Abstract
Objective
Different mechanical circulatory support (MCS) systems are used in children with intractable heart failure. However, the need for anticoagulation leads to hemorrhage with subsequent use of blood products. We compared the coagulation disorders and the need for blood products in children treated either with extracorporeal membrane oxygenation (ECMO) or with the Berlin Heart pulsatile pneumatic ventricular assist device.
Patients
We retrospectively reviewed the first 8-day course of 64 children who were on MCS for more than 2 days between 1990 and 2002. Thirty children (median age 7.4 years, weight 25.5 kg) received Berlin Heart support and 34 children (median age 1.8 years, weight 9.2 kg) ECMO. Anticoagulation was accomplished by continuous infusion of heparin. Red blood cell count, platelet count, aPTT, AT III, fibrinogen, and ACT were measured regularly. Depending on blood loss and the coagulation disorder, red blood cells, fresh frozen plasma, platelets, and AT III were substituted.
Results
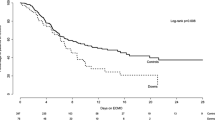
There were no preoperative differences in hematological parameters between the two groups. In the Berlin Heart group platelet transfusion was 4.3 ml·kg·day vs 24.6 ml·kg·day in the ECMO group. Red blood cell substitution was 17.2 vs 60.3 ml·kg·day. Fresh frozen plasma substitution was 8.5 ml·kg·day vs 46.9 ml·kg·day (P<0.001). Even in the congenital heart defect subgroups, when MCS was implanted without recent cardiotomy, the differences were significant. Nevertheless, the mean daily values for hemoglobin, platelets, and fibrinogen were lower in the ECMO group. There was lower overall mortality in the Berlin Heart group.
Conclusions
Compared to ECMO, use of the Berlin Heart in children results in less blood loss and lower consumption of red blood cells, platelets, and fresh frozen plasma.




Similar content being viewed by others
References
Duncan BW (2002) Mechanical circulatory support for infants and children with cardiac disease. Ann Thorac Surg 73:1670–1677
Beghetti M, Rimensberger PC (2000) Mechanical circulatory support in pediatric patients. Intensive Care Med 26:350–352
Hetzer R, Loebe M, Weng Y, Alexi-Meskhishvili V, Stiller B (1999) Pulsatile pediatric ventricular assist devices: current results for bridge to transplantation. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2:157–176
Duncan BW, Hraska V, Jonas RA, Wessel DL, Del Nido PJ, Laussen PC, Mayer JE, Lapierre RA, Wilson JM (1999) Mechanical circulatory support in children with cardiac disease. J Thorac Cardiovasc Surg 117:529–542
Reinhartz O, Keith FM, El-Banayosy A, McBride LR, Robbins RC, Copeland JG, Farrar DJ (2001) Multicenter experience with the thoratec ventricular assist device in children and adolescents. J Heart Lung Transplant 20:439–448
Levi D, Marelli D, Plunkett M, Alejos J, Bresson J, Tran J, Eisenring C, Sadeghi A, Galindo A, Fazio D, Gupta A, Burch C, George B, Laks H (2002) Use of assist devices and ECMO to bridge pediatric patients with cardiomyopathy to transplantation. J Heart Lung Transplant 21:760–770
Ibrahim AE, Duncan BW, Blume ED, Jonas RA (2000) Long-term follow-up of pediatric cardiac patients requiring mechanical circulatory support. Ann Thorac Surg 69:186–192
Aharon AS, Drinkwater DC Jr, Churchwell KB, Quisling SV, Reddy VS, Taylor M, Hix S, Christian KG, Pietsch JB, Deshpande JK, Kambam J, Graham TP, Chang PA (2001) Extracorporeal membrane oxygenation in children after repair of congenital cardiac lesions. Ann Thorac Surg 72:2095–2101
Kirshbom PM, Bridges ND, Myung RJ, Gaynor JW, Clark BJ, Spray TL (2002) Use of extracorporeal membrane oxygenation in pediatric thoracic organ transplantation. J Thorac Cardiovasc Surg 123:130–136
Mehta U, Laks H, Sadeghi A, Marelli D, Odim J, Alejos J, Kim M, Atkinson JB, Bui KC (2000) Extracorporeal membrane oxygenation for cardiac support in pediatric patients. Am Surg 66:879–886
del Nido PJ, Armitage JM, Fricker FJ, Shaver M, Cipriani L, Dayal G, Park SC, Siewers RD (1994) Extracorporeal membrane oxygenation support as a bridge to pediatric heart transplantation. Circulation 90:1166–1169
Reinhartz O, Stiller B, Eilers R, Farrar DJ (2002) Current clinical status of pulsatile pediatric circulatory support. Asaio J 48:455–459
Stiller B, Dahnert I, Berger F, Weng Y, Loebe M, Alexi-Meskhishvili V, Hetzer R, Lange PE (2000) Artificial heart in terminal stage of dilated cardiomyopathy in childhood. Z Kardiol 89:1039–1045
Ishino K, Loebe M, Uhlemann F, Weng Y, Hennig E, Hetzer R (1997) Circulatory support with paracorporeal pneumatic ventricular assist device (VAD) in infants and children. Eur J Cardiothorac Surg 11:965–972
Throckmorton AL, Allaire PE, Gutgesell JH, Matherne JG, Olsen DB, Wood HG, Allaire JH, Patel SM (2002) Pediatric circulatory support systems. Asaio J 48:216–221
Stiller B, Lange PE, Hetzer R (2002) Left ventricular assist device. N Engl J Med 346:1023–1025
Muntean W (1999) Coagulation and anticoagulation in extracorporeal membrane oxygenation. Artif Organs 23:979–983
Jarjour IT, Ahdab-Barmada M (1994) Cerebrovascular lesions in infants and children dying after extracorporeal membrane oxygenation. Pediatr Neurol 10:13–19
Muntean W (2002) Fresh frozen plasma in the pediatric age group and in congenital coagulation factor deficiency. Thromb Res 107:S29
Zavadil DP, Stammers AH, Willett LD, Deptula JJ, Christensen KA, Sydzyik RT (1998) Hematological abnormalities in neonatal patients treated with extracorporeal membrane oxygenation (ECMO). J Extra Corpor Technol 30:83–90
Hirthler MA, Blackwell E, Abbe D, Doe-Chapman R, LeClair Smith C, Goldthorn J, Canizaro P (1992) Coagulation parameter instability as an early predictor of intracranial hemorrhage during extracorporeal membrane oxygenation. J Pediatr Surg 27:40–43
Stiller B, Dahnert I, Weng YG, Hennig E, Hetzer R, Lange PE (1999) Children may survive severe myocarditis with prolonged use of biventricular assist devices. Heart 82:237–240
Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP, Chang AC (2000) Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med 28:3296–3300
Stallion A, Cofer BR, Rafferty JA, Ziegler MM, Ryckman FC (1994) The significant relationship between platelet count and haemorrhagic complications on ECMO. Perfusion 9:265–269
McManus ML, Kevy SV, Bower LK, Hickey PR (1995) Coagulation factor deficiencies during initiation of extracorporeal membrane oxygenation. J Pediatr 126:900–904
Loebe M, Hennig E, Müller J, Spiegelsberger S, Weng Y, Hetzer R (1997) Long-term mechanical circulatory support as a bridge to transplantation, for recovery from cardiomyopathy, and for permanent replacement. Eur J Cardiothorac Surg 11:S18–24
Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, Long JW, Ascheim DD, Tierney AR, Levitan RG, Watson JT, Meier P, Ronan NS, Shapiro PA, Lazar RM, Miller LW, Gupta L, Frazier OH, Desvigne-Nickens P, Oz MC, Poirier VL (2001) Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med 345:1435–1443
Hetzer R, Loebe M, Potapov EV, Weng Y, Stiller B, Hennig E, Alexi-Meskishvili V, Lange PE (1998) Circulatory support with pneumatic paracorporeal ventricular assist device in infants and children. Ann Thorac Surg 66:1498–1506
Cheung PY, Sawicki G, Salas E, Etches PC, Schulz R, Radomski MW (2000) The mechanisms of platelet dysfunction during extracorporeal membrane oxygenation in critically ill neonates. Crit Care Med 28:2584–2590
Graves DF, Chernin JM, Kurusz M, Zwischenberger JB (1996) Anticoagulation practices during neonatal extracorporeal membrane oxygenation: survey results. Perfusion 11:461–466
De Waele JJ, Van Cauwenberghe S, Hoste E, Benoit D, Colardyn F (2003) The use of the activated clotting time for monitoring heparin therapy in critically ill patients. Intensive Care Med 29:325–328
Rosenthal DN, Dubin AM, Chin C, Falco D, Gamberg P, Bernstein D (2000) Outcome while awaiting heart transplantation in children: a comparison of congenital heart disease and cardiomyopathy. J Heart Lung Transplant 19:751–755
Acknowledgement
We are grateful for statistical calculations by Julia Stein and editorial assistance by Anne Gale, both of the Deutsches Herzzentrum Berlin, Germany
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest: Dr. Roland Hetzer received 4,000 Euros per year as consultant from the company Berlin Heart
Rights and permissions
About this article
Cite this article
Stiller, B., Lemmer, J., Merkle, F. et al. Consumption of blood products during mechanical circulatory support in children: comparison between ECMO and a pulsatile ventricular assist device. Intensive Care Med 30, 1814–1820 (2004). https://doi.org/10.1007/s00134-004-2352-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2352-z