Abstract
Aims/hypothesis
Obesity and diabetes are associated with increased intracellular p38 mitogen-activated protein kinase (MAPK) signalling, which may promote tissue inflammation and injury. Activation of p38 MAPK can be induced by either of the immediate upstream kinases, MAP kinase kinase (MKK)3 or MKK6, and recent evidence suggests that MKK3 has non-redundant roles in the pathology attributed to p38 MAPK activation. Therefore, this study examined whether MKK3 signalling influences the development of obesity, type 2 diabetes and diabetic nephropathy.
Methods
Wild-type and Mkk3 (also known as Map2k3) gene-deficient db/db mice were assessed for the development of obesity, type 2 diabetes and renal injury from 8 to 32 weeks of age.
Results
Mkk3 +/+ db/db and Mkk3 −/− db/db mice developed comparable obesity and were similar in terms of incidence and severity of type 2 diabetes. At 32 weeks, diabetic Mkk3 +/+ db/db mice had increased kidney levels of phospho-p38 and MKK3 protein. In comparison, kidney levels of phospho-p38 in diabetic Mkk3 −/− db/db mice remained normal, despite a fourfold compensatory increase in MKK6 protein levels. The reduced levels of p38 MAPK signalling in the diabetic kidneys of Mkk3 −/− db/db mice was associated with protection against the following: declining renal function, increasing albuminuria, renal hypertrophy, podocyte loss, mesangial cell activation and glomerular fibrosis. Diabetic Mkk3 −/− db/db mice were also significantly protected from tubular injury and interstitial fibrosis, which was associated with reduced Ccl2 mRNA expression and interstitial macrophage accumulation.
Conclusions/interpretation
MKK3–p38 MAPK signalling is not required for the development of obesity or type 2 diabetes, but plays a distinct pathogenic role in the progression of diabetic nephropathy in db/db mice.
Similar content being viewed by others
Introduction
Inflammation and cellular dysfunction are features of obesity, diabetes and diabetic nephropathy, which are associated with intracellular activation of mitogen-activated protein kinase (MAPK) signalling pathways. Components of the diabetic milieu, including hyperglycaemia, hyperlipidaemia, hyperinsulinaemia, reactive oxygen species, AGE, angiotensin II and proinflammatory cytokines, can stimulate increased MAPK signalling in cells and may thereby promote tissue injury [1].
p38 MAPK signalling is known to promote inflammatory and profibrotic responses and has been associated with other cellular functions such as glucose uptake, cell differentiation, apoptosis and proliferation [2–4]. Levels of activated p38 are elevated in the skeletal muscle, adipose tissue and kidneys of diabetic patients [5–7], suggesting that some p38 responses may be important for the pathogenesis of diabetes and its complications. Functional blocking studies in animal models have demonstrated that p38 signalling induces the inflammation in insulitis and diabetic cardiomyopathy [8, 9]. Furthermore, in vitro experiments have shown that p38 inhibition can suppress adipogenesis, prevent insulin resistance in myotubes exposed to TNF-α or oxidative stress and stimulate glucose transport in adipocytes [10, 11]; however, these findings remain controversial.
Clinical studies have demonstrated that kidney p38 activity is increased and associated with the development of diabetic nephropathy [5, 12]. Renal biopsies from patients with established type 2 diabetes display prominent p38 signalling despite treatment with angiotensin system inhibitors [5]. In comparison, animal models of diabetes have shown that p38 activation rapidly increases in glomeruli and tubules in response to hyperglycaemia and occurs in the accumulating kidney interstitial cells associated with advanced nephropathy. Pharmacological blockade of p38 is known to suppress the development of inflammation and fibrosis in acute kidney disease [13, 14]. These mechanisms are also important in the progression of diabetic renal injury, suggesting that diabetic nephropathy may also be suppressed by inhibiting p38 signalling.
In vitro studies have identified specific kidney cells and mechanisms of renal injury that may be affected by p38 signalling during diabetes. Exposure to high glucose activates p38 in human mesangial cells [15], mouse podocytes [16] and rat proximal tubular cells [17]. Similarly, glycated albumin can stimulate p38 phosphorylation in cultured fibroblasts [18]. Activation of p38 induces apoptosis of rat mesangial cells exposed to methylglyoxal [19] and apoptosis of mouse podocytes following stimulation with TGF-β [20] and AGE [21, 22]. In addition, p38 signalling can contribute to proinflammatory and profibrotic responses. Activation of p38 enhances production of monocyte chemoattractant protein-1 (MCP-1) by vascular endothelial cells [23], induces local angiotensinogen production in rat tubular cells [17], stimulates both TGF-β-induced fibronectin accumulation in renal interstitial fibroblasts [24] and collagen production in mouse mesangial cells [25], increases Tgf-β1 (also known as Tgfb1) expression in renal tubular cells [26] and promotes synthesis of vascular endothelial growth factor induced by angiotensin II [27, 28]. Studies have also shown that p38 signalling mediates both tubular hypertrophy induced by high glucose [26] and transactivation of the epidermal growth factor receptor required for dedifferentiation of proximal tubular epithelial cells following oxidant injury [29].
Functional blocking studies are required to determine the role of p38 signalling in diabetes and its complications. One strategy for achieving this goal is to perform studies of diabetes in a mouse strain that is genetically deficient in one of the immediate upstream kinases (MAP kinase kinase [MKK]3 or MKK6) that regulate p38 signalling. These protein kinases provide a parallel and independent mechanism of phosphorylating p38 but their relative contribution to the increased p38 activity associated with diabetic nephropathy is unknown. Genetically modified Mkk3 −/− and Mkk6 −/− mice are viable and fertile, and provide an opportunity to study the role of p38 signalling in models of disease. Of these two kinases, MKK3 appears to be the most attractive target for studies of genetic deletion, because MKK3–p38 signalling has been shown to be non-redundant in some pathological processes [30, 31]. Furthermore, mouse studies have shown that Mkk3 deficiency is protective in models of passive arthritis and streptozotocin-induced pancreatic inflammation [32, 33].
In the current study, Mkk3-deficient db/db mice were created and used to examine the role of MKK3–p38 signalling in the development of obesity, hyperglycaemia and nephropathy in the db/db model of type 2 diabetes.
Methods
Animal model
Obese (db/db) and lean db/+ heterozygote control mice were created by breeding pairs of C57BL/6 db/+ mice obtained from Jackson Laboratories (Bar Harbor, ME, USA) and were genotyped for the mutated leptin receptor. Mkk3 −/− mice [34] were back-crossed for eight generations on to the C57BL/6 strain and bred at Monash Medical Centre (Clayton, VIC, Australia). Mkk3 −/− mice were then crossed with C57BL/6 db/+ mice to create Mkk3 −/− db/+ mice, which were validated by genotyping. The latter were then interbred to create Mkk3 −/− db/db mice. Only males were used for the study due to the higher incidence of diabetes. Mice were maintained on a normal diet under standard animal housing conditions.
The development of obesity and diabetes was examined in groups of Mkk3 +/+ and Mkk3 −/− db/db mice (n = 33–40) between 8 and 32 weeks of age, with monthly assessment of weight and blood glucose (Medisense glucometer; Abbott Laboratories, Bedford, MA, USA). Insulin and glucose tolerance tests (described below) were performed at 8 and 32 weeks. Subgroups of the Mkk3 +/+ and Mkk3 −/− db/db mice (n = 10), which showed equivalent levels of diabetes from 12 to 32 weeks, were used to examine the development of diabetic nephropathy and kidney p38 signalling. The urine albumin excretion rate was measured at 8, 16, 24 and 32 weeks. Renal function was determined at 32 weeks. Groups of age-matched non-diabetic Mkk3 +/+ and Mkk3 −/− db/+ mice (n = 8–10) were also studied as controls. Mice were killed at 32 weeks and selected organs (liver, kidneys and epidydimal fat) were examined. Tissues were fixed in 4% (vol./vol.) neutral-buffered formalin or 2% (wt/vol.) paraformaldehyde–lysine–periodate (PLP) or were snap-frozen.
Approval for these studies was obtained from the Monash Medical Centre Animal Ethics Committee in accordance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes, 7th edition (2004).
Glucose and insulin tolerance tests
To test glucose tolerance, mice were given an intraperitoneal injection of d-glucose (1 g/kg) after a 12 h fast. For insulin tolerance, mice were injected with human insulin (2 U/kg; Actrapid, Novo Nordisk, Bagsvaerd, Denmark) after a 6 h fast. The tolerance profiles were assessed by measuring blood glucose at 0, 30, 60, 90 and 120 min, using the glucose oxidase method.
Biochemical analysis
Urine was collected from mice housed in metabolism cages for 18 h. Whole blood was collected by cardiac puncture in anaesthetised mice, centrifuged (800 g, 10 min) and stored as serum or heparinised plasma. ELISA kits were used to measure urine albumin (Bethyl Laboratories, Montgomery, TX, USA) and plasma insulin (Linco Research, St Charles, MO, USA). Serum NEFA were assessed by a colorimetric assay kit (Wako Pure Chemical Industries, Osaka, Japan). HbA1c was measured by HPLC in the Biochemistry Department at the Monash Medical Centre. Serum and urine creatinine were determined by HPLC and used to calculate creatinine clearance.
Histopathology analysis
Formalin-fixed sections (2 μm) were stained with periodic acid–Schiff’s reagent to assess structure and counterstained with haematoxylin to identify nuclei. Glomerular volume and matrix fraction were assessed by computer image analysis (Image-Pro Plus; Media Cybernetics, Silver Spring, MD, USA) and cellularity was assessed by counting nuclei in 20 hilar glomerular cross-sections (gcs) per animal. Tubular atrophy was assessed by counting injured (dilated, atrophied, necrotic) tubular cross-sections (tcs) in ten cortical fields (magnification: ×250) as a percentage of total tcs. Interstitial volume was assessed by point-counting in 20 fields (magnification: ×400). Staining for collagen was performed by immersing sections (4 μm) in 1% (wt/vol.) Picro-sirius red (Sirius Red; Sigma-Aldrich, St Louis, MO, USA) for 1 h and differentiating with 0.5% (vol./vol.) glacial acetic acid. Glomerular (20 hilar gcs) and interstitial staining (20 cortical fields, magnification: ×250, excluding blood vessels) were assessed by computer image analysis, as a percentage of area stained. All scoring was performed on blinded slides.
Antibodies
The following primary antibodies were used in this study: rabbit anti-phospho (p)-p38 MAPK (Thr180/Tyr182), rabbit anti-phospho-MKK3/phospho-MKK6 (Ser189/207) and rabbit anti-cleaved caspase 3 (ASP175) (Cell Signaling, Beverly, MA, USA); mouse anti-p38α (Upstate Biotechnology, Lake Placid, NY, USA); rabbit anti-MKK3, goat anti-MKK6 and rabbit anti-Wilm’s tumour (WT) antigen 1 (C-19) (Santa Cruz Biotechnology, Santa Cruz, CA, USA); rabbit anti-tubulin (Abcam, Cambridge, UK); mouse anti-α-smooth muscle actin (SMA) (1A4; Sigma-Aldrich); rat anti-mouse Ki67 (TEC-3; Dako, Carpinteria, CA, USA); and rat-anti CD68 (FA-11; Serotec, Oxford, UK).
Immunohistochemistry
Immunostaining for phospho-p38, cleaved caspase-3, WT1 and Ki67 was performed on 4 μm formalin-fixed paraffin-embedded sections. Immunostaining for CD68 was performed on 5 μm PLP-fixed cryostat sections. For antigen retrieval (phospho-p38, cleaved caspase-3, WT1 and Ki67), dewaxed paraffin sections were heated in a microwave oven (800 W, 12 min) or pressure cooker (HIGH setting 20 min, full pressure 5 min) in 10 mmol/l sodium citrate buffer (pH 6.0). After cooling, sections were treated with 20% (vol./vol.) sheep serum or 20% (vol./vol.) rabbit serum for 30 min and then incubated overnight at 4°C with primary antibody in 3% (wt/vol.) BSA. Sections were then placed in 0.6% (vol./vol.) hydrogen peroxide in methanol for 20 min to inactivate endogenous peroxidase. For detection of α-SMA antibody, sections were incubated with peroxidase-conjugated sheep anti-mouse IgG (Dako), followed by mouse peroxidase-conjugated anti-peroxidase complexes (Dako). All other primary antibodies were detected using a standard ABC-peroxidase system: avidin–biotin block, biotinylated antibodies (sheep anti-rabbit or rabbit anti-rat IgG) and ABC-peroxidase (Vector Laboratories, Burlingame, CA, USA). Sections were developed with 3,3-diaminobenzidine (Sigma) to produce a brown colour. CD68 sections were counterstained with haematoxylin to assist cell counting. Normal rabbit and goat serum or isotyped-matched irrelevant IgGs were used as negative controls.
Quantification of immunohistochemistry
The number of phospho-p38-, WT1-, Ki67- and CD68-positive cells was counted in 20 hilar gcs per animal (magnification: ×400). The number of phospho-p38-positive tubules (>50% nuclei stained) was counted in 20 cortical fields (magnification: ×250) and expressed as a percentage of total tcs. Interstitial phospho-p38-positive and CD68-positive cells were counted in 50 cortical fields (magnification: ×400) and expressed as cells/mm2. Cleaved caspase-3-positive tubular cells were counted in the entire kidney cortex and expressed as cells/mm2. Cleaved caspase-3-positive glomerular cells were extremely rare and therefore not assessed. α-SMA staining was quantified by computer image analysis in 20 hilar gcs (magnification: ×400) and 20 cortical fields (magnification: ×250), and expressed as the percentage of area stained.
Western blotting
Frozen kidney samples were homogenised in lysis buffer (pH 7.2) containing 8.1 mmol/l Na2HPO4, 1.5 mmol/l KH2PO4, 135 mmol/l NaCl, 2.7 mmol/l KCl, 1.0 mmol/l EDTA, 5 mmol/l NaF, 6 mol/l urea, 0.5% (vol./vol.) Triton-X-100, 1.0 mmol/l Na3VO4, 20 mmol/l sodium pyrophosphate, 25 μg/ml leupeptin, 3 μg/ml aprotinin, 100 μmol/l phenylmethylsulfonyl fluoride and 1% (vol./vol.) phosphatase inhibitor cocktail (Sigma-Aldrich). Samples were separated on a 4–20% (wt/vol.) SDS-PAGE gel and electro-transferred on to nitrocellulose membranes. Membranes were then blocked for 1 h with Odyssey blocking buffer (LICOR, Lincoln, NE, USA) and incubated overnight at 4°C with primary antibody in Odyssey buffer. Blots were then washed with Tris-buffered saline/0.1% (vol./vol.) Tween-20 and incubated for 1 h with secondary antibody (goat anti-rabbit or donkey anti-goat Alexa Fluor 680 [Invitrogen, Carlsbad, CA, USA]; or donkey anti-mouse IRDye 800 [Rockland, Gilbertsville, PA, USA]). After washing, protein bands were detected using the Odyssey Infrared Image Detection system (LICOR). α-Tubulin was used as a loading control. After detection of phospho-p38 and tubulin at 680 nm, blots were reprobed for p38α at 800 nm. Densitometry analysis was performed using Gel-pro Analyzer 3.0 software (Media Cybernetics). Results are expressed as the integrated optical density relative to tubulin.
Real-time RT-PCR
Total RNA was extracted from whole-kidney samples using the RiboPure reagent (Ambion, Austin, TX, USA) and reverse-transcribed using a kit (Superscript First-Strand Synthesis kit; Invitrogen) with random primers. Real-time PCR was performed using the Rotor-Gene 3000 system (Corbett Research, Sydney, NSW, Australia) with thermal cycling conditions of 37°C for 10 min, 95°C for 5 min, followed by 50 cycles of 95°C for 15 s, 60°C for 20 s and 68°C for 20 s. The primer pairs and carboxyfluorescein-labelled minor groove binder probes used were: Tnf-α (also known as Tnf) (forward: GGC TGC CCC GAC TAC GT; reverse: TTT CTC CTG GTA TGA GAT AGC AAA TC; probe: TCA CCC ACA CCG TCA G); Ccl2 (forward: GAC CCG TAA ATC TGA AGC TAA; reverse: CAC ACT GGT CAC TCC TAC AGA A; probe: ACA ACC ACC TCA AGC AC); and Tgf-ß1 (forward: GGA CAC ACA GTA CAG CAA; reverse: GAC CCA CGT AGT AGA CGA T; probe: ACA ACC AAC ACA ACC C). The relative amount of mRNA was calculated using comparative Ct (ΔΔCt) method. All specific amplicons were normalised against 18S rRNA, which was amplified in the same reaction as an internal control using commercial assay reagents (Applied Biosystems, Scoresby, VIC, Australia).
Statistical analysis
Statistical differences were analysed by either the unpaired Student’s t test or one way ANOVA with Tukey’s multiple comparison post-test. Correlations were performed using Pearson’s correlation coefficient. Data were recorded as mean ± SEM with p < 0.05 considered significant. All analyses were performed using GraphPad Prism 5.0 (GraphPad, San Diego, CA, USA).
Results
Mkk3 deletion does not affect obesity or type 2 diabetes in db/db mice
Between the age of 8 and 32 weeks, Mkk3 +/+ db/db and Mkk3 −/− db/db mice developed comparable obesity and were 50% heavier than control db/+ mice at 32 weeks (Fig. 1a). The incidence of diabetes (non-fasting blood glucose >16 mmol/l) was similar in Mkk3 +/+ db/db and Mkk3 −/− db/db mice, reaching approximately 50% at 32 weeks (Fig. 1b). In addition, both db/db genotypes showed an equivalent impairment of glucose and insulin tolerance compared with db/+ mice at 8 and 32 weeks (Fig. 1c–f). Mkk3 −/− db/db mice showed less hepatomegaly than Mkk3 +/+ db/db mice at 32 weeks, but there was no significant difference in epididymal fat weight, plasma insulin or serum NEFA (Table 1).
Effect of MKK3 deficiency on obesity and type 2 diabetes. Serial measurements from 8 to 32 weeks of age show the development of a an equivalent obesity profile between Mkk3 +/+ db/db (upright triangles) and Mkk3 −/− db/db mice (inverted triangles), which were 50% bigger than control db/+ mice (circles) at 32 weeks, and b a similar incidence of diabetes between Mkk3 +/+ db/db (solid line) and Mkk3 −/− db/db mice (dotted line) of 50% by 32 weeks. Glucose tolerance and insulin sensitivity tests performed at week 8 (c, d) and week 32 (e, f) show a similar progression of glucose intolerance and insulin resistance in Mkk3 +/+ db/db mice (upright triangles) and Mkk3 −/− db/db (inverted triangles) compared with control db/+ mice (circles). Data are means ± SEM; n = 33–40. a p < 0.001 for db/db vs db/+ mice; b p < 0.05 for Mkk3 −/− db/db vs Mkk3 +/+ db/db mice
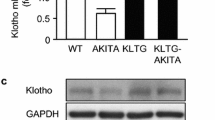
Mkk3 deficiency reduces p38 MAPK activation in diabetic kidneys
Diabetic Mkk3 +/+ and Mkk3 −/− db/db mice selected for analysis of nephropathy had equivalent obesity (53.3 ± 2.8 vs 58.5 ± 1.9 g), fasting blood glucose profile and HbA1c levels (Fig. 2). At 32 weeks, diabetic Mkk3 +/+ db/db mice had increased kidney levels of phospho-p38, whereas the levels in diabetic Mkk3 −/− db/db mice were not different from db/+ controls (Fig. 3a,b). Similarly, the kidney levels of phospho-MKK3/6 were elevated in diabetic Mkk3 +/+ db/db mice at 32 weeks, whereas diabetic Mkk3 −/− db/db mice showed a trend towards reduced levels of phospho-MKK3/6, which did not reach statistical significance (Fig. 3a,c). Diabetic Mkk3 +/+ db/db mice had a threefold increase in kidney levels of MKK3 protein, but no change in MKK6 protein levels compared with db/+ mice. Deficiency of Mkk3 resulted in a compensatory increase in MKK6 protein levels in db/+ and db/db mice compared with wild-type controls (Fig. 3d,e). This compensatory increase in kidney MKK6 protein levels did not increase kidney levels of phospho-p38 in the diabetic Mkk3 −/− db/db mice.
Equivalent levels of hyperglycaemia in selected db/db mice. Diabetic db/db mice that were selected for analysis of kidney p38 activation and nephropathy had a similar fasting blood glucose profile, which showed a progressive increase of glycaemia from 8 to 32 weeks (a) and the equivalence between the two groups in hyperglycaemia was confirmed by HbA1c measurement at 32 weeks (b). Triangles, Mkk3 +/+ db/db; inverted triangles, Mkk3 −/− db/db; circles, control db/+. Data are means ± SEM; n = 10. a p < 0.001 for db/db vs db/+ mice. The dashed horizontal line represents the threshold level of blood glucose above which mice are considered diabetic
Western blotting analysis of kidney p38 pathway activation. a Representative western blots showing protein bands of MKK3, MKK6 and p38, along with their associated phosphorylated protein bands. α-Tubulin was used as the loading control. b Quantification of phospho-p38 by densitometry showed a 35% reduction in kidney p38 phosphorylation in Mkk3 −/− db/db compared with Mkk3 +/+ db/db mice. c Combined phospho-MKK3/6 protein increased in diabetes, but remained similar in both Mkk3 genotypes of db/db mice, indicating high levels of MKK6 phosphorylation. d MKK3 protein bands were absent in Mkk3 −/− mice, but MKK3 was significantly increased in db/db compared with db/+ Mkk3 +/+ mice. e A compensatory increase in MKK6 was observed in Mkk3 −/− mice, but diabetes as such was not associated with a significantly elevated MKK6 level. Data are means ± SEM; n = 10. Comparisons were made by one way ANOVA (a–c, e) and t test (d). a p < 0.05, b p < 0.01 vs Mkk3 +/+ db/+ mice; c p < 0.05, d p < 0.01 vs Mkk3 +/+ db/db mice
Immunostaining of normal db/+ mouse kidneys identified phospho-p38 in glomerular podocytes and collecting ducts (Fig. 4). In diabetic Mkk3 +/+ db/db mice, the number of phospho-p38-positive cells was significantly increased in the glomeruli, tubules and the interstitium compared with non-diabetic db/+ controls (Fig. 4). The major sources of additional kidney phospho-p38 staining were dilated tubules, interstitial myofibroblasts and mesangial cells. At 32 weeks, diabetic Mkk3 −/− db/db mice had 50% less phospho-p38-positive cells in glomeruli and tubules than diabetic Mkk3 +/+ db/db mice (Fig. 4), which is consistent with the western blot analysis of phospho-p38 in the total kidney.
Phospho-p38 immunohistochemistry. Immunostaining for phospho-p38 in the db/+ kidney demonstrated normal phospho-p38 staining in the occasional podocyte and collecting ducts (a, d). In the Mkk3 +/+ db/db kidney, there was a twofold increase in glomerular and tubular staining for phospho-p38, particularly within the mesangium and dilated tubules (b, e, g, h). In the Mkk3 −/− db/db kidney, the increased glomerular and tubular phospho-p38-positive cells were reduced by 50% (c, f, g, h). Magnification: a–c ×400; d–f ×160. Data are means ± SEM; n = 10. a p < 0.05, b p < 0.01, c p < 0.001 vs db/+ mice; d p < 0.05, e p < 0.01 vs Mkk3 +/+ db/db mice
Mkk3 deficiency reduces albuminuria and preserves renal function in db/db mice
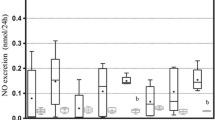
The urine albumin excretion of db/+ mice remained stable at 5 mg/mmol creatinine between 8 and 32 weeks. In comparison, the urine albumin:creatinine ratio increased progressively in diabetic Mkk3 +/+ db/db mice and was 11-fold higher than in db/+ counterparts at 32 weeks. This increase in the urine albumin:creatinine ratio was reduced by 70% in Mkk3 −/− db/db mice at 32 weeks (Fig. 5a). Furthermore, at 32 weeks, a decline in creatinine clearance was seen in diabetic Mkk3 +/+ db/db mice compared with db/+ mice; however, renal function was protected in the diabetic Mkk3 −/− db/db mice (Fig. 5b).
Urinary albumin excretion and renal function. a Serial measurements of the albumin:creatinine ratio (ACR) from 8 to 32 weeks demonstrated a static ACR of around 5 mg/mmol in control db/+ mice (circles). The ACR progressively increased in Mkk3 +/+ db/db mice (upright triangles) and was 11-fold greater than normal by 32 weeks. In contrast, the rise in ACR was significantly attenuated in Mkk3 −/− db/db mice (inverted triangles). b Creatinine clearance (CrCl) was reduced in Mkk3 +/+ db/db mice compared with db/+ mice, but this loss of renal function was abolished in Mkk3 −/− db/db mice. Data are means ± SEM; n = 10. a p < 0.05, b p < 0.001 for db/db vs db/+ mice; c p < 0.05, d p < 0.001 for Mkk3 −/− db/db vs Mkk3 +/+ db/db mice
Mkk3 deficiency reduces renal injury in diabetic db/db mice
Wild-type Mkk3 +/+ db/db mice developed significant glomerular lesions at 32 weeks, which included glomerular hypertrophy, hypercellularity, increased mesangial matrix and collagen deposition. In comparison, Mkk3 −/− db/db mice had similar glomerular hypertrophy and hypercellularity, but showed significant reductions in renal hypertrophy, glomerular matrix and collagen levels (Table 2). Immunostaining for WT1 demonstrated significant podocyte depletion in diabetic Mkk3 +/+ db/db mice compared with db/+ mice, which was partially attenuated in diabetic Mkk3 −/− db/db mice (Fig. 6). Podocyte numbers correlated inversely with the urine albumin:creatinine ratio associated with diabetes (r = −0.65, p = 0.0002). Mesangial immunostaining of α-SMA, a marker of mesangial cell activation, was increased in Mkk3 +/+ db/db compared with db/+ mice; however, this response was reduced in Mkk3 −/− db/db mice (Fig. 6).
Effect of Mkk3 deficiency on podocyte depletion and mesangial cell activation. WT1 immunostaining for podocytes in control db/+ (a), Mkk3 +/+ db/db (b) and Mkk3 −/− db/db mice (c) demonstrated a marked reduction in podocyte numbers in Mkk3 +/+ diabetic mice, which was better preserved in Mkk3 −/− diabetic mice (g). Immunostaining for α-SMA as a marker of mesangial cell activation in db/+ mice (d), Mkk3 +/+ db/db mice (e) and Mkk3 −/− db/db mice (f) demonstrated a small amount of age-related α-SMA in db/+ mice, which was dramatically increased in Mkk3 +/+ db/db mice and attenuated in Mkk3 −/− db/db mice. Magnification: a–c ×1,000; d–f ×400. Data are means ± SEM; n = 10. a p < 0.01, b p < 0.001 vs db/+ mice; c p < 0.05, d p < 0.001 vs Mkk3 +/+ db/db mice
Significant tubulointerstitial lesions were also found in Mkk3 +/+ db/db mice at 32 weeks. These included tubular atrophy, tubular cell apoptosis, increased interstitial volume, accumulation of α-SMA-positive myofibroblasts and enhanced collagen deposition (Table 2, Fig. 7). Tubular cell proliferation, an index of the response to tubular damage, was also increased in these diabetic kidneys (Table 2). In comparison, all measured markers of tubular injury and tubulointerstitial collagen deposition were significantly reduced in diabetic Mkk3 −/− db/db mice (Table 2). There was also a trend towards reduced interstitial myofibroblast accumulation in db/db mice lacking Mkk3; however, this was not statistically significant.
Tubulo-interstitial injury is reduced by Mkk3 deficiency. Periodic acid–Schiff’s reagent sections of db/+ (a), Mkk3 +/+ db/db (b) and Mkk3 −/− db/db (c) mice demonstrated that tubular atrophy was greatly increased in diabetes, but significantly improved in Mkk3 −/− db/db mice. Sirius Red staining of collagen in db/+ (d), Mkk3 +/+ db/db (e) and Mkk3 −/− db/db mice (f) demonstrated that diabetic mice developed significant thickening of the tubular basement membrane and increased interstitial collagen, but both of these were reduced in Mkk3 −/− db/db mice. Magnification: ×250
Gene transcript levels of proinflammatory and profibrotic molecules were also measured. Ccl2 was examined because it is known to be increased in diabetic kidneys and promotes interstitial inflammation [35]. At 32 weeks, kidney Ccl2 mRNA was increased more than threefold in diabetic Mkk3 +/+ db/db mice compared with db/+ mice, but this upregulation of Ccl2 was reduced by 50% in diabetic Mkk3 −/− db/db mice (Fig. 8). The accumulation of interstitial CD68-positive macrophages, detected by immunostaining (Table 2), correlated with the increased level of kidney Ccl2 mRNA in diabetic Mkk3 +/+ db/db mice and its reduction in diabetic Mkk3 −/− db/db mice (r = 0.51, p = 0.02). In contrast, kidney mRNA levels of Tgf-β1 and Tnf-α mRNA levels were increased three- to fourfold in diabetic Mkk3 +/+ db/db mice compared with db/+ mice, but were not reduced in diabetic Mkk3 −/− db/db mice (Fig. 8).
Mkk3 deficiency attenuates kidney expression of Ccl2 but not Tgf-β1 or Tnf-α. Assessment of kidney expression of Ccl2 by quantitative RT-PCR (a) demonstrated a threefold increase in Ccl2 mRNA in Mkk3 +/+ db/db compared with control db/+ mice, which was reduced by 50% in Mkk3 −/− db/db mice. Kidney expression of Tgf-β1 (b) and Tnf-α mRNA (c) was increased four- and threefold, respectively, in db/db mice, compared with control db/+ mice, and was not significantly affected by Mkk3 deficiency. Data are means ± SEM; n = 10. a p < 0.05, b p < 0.01 vs db/+ mice; c p < 0.05 vs Mkk3 +/+ db/db mice
Discussion
This study has established a role for MKK3 and its effect on p38 MAPK signalling in the development of diabetic nephropathy in db/db mice. Although Mkk3 deficiency did not alter the incidence or progression of obesity and type 2 diabetes, it did significantly reduce diabetic renal injury and prevented a loss of renal function in our model, indicating that MKK3–p38 signalling is important to the pathology of diabetic nephropathy.
Previous studies had led us to anticipate that Mkk3 deficiency would modify the major metabolic events leading to type 2 diabetes. In vitro experiments have shown that p38 activation reduces expression of the glucose transporter GLUT4 [7, 36] and suppresses adipogenesis by inhibiting Ppar-γ (also known as Pparg) and c/ebp-β (also known as Cebpb) transcriptional activities [37], suggesting that a deficiency of MKK3–p38 signalling might promote insulin-stimulated glucose uptake and adipose expansion. However, our study showed that Mkk3 deficiency did not affect body weight, insulin and glucose tolerance, plasma insulin or epididymal fat accumulation. There was a small difference in liver size, which may be related to reduced hepatic lipogenesis [38], but serum NEFA were unaffected and no observable effect on hyperglycaemia was seen, as demonstrated by the equivalent incidence of type 2 diabetes and similar fasting blood glucose and glycated haemoglobin values in both genotypes. Thus, our findings prove that MKK3–p38 signalling is not by itself critical to the development of obesity or type 2 diabetes and that compensatory mechanisms may exist to overcome any decline in p38 activity in Mkk3 −/− tissues regulating obesity and hyperglycaemia.
Our examination of Mkk3 +/+ db/db mice established that kidney MKK3 levels are increased in type 2 diabetes in association with elevated p38 MAPK signalling. Mkk3 deficiency prevented this increase in kidney p38 MAPK signalling despite a compensatory increase in MKK6. This phenomenon has also been observed in Mkk3 −/− kidneys with obstructive uropathy [39] and is consistent with an in vitro study showing that inhibition of p38α stimulates MKK6 production [40].
Histopathology analysis demonstrated that MKK3–p38 signalling contributes to early glomerular injury in diabetic db/db kidneys. Podocyte depletion is a characteristic feature of diabetic nephropathy, both in experimental models [16] and in human type 2 diabetes [41–43], and is associated with the development of albuminuria. In this study, we saw preservation of podocyte numbers in the diabetic kidneys of Mkk3 −/− compared with Mkk3 +/+ db/db mice, a finding which correlated with protection from albuminuria. This finding supports in vitro observations that activation of p38 by AGE and oxidative stress triggers podocyte apoptosis [16, 21, 28]. However, significant protection from podocyte apoptosis was not observed in our model because podocyte apoptosis is an early response to hyperglycaemia [16] and our db/db mice were examined after 20 weeks of hyperglycaemia. Deficiency of Mkk3 also reduced glomerular levels of α-SMA and collagen in diabetic db/db kidneys, which is consistent with in vitro observations showing that TGF-β1-induced collagen production by murine mesangial cells is dependent on MKK3–p38 signalling [30]. This finding is clinically relevant, since mesangial cell production of α-SMA correlates with glomerulosclerosis in human type 2 diabetes [44].
In diabetic Mkk3 −/− db/db mice, protection against tubulointerstitial damage also coincided with a reduction in albuminuria. Elements of the diabetic milieu (hyperglycaemia and AGE) as well as albuminuria are capable of causing tubular injury, which may occur via the activation of p38 signalling. However, here we were unable to distinguish whether one or both of these mechanisms were affected by a deficiency of Mkk3 in our model.
Increased levels of the Ccl2 gene and its protein MCP-1 are consistently found in diabetic kidneys and are required for the progression of renal inflammation and injury [35, 45]. In this study, Mkk3 −/− db/db mice had reduced kidney expression of Ccl2 mRNA, which correlated with a similar reduction in interstitial macrophages, suggesting that the inflammatory process had been suppressed. In addition, reduced Ccl2 expression may also directly impact on glomerulosclerosis since MCP-1 induces fibronectin production in human mesangial cells, which are known to possess the MCP-1 receptor, and Ccl2 deficiency results in reduced glomerular fibronectin deposition in diabetic kidneys [46]. This potential mechanism is supported by our finding that diabetic Mkk3 −/− kidneys are partially protected from glomerular fibrosis, as well as by a recent study showing that suppression of p38 activity reduces fibronectin production in diabetic glomeruli [47]. Therefore, this study has identified that MKK3–p38 signalling is a factor promoting MCP-1-mediated injury in diabetic kidneys, which is consistent with other models of kidney disease showing that inhibition of p38 signalling suppresses abnormal renal MCP-1 production [13].
In diabetic db/db kidneys, Mkk3 deficiency did not reduce mRNA expression of Tgf-β1 and Tnf-α, suggesting that p38 signalling is either not necessary or that the compensatory increase in MKK6–p38 signalling is sufficient to promote renal production of these cytokines. Evidence for this comes from in vitro studies. Although p38 inhibitors can inhibit IL-1 and TNF-α production by macrophages [48], production of IL-1, IL-6 and TNF-α is not affected in Mkk3 −/− macrophages stimulated with lipopolysaccharide [49]. Thus, the dependence of renal cytokine production on MKK3–p38 signalling may vary according to the stimulus, cell type and the level of p38 activation required. One noteworthy finding in this study is that Mkk3 deficiency reduced renal fibrosis in diabetic db/db mice without lowering kidney expression of Tgf-β1 mRNA. Blockade of p38α has also been reported to reduce acute renal fibrosis without affecting Tgf-β1 mRNA or protein in a rat model of unilateral ureteric obstruction [50]. These findings together suggest that MKK3–p38 signalling plays a role in the development of renal fibrosis by acting downstream of TGF-β1.
In conclusion, MKK3–p38 signalling is not required for the development of obesity or type 2 diabetes, but does play a significant role in the progression of diabetic nephropathy in db/db mice.
Abbreviations
- gcs:
-
glomerular cross-sections
- MAPK:
-
mitogen-activated protein kinase
- MCP-1:
-
monocyte chemoattractant protein-1
- MKK:
-
MAP kinase kinase
- PLP:
-
paraformaldehyde–lysine–periodate
- tcs:
-
tubular cross-sections
- WT:
-
Wilm’s tumour
References
Sheetz MJ, King GL (2002) Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. Jama 288:2579–2588
Zarubin T, Han J (2005) Activation and signaling of the p38 MAP kinase pathway. Cell Res 15:11–18
Cuenda A, Rousseau S (2007) p38 MAP-kinases pathway regulation, function and role in human diseases. Biochim Biophys Acta 1773:1358–1375
Furtado LM, Somwar R, Sweeney G, Niu W, Klip A (2002) Activation of the glucose transporter GLUT4 by insulin. Biochem Cell Biol = Biochimie et Biologie Cellulaire 80:569–578
Adhikary L, Chow F, Nikolic-Paterson DJ et al (2004) Abnormal p38 mitogen-activated protein kinase signalling in human and experimental diabetic nephropathy. Diabetologia 47:1210–1222
Koistinen HA, Chibalin AV, Zierath JR (2003) Aberrant p38 mitogen-activated protein kinase signalling in skeletal muscle from Type 2 diabetic patients. Diabetologia 46:1324–1328
Carlson CJ, Koterski S, Sciotti RJ, Poccard GB, Rondinone CM (2003) Enhanced basal activation of mitogen-activated protein kinases in adipocytes from type 2 diabetes: potential role of p38 in the downregulation of GLUT4 expression. Diabetes 52:634–641
Westermann D, Rutschow S, Van Linthout S et al (2006) Inhibition of p38 mitogen-activated protein kinase attenuates left ventricular dysfunction by mediating pro-inflammatory cardiac cytokine levels in a mouse model of diabetes mellitus. Diabetologia 49:2507–2513
Ando H, Kurita S, Takamura T (2004) The specific p38 mitogen-activated protein kinase pathway inhibitor FR167653 keeps insulitis benign in nonobese diabetic mice. Life Sci 74:1817–1827
Aouadi M, Jager J, Laurent K et al (2007) p38MAP kinase activity is required for human primary adipocyte differentiation. FEBS lett 581:5591–5596
Carlson CJ, Rondinone CM (2005) Pharmacological inhibition of p38 MAP kinase results in improved glucose uptake in insulin-resistant 3T3-L1 adipocytes. Metabolism 54:895–901
Sakai N, Wada T, Furuichi K et al (2005) Involvement of extracellular signal-regulated kinase and p38 in human diabetic nephropathy. Am J Kidney Dis 45:54–65
Sheryanna A, Bhangal G, McDaid J et al (2007) Inhibition of p38 mitogen-activated protein kinase is effective in the treatment of experimental crescentic glomerulonephritis and suppresses monocyte chemoattractant protein-1 but not IL-1beta or IL-6. J Am Soc Nephrol 18:1167–1179
Stambe C, Atkins RC, Tesch GH et al (2003) Blockade of p38alpha MAPK ameliorates acute inflammatory renal injury in rat anti-GBM glomerulonephritis. J Am Soc Nephrol 14:338–351
Wilmer WA, Dixon CL, Hebert C (2001) Chronic exposure of human mesangial cells to high glucose environments activates the p38 MAPK pathway. Kidney Int 60:858–871
Susztak K, Raff AC, Schiffer M, Bottinger EP (2006) Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy. Diabetes 55:225–233
Zhang SL, Tang SS, Chen X, Filep JG, Ingelfinger JR, Chan JS (2000) High levels of glucose stimulate angiotensinogen gene expression via the P38 mitogen-activated protein kinase pathway in rat kidney proximal tubular cells. Endocrinology 141:4637–4646
Daoud S, Schinzel R, Neumann A et al (2001) Advanced glycation endproducts: activators of cardiac remodeling in primary fibroblasts from adult rat hearts. Mol Med 7:543–551
Liu BF, Miyata S, Hirota Y et al (2003) Methylglyoxal induces apoptosis through activation of p38 mitogen-activated protein kinase in rat mesangial cells. Kidney Int 63:947–957
Kang YS, Park YG, Kim BK et al (2006) Angiotensin II stimulates the synthesis of vascular endothelial growth factor through the p38 mitogen activated protein kinase pathway in cultured mouse podocytes. J Mol Endocrinol 36:377–388
Chuang PY, Yu Q, Fang W, Uribarri J, He JC (2007) Advanced glycation endproducts induce podocyte apoptosis by activation of the FOXO4 transcription factor. Kidney Int 72:965–976
Porras A, Zuluaga S, Black E et al (2004) P38 alpha mitogen-activated protein kinase sensitizes cells to apoptosis induced by different stimuli. Mol Biol Cell 15:922–933
Takaishi H, Taniguchi T, Takahashi A, Ishikawa Y, Yokoyama M (2003) High glucose accelerates MCP-1 production via p38 MAPK in vascular endothelial cells. Biochem Biophys Res Commun 305:122–128
Suzuki H, Uchida K, Nitta K, Nihei H (2004) Role of mitogen-activated protein kinase in the regulation of transforming growth factor-beta-induced fibronectin accumulation in cultured renal interstitial fibroblasts. Clin Exp Neurol 8:188–195
Chin BY, Mohsenin A, Li SX, Choi AM, Choi ME (2001) Stimulation of pro-alpha(1)(I) collagen by TGF-beta(1) in mesangial cells: role of the p38 MAPK pathway. Am J Physiol Renal Physiol 280:F495–F504
Fujita H, Omori S, Ishikura K, Hida M, Awazu M (2004) ERK and p38 mediate high-glucose-induced hypertrophy and TGF-beta expression in renal tubular cells. Am J Physiol Renal Physiol 286:F120–F126
Wu DT, Bitzer M, Ju W, Mundel P, Bottinger EP (2005) TGF-beta concentration specifies differential signaling profiles of growth arrest/differentiation and apoptosis in podocytes. J Am Soc Nephrol 16:3211–3221
Schiffer M, Bitzer M, Roberts IS et al (2001) Apoptosis in podocytes induced by TGF-beta and Smad7. J Clin Invest 108:807–816
Zhuang S, Yan Y, Han J, Schnellmann RG (2005) p38 kinase-mediated transactivation of the epidermal growth factor receptor is required for dedifferentiation of renal epithelial cells after oxidant injury. J Biol Chem 280:21036–21042
Wang L, Ma R, Flavell RA, Choi ME (2002) Requirement of mitogen-activated protein kinase kinase 3 (MKK3) for activation of p38alpha and p38delta MAPK isoforms by TGF-beta 1 in murine mesangial cells. J Biol Chem 277:47257–47262
Wang L, Kwak JH, Kim SI, He Y, Choi ME (2004) Transforming growth factor-beta1 stimulates vascular endothelial growth factor 164 via mitogen-activated protein kinase kinase 3-p38alpha and p38delta mitogen-activated protein kinase-dependent pathway in murine mesangial cells. J Biol Chem 279:33213–33219
Inoue T, Boyle DL, Corr M et al (2006) Mitogen-activated protein kinase kinase 3 is a pivotal pathway regulating p38 activation in inflammatory arthritis. Proc Natl Acad Sci U S A 103:5484–5489
Fukuda K, Tesch GH, Yap FY et al (2008) MKK3 signalling plays an essential role in leukocyte-mediated pancreatic injury in the multiple low-dose streptozotocin model. Lab Invest 88:398–407
Wysk M, Yang DD, Lu HT, Flavell RA, Davis RJ (1999) Requirement of mitogen-activated protein kinase kinase 3 (MKK3) for tumor necrosis factor-induced cytokine expression. Proc Natl Acad Sci U S A 96:3763–3768
Chow FY, Nikolic-Paterson DJ, Ma FY, Ozols E, Rollins BJ, Tesch GH (2007) Monocyte chemoattractant protein-1-induced tissue inflammation is critical for the development of renal injury but not type 2 diabetes in obese db/db mice. Diabetologia 50:471–480
Fujishiro M, Gotoh Y, Katagiri H et al (2001) MKK6/3 and p38 MAPK pathway activation is not necessary for insulin-induced glucose uptake but regulates glucose transporter expression. J Biol Chem 276:19800–19806
Aouadi M, Laurent K, Prot M, Le Marchand-Brustel Y, Binetruy B, Bost F (2006) Inhibition of p38MAPK increases adipogenesis from embryonic to adult stages. Diabetes 55:281–289
Xiong Y, Collins QF, An J et al (2007) p38 mitogen-activated protein kinase plays an inhibitory role in hepatic lipogenesis. J Biol Chem 282:4975–4982
Ma FY, Tesch GH, Flavell RA, Davis RJ, Nikolic-Paterson DJ (2007) MKK3-p38 signaling promotes apoptosis and the early inflammatory response in the obstructed mouse kidney. Am J Physiol Renal Physiol 293:F1556–F1563
Ambrosino C, Mace G, Galban S et al (2003) Negative feedback regulation of MKK6 mRNA stability by p38alpha mitogen-activated protein kinase. Mol Cell Biol 23:370–381
Dalla Vestra M, Masiero A, Roiter AM, Saller A, Crepaldi G, Fioretto P (2003) Is podocyte injury relevant in diabetic nephropathy? Studies in patients with type 2 diabetes. Diabetes 52:1031–1035
Pagtalunan ME, Miller PL, Jumping-Eagle S et al (1997) Podocyte loss and progressive glomerular injury in type II diabetes. J Clin Invest 99:342–348
Verzola D, Gandolfo MT, Ferrario F et al (2007) Apoptosis in the kidneys of patients with type II diabetic nephropathy. Kidney Int 72:1262–1272
Yonemoto S, Machiguchi T, Nomura K, Minakata T, Nanno M, Yoshida H (2006) Correlations of tissue macrophages and cytoskeletal protein expression with renal fibrosis in patients with diabetes mellitus. Clin Exp Neurol 10:186–192
Tesch GH (2008) MCP-1/CCL2: a new diagnostic marker and therapeutic target for progressive renal injury in diabetic nephropathy. Am J Physiol Renal Physiol 294:F607–F701
Giunti S, Tesch GH, Pinach S et al (2008) Monocyte chemoattractant protein-1 has prosclerotic effects both in a mouse model of experimental diabetes and in vitro in human mesangial cells. Diabetologia 51:198–207
Jung DS, Li JJ, Kwak SJ et al (2008) FR167653 inhibits fibronectin expression and apoptosis in diabetic glomeruli and in high-glucose-stimulated mesangial cells. Am J Physiol Renal Physiol 295:F595–F604
Lee JC, Laydon JT, McDonnell PC et al (1994) A protein kinase involved in the regulation of inflammatory cytokine biosynthesis. Nature 372:739–746
Lu HT, Yang DD, Wysk M et al (1999) Defective IL-12 production in mitogen-activated protein (MAP) kinase kinase 3 (Mkk3)-deficient mice. EMBO J 18:1845–1857
Stambe C, Atkins RC, Tesch GH, Masaki T, Schreiner GF, Nikolic-Paterson DJ (2004) The role of p38alpha mitogen-activated protein kinase activation in renal fibrosis. J Am Soc Nephrol 15:370–379
Acknowledgements
We thank N. Gibson, Y. Han, P. Frost and E. Grixti for their technical assistance. This study was funded by the National Health and Medical Research Council of Australia and Kidney Health Australia.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, A.K.H., Nikolic-Paterson, D.J., Ma, F.Y. et al. Role of MKK3–p38 MAPK signalling in the development of type 2 diabetes and renal injury in obese db/db mice. Diabetologia 52, 347–358 (2009). https://doi.org/10.1007/s00125-008-1215-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1215-5