Abstract
Background
Aged Care Assessment Teams (ACATs) in Australia assess the care needs of frail older people. Despite being at high risk of medication-related problems (MRPs), ACAT patients do not routinely receive a comprehensive medication review.
Objectives
The aims of the study were to compare three methods for facilitating a pharmacist-led comprehensive medication review for people referred to an ACAT, and compare MRPs identified via ACAT usual care with those identified via pharmacist-led medication reviews.
Methods
A prospective, randomized, comparative study involving 80 community-dwelling patients (median age 84 years) referred to an ACAT in Melbourne, Australia, was conducted.
Following ACAT assessment (usual care), a clinical pharmacist reviewed all participating patients’ ACAT files to identify potential MRPs not identified by the ACAT (medication review method 1). Patients were then randomized into two groups. Group A received information about the Australian government-funded, general practitioner (GP)-initiated Home Medicines Review (HMR) programme, and a letter was sent to their GP recommending an HMR (GPHMR; medication review method 2). Group B patients were referred directly to a clinical pharmacist associated with the ACAT for an ACAT-initiated pharmacist home medicines review (APHMR; medication review method 3); the pharmacist arranged a home visit, obtained a thorough medication history and conducted a comprehensive medication review.
The main outcome measures were the proportion of patients who received a pharmacist home visit within 28 days; the number of MRPs identified by ACAT usual care, pharmacist review of ACAT files, and APHMR, and their clinical risk (assessed by a geriatrician-pharmacist panel); and patients’, GPs’ and ACAT clinicians’ opinions about pharmacist medication review.
Results
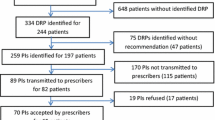
Three hundred patients were referred to the ACAT, and 80 were recruited into the study. Thirty-six of 40 APHMR patients (90.0%) received a pharmacist home visit within 28 days, compared with 7/40 GPHMR patients (17.5%) [p<0.001].
Twenty-one MRPs were identified via ACAT usual care. Pharmacist review of ACAT files identified a further 164 potential MRPs (median 2.0 per patient; inter-quartile range [IQR] 1.0–3.0); however, in patients who received an APHMR, 35/82 potential MRPs (42.7%) turned out not to be actual problems, most commonly because of discrepancies between the patient’s ACAT medication list and the medications currently being used by the patient (median 3.0 discrepancies per patient; IQR 2.0–5.5). APHMR identified a further 79 MRPs (median 2.0; IQR 1.0–3.0).
One hundred and twenty-two MRPs were included in APHMR reports sent to patients’ GPs. Of these, 94 (77.0%) were assessed as being associated with a moderate, high or extreme risk of an adverse event. Sixty-four APHMR recommendations (52.5%) led to changes to patients’ medication regimens or medication management.
Thirty-six of 39 GPs (92.3%) who provided feedback reported that pharmacist medication reviews were useful. Patients (or their carers) also reported that pharmacist home visits were useful: median rating 4.25 out of 5 (IQR 4.0–5.0). Seven of 11 ACAT clinicians (77.8%) agreed that pharmacist-led medication review should be a standard component of ACAT assessments.
Conclusions
ACAT assessments without pharmacist involvement detected fewer MRPs than any of the evaluated pharmacist-led medication review methods. APHMR was more effective than pharmacist review of routinely collected ACAT data, and more reliable and timely than referral to the patients’ GP for a GPHMR.







Similar content being viewed by others
References
Australian Institute of Health and Welfare. Pathways in Aged Care: program use after assessment. Data linkage series no. 10. CSI 10. Canberra (ACT): AIHW, 2011 Feb 2 [online]. Available from URL: http://www.aihw.gov.au/publication-detail/?id=6442475608 [Accessed 2011 Sep 28].
LoGiudice D, Waltrowicz W, Ames D, et al. Health care costs of people referred to an Aged Care Assessment Team: the effect of cognitive impairment. Aust N Z J Public Health 1997; 21: 311–5.
Elliott RA, Woodward MC. Medication-related problems in patients referred to aged care and memory clinics at a tertiary care hospital. Australas J Ageing 2011; 30: 124–9.
Atkin PA, Veitch PC, Veitch EM, et al. The epidemiology of serious adverse drug reactions among the elderly. Drugs Aging 1999; 14: 141–52.
Leendertse AJ, Egberts ACG, Stoker LJ, et al. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med 2008; 168: 1890–6.
Field TS, Mazor KM, Briesacher B, et al. Adverse drug events resulting from patient errors in older adults. J Am Geriatr Soc 2007; 55: 271–6.
Johnson M, Griffiths R, Piper M, et al. Risk factors for an untoward medication event among elders in community-based nursing caseloads in Australia. Public Health Nurs 2005; 22: 36–44.
Australian Pharmaceutical Advisory Council. Guiding principles for medication management in the community. Canberra (ACT): Commonwealth of Australia, 2006 [online]. Available from URL: http://www.health.gov.au/internet/main/publishing.nsf/Content/apac-publications-guiding [Accessed 2011 Sep 28].
Shrank WH, Polinski JM, Avorn J. Quality indicators for medication use in vulnerable elders. J Am Geriatr Soc 2007; 55 (Suppl. 2): S373–S82.
Kroger E, Tourigny A, Morin D, et al. Selecting process quality indicators for the integrated care of vulnerable older adults affected by cognitive impairment or dementia. BMC Health Serv Res 2007; 7: 195.
Hilmer SN. The dilemma of polypharmacy. Australian Prescriber 2008;31:2–3.
Richmond S, Morton V, Cross B, et al., For the RESPECT Trial Team. Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings. Br J Gen Pract 2010; 59: 14–20.
Holland R, Desborough J, Goodyer L, et al. Does pharmacistled medication review help to reduce hospital admissions and deaths in older people? A systematic review and metaanalysis. Br J Clin Pharmacol 2007; 65: 303–16.
Sorensen L, Stokes JA, Purdie DM, et al. Medication reviews in the community: results of a randomized, controlled effectiveness trial. Br J Clin Pharmacol 2004; 58: 648–64.
Crotty M, Halbert J, Rowett D, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 2004; 33: 612–7.
Roughead EE, Barratt JD, Ramsay E, et al. The effectiveness of collaborative medicine reviews in delaying time to next hospitalization for patients with heart failure in the practice setting: results of a cohort study. Circ Heart Fail 2009; 2: 424–8.
Roughead EE, Barratt JD, Ramsay E, et al. Collaborative home medicines review delays time to next hospitalization for warfarin associated bleeding in Australian war veterans. J Clin Pharm Ther 2011; 36: 27–32.
Castelino RL, Bajorek BV, Chen TF. Retrospective evaluation of home medicines review by pharmacists in older Australian patients using the Medication Appropriateness Index. Ann Pharmacother 2010; 44: 1922–9.
Hanlon J, Weinberger M, Samsa G. A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med 1996; 100: 428–37.
Meredith S, Feldman P, Frey D, et al. Improving medication use in newly admitted home healthcare patients: a randomized controlled trial. J Am Geriatr Soc 2002; 50: 1484–91.
Gilbert AL, Roughead EE, Beilby J, et al. Collaborative medication management services: improving patient care. Med J Aust 2002; 177: 189–92.
Home Medicines Review (HMR). Canberra (ACT): Australian Government [online]. Available from URL: http://www.medicareaustralia.gov.au/provider/pbs/fourth-agreement/hmr.jsp [Accessed 2011 Sep 28].
Lee CY, George J, Elliott RA, et al. Prevalence of medication-related risk factors among retirement village residents: a cross-sectional survey. Age Ageing 2010; 39: 581–7.
Roughead EE. Managing adverse drug reactions: time to get serious. Med J Aust 2005; 182: 264–5.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–98.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965; 14: 61–5.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969; 9: 179–86.
FitzGerald RJ. Medication errors: the importance of an accurate drug history. Br J Clin Pharmacol 2009; 67: 671–5.
Watt A, Fernandes O, Colquhoun M, et al. Assuring medication accuracy at transitions in care: medication reconciliation. WHO Collaborating Centre for Patient Safety and Institute for Safe Medication Practices, 2009 [online]. Available from URL: https://www.high5s.org/pub/Manual/TrainingMaterials/MR_Getting_Started_Kit.pdf [Accessed 2011 Sep 28].
Pharmaceutical Society of Australia. Comprehensive medication review: professional practice standards. Canberra (ACT): Pharmaceutical Society of Australia, 2006.
Elliott RA, Woodward MC. Assessment of risk associated with medication-related problems in elderly outpatients. J Pharm Pract Res 2009; 39: 109–13.
Levy H. Self-administered medication-risk questionnaire in an elderly population. Ann Pharmacother 2003; 37: 982–7.
Oladimeji O, Farris KB, Urmie JG, et al. Risk factors for self-reported adverse drug events among Medicare enrollees. Ann Pharmacother 2008; 42: 53–61.
Bollella G, Angley MT, Pink JA, et al. Optimal level of liaison pharmacist intervention to facilitate a post-discharge home medicines review. J Pharm Pract Res 2008; 38: 107–10.
Angley M, Ponniah AP, Spurling LK, et al. Feasibility and timeliness of alternatives to post-discharge home medicines reviews for high-risk patients. J Pharm Pract Res 2011; 41: 27–32.
Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “there’s got to be a happy medium”. JAMA 2010; 304 (14): 1592–601.
Campbell Research and Consulting. Home Medicines Review program qualitative research project final report. Melbourne (VIC): Department of Health and Ageing, 2008 [online]. Available from URL: http://www.health.gov.au/internet/main/publishing.nsf/Content/hmr-qualitative-research-final-report [Accessed 2011 Sep 28].
Triller DM, Clause SL, Briceland LL, et al. Resolution of drug-related problems in home care patients through a pharmacy referral service. Am J Health Syst Pharm 2003; 60: 905–10.
Sorensen L, Stokes JA, Purdie DM, et al. Medication management at home: medication risk factor prevalence and inter-relationships. J Clin Pharm Ther 2006; 31: 485–91.
Krass I, Smith C. Impact of medication regimen reviews performed by community pharmacists for ambulatory patients through liaison with general medical practitioners. Int J Pharm Pract 2000; 8: 111–20.
Harris A, Gospodarevskaya E, Callaghan J, et al. The cost effectiveness of a pharmacist reviewing medication among the elderly in the community. Australas J Ageing 2001; 20: 179–86.
Rikala M, Korhonen MJ, Sulkava R, et al. The effects of medication assessment on psychotropic drug use in the community-dwelling elderly. Int Psychogeriatr 2011; 23: 473–84.
Commonwealth Department of Health and Ageing. The national strategy for quality use of medicines. Canberra (ACT): Commonwealth of Australia, 2002. ISBN 0 642 82005 8 [online]. Available from URL: http://www.health.gov.au/internet/main/publishing.nsf/content/CA777524C860DFF2CA256F1800468B61/$File/natstrateng.pdf [Accessed 2012 Feb 19].
Australian Government Department of Health and Ageing. National health reform [website]. Canberra (ACT): Commonwealth of Australia [online] Available from URL: http://www.yourhealth.gov.au [Accessed 2012 Feb 19].
Acknowledgements
This study was partially funded by the Jack Brockhoff Foundation. The Foundation had no role in the design or conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review or approval of the manuscript. The authors have no conflicts of interest that are directly relevant to the content of this article.
The authors would like to thank the staff and patients of the Heidelberg Aged Care Assessment Service, Ms Shari de Alwis and Mr Tim Tran (clinical pharmacists) and Mr Kent Garrett (Director of Pharmacy) for their assistance and support. We also thank Dr Johnson George for reviewing a draft of this manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Elliott, R.A., Martinac, G., Campbell, S. et al. Pharmacist-Led Medication Review to Identify Medication-Related Problems in Older People Referred to an Aged Care Assessment Team. Drugs Aging 29, 593–605 (2012). https://doi.org/10.1007/BF03262276
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03262276