Abstract
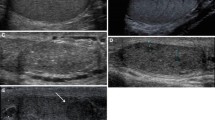
Introduction: Male accessory gland infection (MAGI) exerts a negative influence on male fertility which depends upon its extension. Indeed, we have shown that patients with MAGI involving prostate, seminal vesicles and epididymis have worse sperm parameters compared with patients with prostatitis alone or prostate-vesiculitis. Similarly, MAGI extending bilaterally is associated with a worse sperm output. The aims of this study were to evaluate the prevalence of two different additional ultrasound (US) findings (hypertrophic-congestive and a fibro-sclerotic US form) and to evaluate their semen quality. Materials and methods: One hundred infertile patients with MAGI, diagnosed according to the World Health Organization (WHO) 1993 criteria, were evaluated by scrotal and transrectal ultrasound scans. The control group consisted of 100 healthy, age-matched men. Results: The ultrasound examination confirms two separate US variants of MAGI: a hypertrophic-congestive (prevalence of 56%) and a fibro-sclerotic form (prevalence of 29%). Patients with hypertrophic-congestive MAGI showed higher sperm concentration, motility and normal forms, but also higher sperm leukocytes concentration and seminal reactive oxygen species compared to patients with fibro-sclerotic MAGI. However, all these parameters were significantly worse than those observed in the control group. Discussion: Infertile patients with hypertrophic-congestive MAGI have a better sperm quality compared with patients with fibrosclerotic MAGI; however, they showed higher oxidative stress in semen.
Similar content being viewed by others
References
Rowe P, Comhaire F, Hargreave TB, Mellows HJ eds. WHO manual for the standardized investigation and diagnosis of the infertile couple. Cambridge: Cambridge University Press 1993.
Krieger JN, Nyberg L Jr, Nickel JC. Letter to the editor: NIH consensus definition and classification of prostatitis. JAMA 1999, 282: 236–7.
Comhaire F, Verschraegen G, Vermeulen L. Diagnosis of accessory gland infection and its possible role in male infertility. Int J Androl 1980, 3: 32–45.
Andreessen R, Sudhoff F, Borgmann V, Nagel R. Results of ofloxacin therapy in andrologic patients suffering from therapy-requiring asymptomatic infections. Andrologia 1993, 25: 377–83.
Diemer T, Hales DB, Weidner W. Immune-endocrine interactions and Leydig cell function: the role of cytokines. Andrologia 2003, 35: 55–63.
Vicari E, La Vignera S, Arancio A, et al. Male accessory gland infections and infertility. In: Colpi GM ed. Male infertility today. 2004, 4: 139–51.
Li HJ, Xu P, Liu JS, et al. Prevalence of chronic prostatitis and its effects on male infertility. Zhongua Yi Xue Za Zhi 2001, 84: 369–71.
Vicari E. Seminal leukocyte concentration and related specific reactive oxygen species production in patients with male accessory gland infections. Hum Reprod 1999, 14: 2025–30.
Vicari E. Effectiveness and limits of antimicrobial treatment on seminal leukocyte concentration and related reactive oxygen species production in patients with male accessory gland infection. Hum Reprod 2000, 15: 536–44.
Vicari E, La Vignera S, Castiglione R, Calogero AE. Sperm parameter abnormalities, low seminal fructose and reactive oxygen species overproduction do not discriminate patients with unilateral or bilateral post-infectious inflammatory prostato-vesiculo-epididymitis. J Endocrinol Invest 2006, 29: 18–25.
La Vignera S, Arancio A, Calogero AE, Condorelli R, Koverech A, Vicari E. Male Accessory Gland Infections (MAGI): patient questionnaire and additional ultrasonography criteria. Minerva Med 2008, 99: 421–30.
La Vignera S, Calogero AE, Condorelli R, et al. Ultrasonographic e-valuation of patients with male accessory gland infection. Andrologia 2011, Sep 15 [Epub ahead of print]; doi: 10.1111/j.1439-0272.2010.01132.x.
Sakamoto H, Ogawa Y, Yoshida H. Relationship between testicular volume and testicular function: comparison of the Prader orchidometric and ultrasonographic measurement in patients with infertility. Asian J Androl 2008, 10: 319–24.
Littrup PJ, Williams CR, Egglin TK, Kane RA. Determination of prostate volume with transrectal US for cancer screening. Part II. Accuracy of in vitro and in vivo techniques. Radiology 1991; 179: 49–53.
Terasaki T, Watanabe H, Kamoi K, Naya Y. Seminal vesicle parameters at 10-year intervals measured by transrectal ultrasonography. J Urol 1993, 150: 914–6.
World Health Organization. WHO laboratory manual for the examination of human semen and semen-cervical mucus interaction, 4th ed. Cambridge: Cambridge University Press 1999.
La Vignera S, Calogero AE, Arancio A, et al. Transrectal ultrasonography in infertile patients with persistently elevated bacte-riospermia. Asian J Androl 2008, 10: 731–40.
Vicari E. Seminal leukocyte concentration and related specific reactive oxygen species production in patients with male accessory gland infections. Hum Reprod 1999, 14: 2025–30.
Hendrikx AJ, de la Rosette JJ, van Helvoort-van Dommelen CA, et al. Histological analysis of ultrasonic images of the prostate: an accurate technique. Ultrasound Med Biol 1990, 16: 667–74.
Lotti F, Corona G, Mancini M, et al. Ultrasonographic and clinical correlates of seminal plasma interleukin-8 levels in patients attending an andrology clinic for infertility. Int J Androl 2010, 34: 600–13.
Zahalsky M, Nagler HM. Ultrasound and infertility: diagnostic and therapeutic uses. Curr Urol Rep 2001, 2: 437–42.
Pavlica P, Barozzi L. Imaging of the acute scrotum. Eur Radiol 2001, 11: 220–8.
Bushby LH, Miller FN, Rosairo S, Clarke JL, Sidhu PS. Scrotal calcification: ultrasound appearances, distribution and aetiology. Br J Radiol 2002, 75: 283–8.
Dogra VS, Gottlieb RH, Oka M, Rubens DJ. Sonography of the scrotum. Radiology 2003, 227: 18–36.
Behre HM, Kliesch S, Schädel F, Nieschlag E. Clinical relevance of scrotal and transrectal ultrasonography in andrological patients. Int J Androl 18(Suppl) 1995, 2: 27–31.
Purvis K, Christiansen E. Infection in the male reproductive tract. Impact, diagnosis and treatment in relation to male infertility. Int J Androl 1993, 16: 1–13.
Kim ED, Lipshultz LI. Role of ultrasound in the assessment of male infertility. J Clin Ultrasound 1996, 24: 437–53.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
La Vignera, S., Vicari, E., Condorelli, R. et al. Hypertrophic-congestive and fibro-sclerotic ultrasound variants of male accessory gland infection have different sperm output. J Endocrinol Invest 34, e330–e335 (2011). https://doi.org/10.1007/BF03346729
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03346729