Abstract
Background
Postoperative pulmonary complications, generally defined as any pulmonary abnormality occurring in the postoperative period, are still a significant issue in clinical practice increasing hospital length of stay, morbidity and mortality. Non-invasive ventilation (NIV), primarily applied in cardiogenic pulmonary edema, decompensated COPD and hypoxemic pulmonary failure, is nowadays also used in perioperative settings.
Objective
Investigate the application and results of preventive and therapeutic NIV in postsurgical patients.
Design
A systematic review.
Data sources
Medical literature databases were searched for articles about “clinical trials,” “randomized controlled trials” and “meta-analyses.” The keywords “cardiac surgery,” “thoracic surgery,” “lung surgery,” “abdominal surgery,” “solid organ transplantation,” “thoraco-abdominal surgery” and “bariatric surgery” were combined with any of these: “non-invasive positive pressure ventilation,” “continuous positive airway pressure,” “bilevel ventilation,” “postoperative complications,” “postoperative care,” “respiratory care,” “acute respiratory failure,” “acute lung injury” and “acute respiratory distress syndrome.”
Results
Twenty-nine articles (N = 2,279 patients) met the inclusion criteria. Nine studies evaluated NIV in post-abdominal surgery, three in thoracic surgery, eight in cardiac surgery, three in thoraco-abdominal surgery, four in bariatric surgery and two in post solid organ transplantation used both for prophylactic and therapeutic purposes. NIV improved arterial blood gases in 15 of the 22 prophylactic and in 4 of the 7 therapeutic studies, respectively. NIV reduced the intubation rate in 11 of the 29 studies and improved outcome in only 1.
Conclusions
Despite these limited data and the necessity of new randomized trials, NIV could be considered as a prophylactic and therapeutic tool to improve gas exchange in postoperative patients.
Similar content being viewed by others
Introduction
Recent data suggest that up to 234 million major surgical procedures requiring general or spinal-epidural anesthesia are performed worldwide each year [1]. Postoperative pulmonary complications (PPCs) are generally defined as any pulmonary abnormality occurring in the postoperative period. They may increase hospital length of stay, morbidity, mortality [2] and costs for the health care system [3]. PPCs can include atelectasis, postoperative pneumonia, pulmonary edema, acute respiratory failure, although incidence and clinical significance may vary among them [4]. It has been reported that 5 to 10% of all surgical patients and 9 to 40% of those undergoing abdominal surgery developed at least one PPCs [5–8]. These data show that PPCs occur at the same rate as cardiac complications in non-cardiac surgery [9].
PPCs following surgery can be related to either complications of surgery or general anesthesia (e.g., bronchospasm atelectasis, infection, pulmonary embolism up to ALI/ARDS) and/or specific complications such as those occurring during cardiac surgery such as pleural effusion, bronchopleural fistula, phrenic nerve palsy, sternal wound infection, and severe sepsis [10]. Several pulmonary pathophysiological modifications occurring during anesthesia can persist for days following the surgery, thus increasing the risk of PPCs. The induction of anesthesia, upper abdominal and thoracic surgery are usually associated with a reduction in lung gas volumes promoting lower lobe atelectasis [11, 12]. Atelectasis usually occurs in the most dependent parts of the lung near the diaphragm, which includes about 10% of the total lung tissue and may persist for 2 days after major surgery [13, 14].
Dysfunction of the respiratory muscles, especially of the diaphragm, will occur in the first hours after surgery and may persist up to 1 or 2 weeks [15]. The surgery may impair abdominal, thoracic and diaphragmatic muscles, inducing pain and reducing the phrenic output [16]. All these factors can cause respiratory failure because of respiratory muscle impairment, with an increase in carbon dioxide and/or disorders of lung parenchyma, ventilation-perfusion mismatching and hypoxemia [16–18].
In addition, different risk factors can be simultaneously present in the same patient, thus significantly increasing the probability of developing PPCs.
Arozullah et al. [4], in a very large multicenter observational study enrolling more than 80,000 subjects undergoing major non-cardiac surgery, identified several predictors for PPCs that were then used to compute a respiratory failure index. Postoperative respiratory failure was defined as mechanical ventilation for more than 48 h after surgery or the need for reintubation and mechanical ventilation after postoperative extubation.
The respiratory failure index was analogous to the risk assessment model currently used for predicting postoperative cardiac complications. The respiratory failure risk index was developed from a simplified logistic regression model. Eleven predictors were found. Among them, abdominal aortic aneurysm repair, thoracic, abdominal and emergency surgery, an albumin level less than 30 g/l, a BUN higher than 30 mg/dl, a history of COPD and age higher than 70 years significantly increased the risk of complications. Each of these predictors has a point value, ranging from 4 to 24, so by adding the point value of each of these, it is possible to obtain the respiratory failure index.
The authors found that the higher the respiratory failure index, the higher the risk of developing a PPC.
The more commonly applied strategies to prevent postoperative pulmonary complications include good analgesia, physiotherapy, oxygen therapy and early mobilization [19–21].
Non-invasive ventilation (NIV) is a mechanical ventilation modality that does not require any artificial airway (endotracheal tube or tracheostomy) and, compared to invasive ventilation, requires lower sedation, improves the comfort and reduces the nosocomial infection rate [22, 23].
NIV has primarily been applied in patients with acute exacerbations of chronic obstructive pulmonary disease, cardiogenic pulmonary edema and hypoxemic respiratory failure [22–26]. In recent years NIV has also been used to prevent the occurrence of acute respiratory failure after surgery (prophylactic use) or to treat acute respiratory failure (therapeutic use) [27, 28]. In a phone survey of 60 intensive care units in France, 69% of physicians used NIV as first line treatment in patients with postoperative respiratory failure [29].
NIV has been applied primarily in patients both as continuous positive airway pressure (CPAP) and non-invasive intermittent positive pressure ventilation (NPPV) in different settings [22–26].
The main expected benefits from applying NIV in PPCs are an increase in gas lung volume, an improvement in gas exchange, a reduction of atelectasis and work of breathing without the need for endotracheal intubation, thus avoiding the risk of invasive mechanical ventilation [21, 24, 30–32].
We undertook a systematic review of the randomized controlled trials (RCTs) to determine the efficacy of NIV versus standard therapy to treat or to prevent PPCs in patients undergoing different types of surgery.
Methods
Search strategy
We systematically searched MEDLINE from 1996 to September 2010, EMBASE from 1950 to September 2010 and the Cochrane Central Register of controlled Trials for English articles, limiting the search to “clinical trials” and “randomized controlled trials.” The following keywords, “cardiac surgery,” “thoracic surgery,” “lung surgery,” “abdominal surgery,” “solid organ transplantation,” “thoraco-abdominal surgery” and “bariatric surgery,” were combined with any of these: “non-invasive ventilation,” “non-invasive pressure support ventilation,” “continuous positive airway pressure,” “bilevel ventilation,” “postoperative complications,” “postoperative care,” “respiratory care,” “acute respiratory failure,” “acute lung injury” and “acute respiratory distress syndrome.” Biographies of all selected articles and review article were hand searched for additional relevant articles.
Results
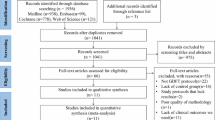
A total of 29 articles met the inclusion criteria and were considered in this systematic review. Nineteen of these studies used CPAP [21, 33–49], and nine used NPPV [50–58]. One study used both CPAP and NPPV [59]. Figure 1 shows the distribution of the preventive and therapeutic NIV clinical trials in a postoperative setting. Seven of the 29 articles applied NIV as a therapeutic tool to reduce PPCs. Evidence synthesis of the randomized control trials on NIV is summarized in Tables 1, 2, and 3.
Abdominal surgery
Hypoxemia complicates the recovery of 30–50% of patients after abdominal surgery; endotracheal intubation and mechanical ventilation may be required in 8–10% of cases, prolonging intensive care and hospital stay and increasing mortality [47]. In a prospective clinical evaluation over a 2-year period in 463 patients admitted to intensive care after abdominal surgery, acute respiratory failure occurred in 96 patients after extubation [60]. Seventy-two patients received NPPV. Forty-eight (67%) of these patients were non-intubated. The intubated patients compared to non-intubated patients presented significantly lower oxygenation on intensive care admission. Interestingly, oxygenation improved only in the non-intubated patients with a concomitant decrease in respiratory rate within the first hours of NPPV treatment.
Prophylactic CPAP
Compared to respiratory therapy (incentive spirometry or coughing and deep breathing), the periodic application of CPAP begun after extubation and continued in the postoperative period was associated with significantly higher arterial oxygenation [46], a quicker recovery of lung volumes [21, 42, 46] and a lower rate of atelectasis [21].
When CPAP was continuously applied for three postoperative hours both in intubated patients at the end of the abdominal surgery [33] and after extubation for at least 12 h [34], it significantly improved arterial oxygenation [33, 34], while the pulmonary complications and rate of reintubation were similar to conventional treatment. Conversely, Carlsson et al. [35], when considering only patients after cholecystectomy, did not find any beneficial effect after the application of non-invasive CPAP every 4 h in terms of arterial oxygenation or spirometry values compared to oxygen therapy. However, CPAP was not found to cause any significant difference in the length of stay [37].
A large multicenter prospective randomized clinical trial carried out by Squadrone et al. [47] cannot be considered either as prophylactic or as a curative tool. They used CPAP delivered by helmet compared with standard treatment in patients who developed acute hypoxemia after elective major abdominal surgery. Patients were extubated after surgery and underwent a 1-h screening test breathing oxygen at an inspiratory fraction of 0.3. If the PaO2/FiO2 remained lower than 300, the patients were randomized to receive CPAP or oxygen for a 6-h period until the acute respiratory failure resolved. Two hundred nine patients were enrolled: one patient (1%) in the CPAP group compared to ten patients (10%) in the control group required intubation. The reasons for intubation were severe hypoxemia and hemodynamic instability. The intensive care length of stay and infection rate were significantly lower in patients treated with CPAP (2.6 ± 4.2 vs. 1.4 ± 1.6 days and 3 vs. 10%, respectively). The hospital length of stay and the outcome did not differ between groups.
Therapeutic NPPV
In a matched controlled study Conti et al. evaluated the NPPV delivered by helmet or face mask to prevent endotracheal intubation in patients with acute respiratory failure after abdominal surgery [53]. Acute respiratory failure was defined by an arterial oxygenation lower than 60 mmHg and with a respiratory rate higher than 25 breaths per min. A sustained improvement in oxygenation was similarly obtained in both groups. The helmet group was associated with a significantly lower number (16 vs. 76%) of general complications (NPPV intolerance, air leaks, nosocomial pneumonia) and with a lower incidence of endotracheal intubations (20 vs. 48%); however, the intensive care mortality did not change between the groups.
Thoracic surgery
Although postoperative mortality and morbidity after lung resection has decreased over the years, its rate still remains high [52]. The overall mortality ranges between 6.2 and 24% after pneumonectomy [61, 62] and between 2.2 and 4.6% after lobectomy [61–63]. Pulmonary complications remain the leading cause of death [64], occurring in between 60 and 80% of the patients [5]. During a 6-year period, Kutlu et al. [65] investigated the frequency of acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) and related mortality after pulmonary resection in more than 1,000 patients. Among the overall lung resections, 625 (55%) were carried out for lung cancer with a combined frequency of ALI/ARDS of 3.9%. Considering the age of the patients, the frequency of ALI/ARDS was 2.8% in patients under 60 years and 4.9% in patients over 60; among patients who developed ALI/ARDS, the overall mortality was 64%. Recently, Sen et al. [66] in an observational study reported that ARDS developed in 7.5% of patients requiring mechanical ventilation after lung resection.
Prophylactic NPPV
In a physiologic study, Aguilo et al. [50] investigated the short-term effects of bilevel ventilation in patients extubated after lung surgery and able to maintain spontaneous breathing compared to conventional treatment. The NPPV was maintained for 60 min. NPPV significantly increased the arterial oxygenation, and this effect was still present 1 h after removing the ventilator support. NPPV did not affect the carbon dioxide level and the physiological dead space. NPPV tolerance was quite good, and only one patient had a significant pleural air leak.
It has also been suggested that an increased risk of postoperative pulmonary complications is associated with lower levels of forced expiratory lung volume and forced vital capacity [65]. Perrin et al. [57] tested the hypothesis of whether a perioperative prophylactic use of NPPV (pre- and postoperatively) produced a better gas exchange and pulmonary function after lung resection compared to oxygen therapy in patients presenting a forced expiratory volume lower than 70% of the predicted. NPPV was initiated 7 days before surgery and was continued postoperatively for 3 days. NPPV was applied for at least five 1-h periods per day. Gas exchange and the spirometric values were significantly better in the NPPV group compared to the control group from day 1 to day 3. The hospital length of stay was significantly lower in the NPPV group (12 ± 1 days) than in the control group (19 ± 3 days).
Therapeutic NPPV
In a randomized trial, Auriant et al. [52] compared the efficacy of bilevel ventilation with standard therapy in patients with acute hypoxemic respiratory insufficiency after lung resection. Patients were enrolled if they presented at least three of the following criteria: respiratory rate higher than 25 breaths per min, active contraction of the accessory respiratory muscles, arterial oxygen ratio lower than 200 mmHg and chest radiographic abnormalities. Two hours after the initiation of treatment, NPPV treatment significantly improved the arterial oxygenation and respiratory rate. Twelve of the 24 patients (50%) in the standard treatment group required invasive mechanical ventilation versus only 5 (20.8%) in the NPPV group. Nine patients in the standard treatment group (37.5%) died versus only three (12.5%) in the bilevel ventilation group (p = 0.045). The mean duration of NPPV was 2.1 ± 2.4 days.
Compared to clinical studies, in a “real life” study over a 4-year period, Lefebvre et al. [67] reported that among 690 patients admitted to intensive care following lung resection, 89 (12.9%) received NPPV. NPPV was applied for hypoxemic acute respiratory failure in 59 patients (66%) and for hypercapnic acute respiratory failure in 30 patients (34%). Initial positive response to NPPV was observed in up to 80% of patients, while NPPV failure occurred in 13 patients (14%) without any difference between hypoxemic or hypercapnic respiratory failure. The average duration of NPPV was 3.4 ± 1.9 days. The mortality rate in the patients who required invasive mechanical ventilation was 46%. The two independent factors significantly associated with NPPV failure were the presence of cardiac comorbidities and the absence of any initial beneficial response.
Thoraco-abdominal vascular surgery
The repair of a thoraco-abdominal aortic aneurysm is a high-risk surgical procedure complicated by intraoperative large high blood losses, incision of the thorax and abdomen, need for elevated blood transfusions and hemodynamic instability.
In a retrospective review of thoraco-abdominal aortic aneurysm repairs, Money et al. [68] reported that 53% of the patients were extubated within 48 h after surgery. Of these patients, 21% developed acute respiratory failure presenting an almost three-fold longer hospital stay (46 days) than patients without acute respiratory failure (16 days).
Svensson et al. [69] reported respiratory problems in up to 60% of the patients that underwent thoraco-abdominal surgery. Postoperative invasive mechanical ventilation was required in about 8% of these patients. The most common reported respiratory complications were atelectasis (37%), pleural effusions (21%) and pneumonia (8%).
Etz et al. [70], in a population of more than 219 patients after aortic aneurysm repair, clearly showed that the need for prolonged respiratory therapy after surgery was associated with a higher mortality rate. Of the 60 patients (27%) who required ventilator support for more than 48 h, 12% died.
Prophylactic CPAP
In a randomized controlled study, Kindgen-Milles et al. [41] evaluated the effects of nasal CPAP continuously delivered for the first 24 h compared to intermittent CPAP plus oxygen therapy in patients following thoraco-abdominal aortic aneurysm repair. When CPAP was applied continuously, it significantly increased the arterial oxygenation. After removing CPAP the oxygenation level was similar in the two groups. The pulmonary complications and the total length of hospital stay were significantly reduced in the group continuously receiving CPAP.
Thoraco-abdominal surgery
Thoraco-abdominal resection for a carcinoma of the esophagus or cardia may present similar respiratory problems to aortic aneurysm repairs. Respiratory efficiency may be further worsened because of the transposition of the stomach into the chest [71]. The rate of respiratory complications after esophago-gastric resection varies between studies, ranging from 8 to 45% [71–73].
Prophylactic CPAP
Seventy patients undergoing thoraco-abdominal resection for carcinoma of the esophagus or cardia were randomized to receive CPAP or an inspiratory resistance-positive expiratory pressure [38]. The two treatments were applied during the first 3 days for 30 min every 2 h. The need for reintubation and prolonged mechanical ventilation was significantly lower in patients treated with CPAP while the gas exchange, lung volumes and clinical outcome were similar between the two groups.
Therapeutic NPPV
In a case control study Michelet et al. [56] compared the efficacy of NPPV with conventional treatment in patients who developed postoperative acute respiratory failure after esophagectomy. Over a 3-year period, 243 patients were admitted to the intensive care unit after surgery, and 84 patients presented acute respiratory failure. Thirty-six of these received NPPV for a mean 6 ± 2 days. NPPV use was associated with a significant reduction in reintubation rate, septic shock and intensive care unit length of stay. No complications, such as major gastric distension or anastomotic leakage, were observed. There was no difference between groups in overall hospital stay or hospital mortality.
Cardiac surgery
Pinilla et al. [45] reported that 40 to 90% of patients undergoing cardiac surgery have pulmonary complications. Possible damage of the phrenic nerve, chest opening, the use of bypass and the use of mammary arteries may further promote postoperative pulmonary impairment [59].
Prophylactic CPAP NPPV
In small series of randomized trials the application of CPAP or NPPV compared to standard treatment with oxygen therapy and chest physiotherapy for a period of 1–12 h significantly improved the gas exchange [45, 48, 49, 59] without any significant difference in the rate of atelectasis [40, 45, 74] or spirometry [45, 74].
Conversely, in a large randomized trial enrolling 468 patients, CPAP significantly reduced the incidence of pulmonary complications (hypoxemia, pneumonia, reintubation rate) compared to oxygen therapy; however, the lengths of stay in the intensive care unit and hospital were similar between groups [49].
Therapeutic CPAP NPPV
One hundred fifty patients who presented a radiological atelectasis score >2 were randomized to receive either CPAP or NPPV four times a day for 30-min sessions [44]. Compared to CPAP, NPPV caused a significantly higher reduction in the radiological atelectasis score with no significant difference in arterial blood gases. The hospital length of stay and the mortality rate were not different between the two groups.
De Morais Coimbra et al. [36] randomized 57 patients presenting acute respiratory failure to receive CPAP or bilevel ventilation. They did not find any statistically significant difference in terms of gas exchange or reduction in the intubation rate among them.
Bariatric surgery
In the largest prospective worldwide database on bariatric surgery, enrolling more than 13,000 patients, acute respiratory failure represented the fourth cause of mortality (11%) [75]. Morbidly obese compared to non-obese patients are characterized by a restrictive syndrome, an increase in chest wall elastance and intra-abdominal pressure, which may promote lung atelectasis [76–79]. Obese patients may also present several respiratory complications such as sleep apnea syndrome [80] and obesity hypoventilation syndrome. These co-morbidities may increase the sensitivity to the anesthetics and opioids, enhancing the risk of acute respiratory failure [81].
Prophylactic CPAP
Neligan et al. [43] evaluated, in 40 morbidly obese patients undergoing laparoscopic gastric bypass surgery, CPAP applied immediately after extubation in the operating room or after 30 min in the post-surgical care unit. In both groups CPAP was applied for a minimum of 8 h. The CPAP significantly preserved lung volume after 1 h and at day 1 after surgery.
A further study showed that CPAP applied after surgery in the post-surgical care unit for 8 h significantly improved arterial oxygenation without any influence on carbon dioxide elimination [39].
Similarly to previous studies, the application of bilevel ventilation during the first 24 h after gastroplasty significantly improved forced vital capacity, forced expiratory volume and arterial saturation compared to oxygen therapy alone [54, 55]. This improvement was maintained after the interruption of the NPPV, leading to a faster recovery of the preoperative spirometric lung volumes.
Some concerns had arisen regarding the use of NIV in postoperative patients because of the possible increase in the intra-luminal pressure of the stomach and intestine, which could promote anastomotic disruptions. A specific study was designated to examine the incidence of anastomotic disruption and respiratory complications [82]. The authors found that only 15 cases of major anastomotic leaks in more than 1,000 postoperative patients; out of these anastomotic leaks, only two of these leaks occurred in patients receiving CPAP. However, these results could not be applied in malnourished patients or in cancer patients undergoing surgery who may present difficulties in wound healing.
Solid organ transplantation
The indications, the number of transplantations and the rate of survival after lung transplantation have improved over the years. However, acute respiratory failure still represents the most frequent cause of postoperative mortality [83, 84].
Therapeutic NPPV
Antonelli et al. [51] randomized 40 recipients of solid organ transplants (i.e., lung, liver and kidney) with hypoxemic acute respiratory failure to NPPV delivered by face mask or to conventional medical treatment. Within the first hour, NPPV significantly improved the oxygenation in 14 patients (70%) versus 5 patients (25%) receiving conventional treatment (25%). This improvement was also observed over time in the patients managed with NPPV. Only 4 patients (20%) of the NPPV group versus 14 patients (70%) of the conventional group required invasive mechanical ventilation. Four patients (20%) compared to ten patients (50%) died in the intensive care unit. In addition, severe sepsis and septic shock developed less frequently in the NPPV group. The 16 survivors in the NPPV group had a shorter length of stay in the intensive care unit than the 10 survivors in the conventional group; however, the hospital mortality rate was not different between groups.
Rocco et al. [58], in an observational study on 21 patients who presented acute respiratory failure after bilateral lung transplantation, reported that NPPV prevented endotracheal intubation in 18 out of 21 treated patients (85%). Fifteen patients showed a sustained improvement, and 19 out of 21 patients (90%) were discharged from the intensive care unit.
Discussion
The objective of this review was to identify the best clinical evidence available on the use of NIV in the perioperative setting. NIV significantly improved arterial blood gas in 19 of the considered studies [33, 34, 36, 38, 39, 41, 45–52, 54, 55, 57–59] and the intubation rate compared to standard medical therapy in 11 of them [34, 36, 38, 41, 47, 49, 51–53, 56, 58]. NIV improved the outcome in only one study [52].
The rationale for using NIV in the postoperative patients depends mainly on the cause of the respiratory failure and whether NIV has to be used therapeutically or just as a preventive tool to avoid respiratory distress. We clearly separated the preventive and therapeutic application of NIV as well as CPAP versus NPPV in order to avoid any misunderstandings in NIV use. Although NIV is defined as any form of ventilatory support applied without ETI [52], NPPV and CPAP are different modes of delivering positive pressure. CPAP delivers a constant airway pressure during all the respiratory cycle while NPPV delivers intermittent inspiratory pressure. CPAP is a spontaneous breathing modality where the pressure applied to the respiratory system is only generated by the respiratory muscles, whereas during NPPV the pressure applied to the respiratory system is generated only by the ventilator (controlled modes) or by the ventilator and the respiratory muscles (assisted modes). NPPV may be delivered as pressure support ventilation with or without positive pressure during the expiration (PEEP) or bilevel ventilation [52].
We considered a therapeutic study, that is, a study that usually includes patients with overt acute respiratory failure, which means the presence of hypoxemia or hypercapnia coupled with signs of respiratory muscle fatigue such as tachypnea. In Squadrone’s study [47], hypoxemia was the only inclusion criteria. For this reason we consider this study neither a study were NIV was used as prophylactic nor a therapeutic tool.
The present review has some limitations. (1) The review process identified data sets on the efficacy of NIV treatment separated by 21 years. Consequently, it would be possible that over this period of time the clinical scenario has changed because of better technology and more accurate diagnostic procedures. (2) The evaluated studies may differ slightly with regard to eligibility criteria and in the methods for delivering CPAP or NPPV. However, we clearly divided the studies that applied CPAP or NPPV. (3) We decided not to perform any meta-analysis evaluating the association of NIV and patient outcomes in abdominal surgery, because of the absence of any new studies since the meta-analysis carried out by Ferreyra et al. [85]. Regarding the other surgical setting (thoracic, thoraco-abdominal, bariatric surgery and solid organ transplantation), only a few studies are available and present great heterogeneity (prophylactic-therapeutic use). This makes data pooling not clinically acceptable.
In conclusion, anesthesia and surgery can profoundly impair respiratory function for several days resulting in PPCs leading to respiratory failure. Despite the limited data and the need for more randomized trials, early administration of NIV should be considered both as a prophylactic and as a therapeutic tool in postoperative patients for improving gas exchange. However, a careful search for any possible surgical complications and the selection of the correct interface (helmet vs. face mask) and type of NIV (CPAP vs. NPPV) together with the individual characteristics of the patients is fundamental for increasing NIV success.
References
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372:139–144
O’Donohue WJ Jr (1992) Postoperative pulmonary complications. When are preventive and therapeutic measures necessary? Postgrad Med 91:167–175
Gardner B, Palasti S (1990) A comparison of hospital costs and morbidity between octogenarians and other patients undergoing general surgical operations. Surg Gynecol Obstet 171:299–304
Arozullah AM, Daley J, Henderson WG, Khuri SF (2000) Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 232:242–253
Harpole DH Jr, DeCamp MM Jr, Daley J, Hur K, Oprian CA, Henderson WG, Khuri SF (1999) Prognostic models of thirty-day mortality and morbidity after major pulmonary resection. J Thorac Cardiovasc Surg 117:969–979
Wong DH, Weber EC, Schell MJ, Wong AB, Anderson CT, Barker SJ (1995) Factors associated with postoperative pulmonary complications in patients with severe chronic obstructive pulmonary disease. Anesth Analg 80:276–284
Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguia C, Gonzalez M, Epstein SK, Hill NS, Nava S, Soares MA, D’Empaire G, Alia I, Anzueto A (2004) Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med 350:2452–2460
Antonelli M, Conti G, Rocco M, Bufi M, De Blasi RA, Vivino G, Gasparetto A, Meduri GU (1998) A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med 339:429–435
Kroenke K, Lawrence VA, Theroux JF, Tuley MR, Hilsenbeck S (1993) Postoperative complications after thoracic and major abdominal surgery in patients with and without obstructive lung disease. Chest 104:1445–1451
Smetana GW (1999) Preoperative pulmonary evaluation. N Engl J Med 340:937–944
Chawla G, Drummond GB (2008) Fentanyl decreases end-expiratory lung volume in patients anaesthetized with sevoflurane. Br J Anaesth 100:411–414
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31:1327–1335
Magnusson L, Spahn DR (2003) New concepts of atelectasis during general anaesthesia. Br J Anaesth 91:61–72
Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR, Magnusson L (2002) Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 95:1788–1792
Ferreyra G, Squadrone V, Ranieri VM (2005) Acute respiratory failure after abdominal surgery. In: Year of intensive care and emergency medicine, 1st edn. Springer, Berlin, pp 10–18
Warner DO (2000) Preventing postoperative pulmonary complications: the role of the anesthesiologist. Anesthesiology 92:1467–1472
Dureuil B, Cantineau JP, Desmonts JM (1987) Effects of upper or lower abdominal surgery on diaphragmatic function. Br J Anaesth 59:1230–1235
Simonneau G, Vivien A, Sartene R, Kunstlinger F, Samii K, Noviant Y, Duroux P (1983) Diaphragm dysfunction induced by upper abdominal surgery. role of postoperative pain. Am Rev Respir Dis 128:899–903
Ingwersen UM, Larsen KR, Bertelsen MT, Kiil-Nielsen K, Laub M, Sandermann J, Bach K, Hansen H (1993) Three different mask physiotherapy regimens for prevention of post-operative pulmonary complications after heart and pulmonary surgery. Intensive Care Med 19:294–298
Kyzer S, Charuzi I (1998) Obstructive sleep apnea in the obese. World J Surg 22:998–1001
Stock MC, Downs JB, Gauer PK, Alster JM, Imrey PB (1985) Prevention of postoperative pulmonary complications with CPAP, incentive spirometry, and conservative therapy. Chest 87:151–157
Evans TW (2001) International Consensus Conferences in Intensive Care Medicine: non-invasive positive pressure ventilation in acute respiratory failure. Organised jointly by the American Thoracic Society, the European Respiratory Society, the European Society of Intensive Care Medicine, and the Societe de Reanimation de Langue Francaise, and approved by the ATS Board of Directors, December 2000. Intensive Care Med 27:166–178
Nava S, Hill N (2009) Non-invasive ventilation in acute respiratory failure. Lancet 374:250–259
British Thoracic Society Standards of Care Committee (2002) Non-invasive ventilation in acute respiratory failure. Thorax 57:192–211
Ferrer M (2008) Non-invasive ventilation in the weaning process. Minerva Anestesiol 74:311–314
Nava S, Navalesi P, Carlucci A (2009) Non-invasive ventilation. Minerva Anestesiol 75:31–36
Ferreyra G, Long Y, Ranieri VM (2009) Respiratory complications after major surgery. Curr Opin Crit Care 15:342–348
Jaber S, Chanques G, Jung B (2010) Postoperative noninvasive ventilation. Anesthesiology 112:453–461
Chanques G, Jaber S, Delay JM, Perrigault PF, Lefrant JY, Eledjam JJ (2003) Phoning study about postoperative practice and application of non-invasive ventilation. Ann Fr Anesth Reanim 22:879–885
Covelli HD, Weled BJ, Beekman JF (1982) Efficacy of continuous positive airway pressure administered by face mask. Chest 81:147–150
Duncan SR, Negrin RS, Mihm FG, Guilleminault C, Raffin TA (1987) Nasal continuous positive airway pressure in atelectasis. Chest 92:621–624
Kindgen-Milles D, Buhl R, Gabriel A, Bohner H, Muller E (2000) Nasal continuous positive airway pressure: a method to avoid endotracheal reintubation in postoperative high-risk patients with severe nonhypercapnic oxygenation failure. Chest 117:1106–1111
Anderes C, Anderes U, Gasser D, Dittmann M, Turner J, Brennwald J, Keller R, Ferstl A, Wolff G (1979) Postoperative spontaneous breathing with CPAP to normalize late postoperative oxygenation. Intensive Care Med 5:15–21
Bohner H, Kindgen-Milles D, Grust A, Buhl R, Lillotte WC, Muller BT, Muller E, Furst G, Sandmann W (2002) Prophylactic nasal continuous positive airway pressure after major vascular surgery: results of a prospective randomized trial. Langenbecks Arch Surg 387:21–26
Carlsson C, Sonden B, Thylen U (1981) Can postoperative continuous positive airway pressure (CPAP) prevent pulmonary complications after abdominal surgery? Intensive Care Med 7:225–229
de Morais Coimbra VR, de Almeida Lara R, Flores EG, Nozawa E, Costa JO, Zanetti MI (2007) Application of noninvasive ventilation in acute respiratory failure after cardiovascular surgery. Arq Bras Cardiol 89:270–276
Denehy L, Carroll S, Ntoumenopoulos G, Jenkins S (2001) A randomized controlled trial comparing periodic mask CPAP with physiotherapy after abdominal surgery. Physiother Res Int 6:236–250
Fagevik Olsèn M, Wennberg E, Johnsson E, Josefson K, Lönroth H, Lundell L (2002) Randomized clinical study of the prevention of pulmonary complications after thoracoabdominal resection by two different breathing techniques. Br J Surg 89:1228–1234
Gaszynski T, Tokarz A, Piotrowski D, Machala W (2007) Boussignac CPAP in the postoperative period in morbidly obese patients. Obes Surg 17:452–456
Jousela I, Rasanen J, Verkkala K, Lamminen A, Makelainen A, Nikki P (1994) Continuous positive airway pressure by mask in patients after coronary surgery. Acta Anaesthesiol Scand 38:311–316
Kindgen-Milles D, Muller E, Buhl R, Bohner H, Ritter D, Sandmann W, Tarnow J (2005) Nasal-continuous positive airway pressure reduces pulmonary morbidity and length of hospital stay following thoracoabdominal aortic surgery. Chest 128:821–828
Lindner KH, Lotz P, Ahnefeld FW (1987) Continuous positive airway pressure effect on functional residual capacity, vital capacity and its subdivisions. Chest 92:66–70
Neligan PJ, Malhotra G, Fraser M, Williams N, Greenblatt EP, Cereda M, Ochroch EA (2009) Continuous positive airway pressure via the Boussignac system immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesthesiology 110:878–884
Pasquina P, Merlani P, Granier JM, Ricou B (2004) Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesth Analg 99:1001–1008, table
Pinilla JC, Oleniuk FH, Tan L, Rebeyka I, Tanna N, Wilkinson A, Bharadwaj B (1990) Use of a nasal continuous positive airway pressure mask in the treatment of postoperative atelectasis in aortocoronary bypass surgery. Crit Care Med 18:836–840
Ricksten SE, Bengtsson A, Soderberg C, Thorden M, Kvist H (1986) Effects of periodic positive airway pressure by mask on postoperative pulmonary function. Chest 89:774–781
Squadrone V, Coha M, Cerutti E, Schellino MM, Biolino P, Occella P, Belloni G, Vilianis G, Fiore G, Cavallo F, Ranieri VM (2005) Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA 293:589–595
Thomas AN, Ryan JP, Doran BR, Pollard BJ (1992) Nasal CPAP after coronary artery surgery. Anaesthesia 47:316–319
Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D (2009) Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: a prospective, randomized, controlled trial in 500 patients. Chest 135:1252–1259
Aguilo R, Togores B, Pons S, Rubi M, Barbe F, Agusti AG (1997) Noninvasive ventilatory support after lung resectional surgery. Chest 112:117–121
Antonelli M, Conti G, Bufi M, Costa MG, Lappa A, Rocco M, Gasparetto A, Meduri GU (2000) Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA 283:235–241
Auriant I, Jallot A, Herve P, Cerrina J, Le Roy LF, Fournier JL, Lescot B, Parquin F (2001) Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med 164:1231–1235
Conti G, Cavaliere F, Costa R, Craba A, Catarci S, Festa V, Proietti R, Antonelli M (2007) Noninvasive positive-pressure ventilation with different interfaces in patients with respiratory failure after abdominal surgery: a matched-control study. Respir Care 52:1463–1471
Ebeo CT, Benotti PN, Byrd RP Jr, Elmaghraby Z, Lui J (2002) The effect of bi-level positive airway pressure on postoperative pulmonary function following gastric surgery for obesity. Respir Med 96:672–676
Joris JL, Sottiaux TM, Chiche JD, Desaive CJ, Lamy ML (1997) Effect of bi-level positive airway pressure (BiPAP) nasal ventilation on the postoperative pulmonary restrictive syndrome in obese patients undergoing gastroplasty. Chest 111:665–670
Michelet P, D’Journo XB, Seinaye F, Forel JM, Papazian L, Thomas P (2009) Non-invasive ventilation for treatment of postoperative respiratory failure after oesophagectomy. Br J Surg 96:54–60
Perrin C, Jullien V, Venissac N, Berthier F, Padovani B, Guillot F, Coussement A, Mouroux J (2007) Prophylactic use of noninvasive ventilation in patients undergoing lung resectional surgery. Respir Med 101:1572–1578
Rocco M, Conti G, Antonelli M, Bufi M, Costa MG, Alampi D, Ruberto F, Stazi GV, Pietropaoli P (2001) Non-invasive pressure support ventilation in patients with acute respiratory failure after bilateral lung transplantation. Intensive Care Med 27:1622–1626
Matte P, Jacquet L, Van Dyck M, Goenen M (2000) Effects of conventional physiotherapy, continuous positive airway pressure and non-invasive ventilatory support with bilevel positive airway pressure after coronary artery bypass grafting. Acta Anaesthesiol Scand 44:75–81
Jaber S, Delay JM, Chanques G, Sebbane M, Jacquet E, Souche B, Perrigault PF, Eledjam JJ (2005) Outcomes of patients with acute respiratory failure after abdominal surgery treated with noninvasive positive pressure ventilation. Chest 128:2688–2695
Ginsberg RJ, Hill LD, Eagan RT, Thomas P, Mountain CF, Deslauriers J, Fry WA, Butz RO, Goldberg M, Waters PF (1983) Modern thirty-day operative mortality for surgical resections in lung cancer. J Thorac Cardiovasc Surg 86:654–658
Patel RL, Townsend ER, Fountain SW (1992) Elective pneumonectomy: factors associated with morbidity and operative mortality. Ann Thorac Surg 54:84–88
Keagy BA, Lores ME, Starek PJ, Murray GF, Lucas CL, Wilcox BR (1985) Elective pulmonary lobectomy: factors associated with morbidity and operative mortality. Ann Thorac Surg 40:349–352
Harpole DH, Liptay MJ, DeCamp MM Jr, Mentzer SJ, Swanson SJ, Sugarbaker DJ (1996) Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann Thorac Surg 61:977–982
Kutlu CA, Williams EA, Evans TW, Pastorino U, Goldstraw P (2000) Acute lung injury and acute respiratory distress syndrome after pulmonary resection. Ann Thorac Surg 69:376–380
Sen S, Sen S, Senturk E, Kuman NK (2010) Postresectional lung injury in thoracic surgery pre and intraoperative risk factors: a retrospective clinical study of a hundred forty-three cases. J Cardiothorac Surg 5:62
Lefebvre A, Lorut C, Alifano M, Dermine H, Roche N, Gauzit R, Regnard JF, Huchon G, Rabbat A (2009) Noninvasive ventilation for acute respiratory failure after lung resection: an observational study. Intensive Care Med 35:663–670
Money SR, Rice K, Crockett D, Becker M, Abdoh A, Wisselink W, Kazmier F, Hollier L (1994) Risk of respiratory failure after repair of thoracoabdominal aortic aneurysms. Am J Surg 168:152–155
Svensson LG, Hess KR, Coselli JS, Safi HJ, Crawford ES (1991) A prospective study of respiratory failure after high-risk surgery on the thoracoabdominal aorta. J Vasc Surg 14:271–282
Etz CD, Di Luozzo G, Bello R, Luehr M, Khan MZ, Bodian CA, Griepp RB, Plestis KA (2007) Pulmonary complications after descending thoracic and thoracoabdominal aortic aneurysm repair: predictors, prevention, and treatment. Ann Thorac Surg 83:S870–S876
Bishop DG, McKeown KC (1979) Postoperative hypoxaemia: oesophagectomy with gastric replacement. Br J Surg 66:810–812
Black J, Kalloor GJ, Collis JL (1977) The effect of the surgical approach on respiratory function after oesophageal resection. Br J Surg 64:624–627
Crozier TA, Sydow M, Siewert JR, Braun U (1992) Postoperative pulmonary complication rate and long-term changes in respiratory function following esophagectomy with esophagogastrostomy. Acta Anaesthesiol Scand 36:10–15
Stock MC, Downs JB, Cooper RB, Lebenson IM, Cleveland J, Weaver DE, Alster JM, Imrey PB (1984) Comparison of continuous positive airway pressure, incentive spirometry, and conservative therapy after cardiac operations. Crit Care Med 12:969–972
Morino M, Toppino M, Forestieri P, Angrisani L, Allaix ME, Scopinaro N (2007) Mortality after bariatric surgery: analysis of 13, 871 morbidly obese patients from a national registry. Ann Surg 246:1002–1007
Ogunnaike BO, Jones SB, Jones DB, Provost D, Whitten CW (2002) Anesthetic considerations for bariatric surgery. Anesth Analg 95:1793–1805
Pelosi P, Croci M, Ravagnan I, Vicardi P, Gattinoni L (1996) Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest 109:144–151
Pelosi P, Croci M, Ravagnan I, Cerisara M, Vicardi P, Lissoni A, Gattinoni L (1997) Respiratory system mechanics in sedated, paralyzed, morbidly obese patients. J Appl Physiol 82:811–818
Pelosi P, Croci M, Ravagnan I, Tredici S, Pedoto A, Lissoni A, Gattinoni L (1998) The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg 87:654–660
Chung SA, Yuan H, Chung F (2008) A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg 107:1543–1563
Ahmad S, Nagle A, McCarthy RJ, Fitzgerald PC, Sullivan JT, Prystowsky J (2008) Postoperative hypoxemia in morbidly obese patients with and without obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesth Analg 107:138–143
Huerta S, DeShields S, Shpiner R, Li Z, Liu C, Sawicki M, Arteaga J, Livingston EH (2002) Safety and efficacy of postoperative continuous positive airway pressure to prevent pulmonary complications after Roux-en-Y gastric bypass. J Gastrointest Surg 6:354–358
Cooper JD, Patterson GA, Trulock EP (1994) Results of single and bilateral lung transplantation in 131 consecutive recipients. Washington University Lung Transplant Group. J Thorac Cardiovasc Surg 107:460–470
Shapiro BJ, Veeraraghavan S, Barbers RG (1999) Lung transplantation for cystic fibrosis: an update and practical considerations for referring candidates. Curr Opin Pulm Med 5:365–370
Ferreyra GP, Baussano I, Squadrone V, Richiardi L, Marchiaro G, Del Sorbo L, Mascia L, Merletti F, Ranieri VM (2008) Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg 247:617–626
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiumello, D., Chevallard, G. & Gregoretti, C. Non-invasive ventilation in postoperative patients: a systematic review. Intensive Care Med 37, 918–929 (2011). https://doi.org/10.1007/s00134-011-2210-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2210-8