Abstract
Introduction
Suicide attempt is a common cause for major trauma. Due to the underlying psychiatric disease, patients` compliance or even prognosis may be reduced. Modalities of discharge after surgical acute care might differ.
Methods
Retrospective study including trauma patients of two urban level 1 trauma centers between 2013 and 2017. Data originally collected for quality management using the German trauma registry were supplemented after review of medical charts with details on psychiatric disease and discharge modalities.
Results
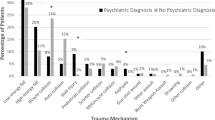
We included 2118 consecutive patients of which 108 (5%) attempted suicide. Most common psychiatric diagnosis were depression (38%) and schizophrenia (25.9%). Comparing patients after suicide attempt with others, suicide attempt was associated with a younger age (42.3 vs. 49.0 years), a higher injury severity (mean ISS 24.7 vs. 16.8) and consecutively, a higher expected mortality (risk-adjusted prognosis for mortality 18.0 vs. 8.1%), while observed mortality was lower than expected in both groups (16.7 vs. 6.4%). Survivors after suicide attempt had a longer stay on ICU (mean days on ICU 17 vs. 7). 56% were transferred to psychiatric facilities and only 4% could be discharged home after acute surgical care.
Conclusion
Incidence of suicide attempts among major trauma patients is high. Mean injury severity is higher than in unintended trauma and associated with a prolonged stay on intensive care unit even after adjustment for injury severity and age. Risk-adjusted mortality is not increased. Proportion of patients discharged home or to out-patient rehabilitation is very low. Specialized institutions who offer both, musculoskeletal rehabilitation and psychiatric care are required for rehabilitative treatment after the acute surgical care.
Similar content being viewed by others
Availability of data and materials
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Publ Health. 2000;90(4):523–6. https://doi.org/10.2105/ajph.90.4.523.
Bjorkenstam E, Bjorkenstam C, Holm H, Gerdin B, Ekselius L. Excess cause-specific mortality in in-patient-treated individuals with personality disorder: 25-year nationwide population-based study. Br J Psychiatry. 2015;207(4):339–45. https://doi.org/10.1192/bjp.bp.114.149583.
Huang Y, Kotov R, de Girolamo G, Preti A, Angermeyer M, Benjet C, et al. DSM-IV personality disorders in the WHO World Mental Health Surveys. Br J Psychiatry. 2009;195(1):46–53. https://doi.org/10.1192/bjp.bp.108.058552.
Bjorkenstam C, Bjorkenstam E, Gerdin B, Ekselius L. Excess cause-specific mortality in out-patients with personality disorder. BJPsych Open. 2015;1(1):54–5. https://doi.org/10.1192/bjpo.bp.115.000356.
Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. https://doi.org/10.1192/bjp.173.1.11.
Topp T, Lefering R, Mueller T, Ruchholtz S, Patzer T, Kuhne CA, et al. Suicide in old age: the underestimated risk. An analysis of 1894 patients in the Trauma Registry of the German Trauma Society. Unfallchirurg. 2013;116(4):332–7. https://doi.org/10.1007/s00113-011-2109-4.
Clous EA, Beerthuizen KC, Ponsen KJ, Luitse JSK, Olff M, Goslings JC. Trauma and psychiatric disorders: a systematic review. J Trauma Acute Care Surg. 2017;82(4):794–801. https://doi.org/10.1097/TA.0000000000001371.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU: the revised injury severity classification, version II. Crit Care. 2014;18(5):476. https://doi.org/10.1186/s13054-014-0476-2.
Lefering R, Huber-Wagner S, Bouillon B, Lawrence T, Lecky F, Bouamra O. Cross-validation of two prognostic trauma scores in severely injured patients. Eur J Trauma Emerg Surg. 2020. https://doi.org/10.1007/s00068-020-01373-6.
Lai CY, Maegele M, Yeung JHH, Lefering R, Hung KCK, Chan PSL, et al. Major trauma care in Hong Kong and Germany: a trauma registry data benchmark study. Eur J Trauma Emerg Surg. 2020. https://doi.org/10.1007/s00068-020-01311-6.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4. https://doi.org/10.1016/s0140-6736(75)92830-5.
Keats AS. The ASA classification of physical status–a recapitulation. Anesthesiology. 1978;49(4):233–6.
Bennett KM, Vaslef SN, Shapiro ML, Brooks KR, Scarborough JE. Does intent matter? The medical and societal burden of self-inflicted injury. J Trauma. 2009;67(4):841–7. https://doi.org/10.1097/TA.0b013e3181b24cd3.
David JS, Gelas-Dore B, Inaba K, Levrat A, Riou B, Gueugniaud PY, et al. Are patients with self-inflicted injuries more likely to die? J Trauma. 2007;62(6):1495–500. https://doi.org/10.1097/01.ta.0000250495.77266.7f.
Varley J, Pilcher D, Butt W, Cameron P. Self harm is an independent predictor of mortality in trauma and burns patients admitted to ICU. Injury. 2012;43(9):1562–5. https://doi.org/10.1016/j.injury.2011.06.005.
Aufmkolk M, Voggenreiter G, Majetschak M, Neudeck F, Schmit-Neuerburg KP, Obertacke U. Injuries due to falls from a great height. A comparative analysis of injuries and their outcome following suicide-related and accidental falls. Unfallchirurg. 1999;102(7):525–30. https://doi.org/10.1007/s001130050445.
Ruchholtz S, Nast-Kolb D, Waydhas C, Schweiberer L. The injury pattern in polytrauma. Value of information regarding accident process in clinical acute management. Unfallchirurg. 1996;99(9):633–41. https://doi.org/10.1007/s001130050036.
Dickinson A, Roberts M, Kumar A, Weaver A, Lockey DJ. Falls from height: injury and mortality. J R Army Med Corps. 2012;158(2):123–7. https://doi.org/10.1136/jramc-158-02-11.
Wong TH, Nguyen HV, Chiu MT, Chow KY, Ong ME, Lim GH, et al. The low fall as a surrogate marker of frailty predicts long-term mortality in older trauma patients. PLoS ONE. 2015;10(9):e0137127. https://doi.org/10.1371/journal.pone.0137127.
Goldman-Mellor SJ, Caspi A, Harrington H, Hogan S, Nada-Raja S, Poulton R, et al. Suicide attempt in young people: a signal for long-term health care and social needs. JAMA Psychiatry. 2014;71(2):119–27. https://doi.org/10.1001/jamapsychiatry.2013.2803.
Acknowledgements
A part of the study results has been presented in 2019 at the German Interdisciplinary Association for Intensive Care and Emergency Medicine (DIVI) annual congress in Hamburg, Germany.
Author information
Authors and Affiliations
Contributions
AN, UH, were equally responsible for the writing of the manuscript. AN and UH conducted the statistical analysis. AN, UH, OK, TO, CW, MD, TAS participated in the study design and conduct and assisted in the writing of the manuscript. Each author made substantial contributions to the conception or design of the work, the acquisition, analysis or interpretation of data, and drafting and final approval of the manuscript. All authors read and approved and read the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Consent for publication
We obtained consent for publication of de-identified data
Rights and permissions
About this article
Cite this article
Nohl, A., Ohmann, T., Kamp, O. et al. Major trauma due to suicide attempt: increased workload but not mortality. Eur J Trauma Emerg Surg 48, 519–523 (2022). https://doi.org/10.1007/s00068-020-01436-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01436-8