147:952–957
Tashjian AH, Voelkel EF, Lazzaro M, Goad D, Bosma T, Levine L (1987) Tumor necrosis factor—a (cachectin) stimulates bone resorption in mouse calvaria via a prostaglandin-mediated mechanisms. Endocrinology 120(5):2029–2036
Vaes G (1988) Cellular biology and biochemical mechanism of bone resorption: a review of recent developments on the formation, activation and mode of action of osteoclasts. Clin Orthop 231:239–271
Levin J, Bang FB (1968) Clottable protein in limulus: its localization and kinetics of coagulation by endotoxin. Diathesis Haemorrhagica 19:186–197
Franceschi RT, Bhanumathi SI (1992) Relationship between collagen synthesis and expression of the osteoblastic phenotype in MC3T3-E1 cells. J Bone Miner Res 7(2):235–246
Kurihara N, Ishizuka S, Kiyoki M, Yoshiyuki H, Ikeda K, Kumegawa M (1986) Effects of 1,25-dihydroxyvitamin D3 on osteoblastic MC3T3-E1 cells. Endocrinology 118:940–947
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Horowitz, S.M., Purdon, M.A. Mechanisms of cellular recruitment in aseptic loosening of prosthetic joint implants. Calcif Tissue Int 57, 301–305 (1995). https://doi.org/10.1007/BF00298886
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00298886