Abstract
Objective
To test the hypothesis that, in resuscitated septic shock patients, central venous-to-arterial carbon dioxide difference [P(cv-a)CO2] may serve as a global index of tissue perfusion when the central venous oxygen saturation (ScvO2) goal value has already been reached.
Design
Prospective observational study.
Setting
A 22-bed intensive care unit (ICU).
Patients
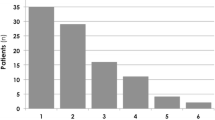
After early resuscitation in the emergency unit, 50 consecutive septic shock patients with ScvO2 > 70% were included immediately after their admission into the ICU (T0). Patients were separated in Low P(cv-a)CO2 group (Low gap; n = 26) and High P(cv-a)CO2 group (High gap; n = 24) according to a threshold of 6 mmHg at T0.
Measurements
Measurements were performed every 6 h over 12 h (T0, T6, T12).
Results
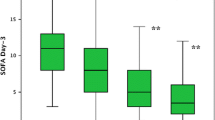
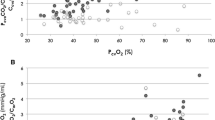
At T0, there was a significant difference between Low gap patients and High gap patients for cardiac index (CI) (4.3 ± 1.6 vs. 2.7 ± 0.8 l/min/m², P < 0.0001) but not for ScvO2 values (78 ± 5 vs. 75 ± 5%, P = 0.07). From T0 to T12, the clearance of lactate was significantly larger for the Low gap group than for the High gap group (P < 0.05) as well as the decrease of SOFA score at T24 (P < 0.01). At T0, T6 and T12, CI and P(cv-a)CO2 values were inversely correlated (P < 0.0001).
Conclusion
In ICU-resuscitated patients, targeting only ScvO2 may not be sufficient to guide therapy. When the 70% ScvO2 goal-value is reached, the presence of a P(cv-a)CO2 larger than 6 mmHg might be a useful tool to identify patients who still remain inadequately resuscitated.

Similar content being viewed by others
References
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Varpula M, Karlsson S, Ruokonen E, Pettila V (2006) Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Intensive Care Med 32:1336–1343
van Beest P, Hofstra J, Schultz M, Boerma E, Spronk P, Kuiper M (2008) The incidence of low venous oxygen saturation on admission to the intensive care unit: a multi-center observational study in The Netherlands. Crit Care 12:R33
Ince C, Sinaasappel M (1999) Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 27:1369–1377
Fink MP (2002) Cytopathic hypoxia. Is oxygen use impaired in sepsis as a result of an acquired intrinsic derangement in cellular respiration? Crit Care Clin 18:165–175
Vallee F, Fourcade O, Marty P, Sanchez P, Samii K, Genestal M (2007) The hemodynamic “target”: a visual tool of goal-directed therapy for septic patients. Clinics 62:447–454
Ladakis C, Myrianthefs P, Karabinis A, Karatzas G, Dosios T, Fildissis G, Gogas J, Baltopoulos G (2001) Central venous and mixed venous oxygen saturation in critically ill patients. Respiration 68:279–285
Brandi LS, Giunta F, Pieri M, Sironi AM, Mazzanti T (1995) Venous-arterial PCO2 and pH gradients in acutely ill postsurgical patients. Minerva Anestesiol 61:345–350
Groeneveld AB, Vermeij CG, Thijs LG (1991) Arterial and mixed venous blood acid-base balance during hypoperfusion with incremental positive end-expiratory pressure in the pig. Anesth Analg 73:576–582
Durkin R, Gergits MA, Reed JF 3rd, Fitzgibbons J (1993) The relationship between the arteriovenous carbon dioxide gradient and cardiac index. J Crit Care 8:217–221
Mecher CE, Rackow EC, Astiz ME, Weil MH (1990) Venous hypercarbia associated with severe sepsis and systemic hypoperfusion. Crit Care Med 18:585–589
Bakker J, Vincent JL, Gris P, Leon M, Coffernils M, Kahn RJ (1992) Veno-arterial carbon dioxide gradient in human septic shock. Chest 101:509–515
Rackow EC, Astiz ME, Mecher CE, Weil MH (1994) Increased venous-arterial carbon dioxide tension difference during severe sepsis in rats. Crit Care Med 22:121–125
Vallet B, Teboul JL, Cain S, Curtis S (2000) Venoarterial CO2 difference during regional ischemic or hypoxic hypoxia. J Appl Physiol 89:1317–1321
Neviere R, Chagnon JL, Teboul JL, Vallet B, Wattel F (2002) Small intestine intramucosal PCO2 and microvascular blood flow during hypoxic and ischemic hypoxia. Crit Care Med 30:379–384
Lamia B, Monnet X, Teboul JL (2006) Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol 72:597–604
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM (2005) Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med 31:818–822
Vallet B, Lebuffe G (2007) How to titrate vasopressors against fluid loading in septic shock. Adv Sepsis 6:34–40
Annane D, Aegerter P, Jars-Guincestre MC, Guidet B (2003) Current epidemiology of septic shock: the CUB-Rea Network. Am J Respir Crit Care Med 168:165–172
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709
Adrogue HJ, Rashad MN, Gorin AB, Yacoub J, Madias NE (1989) Assessing acid-base status in circulatory failure. Differences between arterial and central venous blood. N Engl J Med 320:1312–1316
Gutierrez G (2004) A mathematical model of tissue-blood carbon dioxide exchange during hypoxia. Am J Respir Crit Care Med 169:525–533
Wasserman K, Whipp BJ, Koyl SN, Beaver WL (1973) Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 35:236–243
Raza O, Schlichtig R (2000) Metabolic component of intestinal PCO2 during dysoxia. J Appl Physiol 89:2422–2429
Cohen IL, Sheikh FM, Perkins RJ, Feustel PJ, Foster ED (1995) Effect of hemorrhagic shock and reperfusion on the respiratory quotient in swine. Crit Care Med 23:545–552
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL (2002) Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med 166:98–104
Bakker J, Coffernils M, Leon M, Gris P, Vincent JL (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99:956–962
Teboul JL, Mercat A, Lenique F, Berton C, Richard C (1998) Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med 26:1007–1010
Groeneveld AB (1998) Interpreting the venous-arterial PCO2 difference. Crit Care Med 26:979–980
Lind L (1995) Veno-arterial carbon dioxide and pH gradients and survival in critical illness. Eur J Clin Invest 25:201–205
Mekontso-Dessap A, Castelain V, Anguel N, Bahloul M, Schauvliege F, Richard C, Teboul JL (2002) Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med 28:272–277
Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Abramson D, Scalea TM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J (1993) Lactate clearance and survival following injury. J Trauma 35:584–588; discussion 588–589
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC (2004) Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 32:1637–1642
Reinhart K, Kuhn HJ, Hartog C, Bredle DL (2004) Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 30:1572–1578
Varpula M, Tallgren M, Saukkonen K, Voipio-Pulkki LM, Pettila V (2005) Hemodynamic variables related to outcome in septic shock. Intensive Care Med 31:1066–1071
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2008_1199_MOESM1_ESM.doc
ESM Figure 1: Correlation between CI and P(cv-a)CO2 at each time. T0: r = 0.57, p<0.0001; T6: r = 0.58, p<0.0001 and T12 : r = 0.58, p<0.0001 (DOC 40 kb)
Rights and permissions
About this article
Cite this article
Vallée, F., Vallet, B., Mathe, O. et al. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock?. Intensive Care Med 34, 2218–2225 (2008). https://doi.org/10.1007/s00134-008-1199-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1199-0