Abstract
Summary
Change of microenvironment pH by biodegradable implants may ameliorate unbalanced osteoporotic bone remodeling. The present work demonstrated that a weak alkaline condition stimulated osteoblasts differentiation while suppressed osteoclast generation. In vivo, implants with an alkaline microenvironment pH (monitored by a pH microelectrode) exhibited a promising healing effect for the repair of osteoporotic bone defects.
Introduction
Under osteoporotic conditions, the response of the bone microenvironment to an endosseous implant is significantly impaired, and this substantially increases the risk of fracture, non-union and aseptic implant loosening. Acid-base equilibrium is an important factor influencing bone cell behaviour. The present purpose was to study the effect of a series of alkaline biodegradable implant materials on regeneration of osteoporotic bone defect, monitoring the microenvironment pH (μe-pH) over time.
Methods
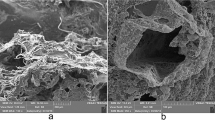
The proliferation and differentiation potential of osteoporotic rat bone marrow stromal cells and RAW 264.7 cells were examined under various pH conditions. Ovariectomized rat bone defects were filled with specific biodegradable materials, and μe-pH was measured by pH microelectrode. New osteoid and tartrate-resistant acid phosphatase-positive osteoclast-like cells were examined by Goldner’s trichrome and TRAP staining, respectively. The intermediate layer between implants and new bone were studied using energy-dispersive X-ray spectroscopy (EDX) linear scanning.
Results
In vitro, weak alkaline conditions stimulated osteoporotic rat bone marrow stromal cells (oBMSC) differentiation, while inhibiting the formation of osteoclasts. In vivo, μe-pH differs from that of the homogeneous peripheral blood and exhibits variations over time particular to each material. Higher initial μe-pH was associated with more new bone formation, late response of TRAP-positive osteoclast-like cells and the development of an intermediate ‘apatitic’ layer in vivo. EDX suggested that residual material may influence μe-pH even 9 weeks post-surgery.
Conclusion
The pH microelectrode is suitable for in vivo μe-pH detection. Alkaline biodegradable materials generate an in vivo microenvironmental pH which is higher than the normal physiological value and show promising healing effects in the context of osteoporotic bone defects.






Similar content being viewed by others
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Feng X, McDonald JM (2011) Disorders of bone remodeling. Annu Rev Pathol 6:121–145
Arcos D, Boccaccini AR, Bohner M, Diez-Perez A, Epple M, Gomez-Barrena E et al (2014) The relevance of biomaterials to the prevention and treatment of osteoporosis. Acta Biomater 10:1793–1805
Delmas PD (2002) Treatment of postmenopausal osteoporosis. Lancet 359:2018–2026
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet 348:1535–1541
Bushinsky DA (2001) Acid–base imbalance and the skeleton. Eur J Nutr 40:238–244
Brandao-Burch A, Utting JC, Orriss IR, Arnett TR (2005) Acidosis inhibits bone formation by osteoblasts in vitro by preventing mineralization. Calcif Tissue Int 77:167–174
Bushinsky DA (1996) Metabolic alkalosis decreases bone calcium efflux by suppressing osteoclasts and stimulating osteoblasts. Am J Physiol 271:F216–F222
Kaunitz JD, Yamaguchi DT (2008) TNAP, TrAP, Ecto-purinergic signaling, and bone remodeling. J Cell Biochem 105:655–662
Harada M, Udagawa N, Fukasawa K, Hiraoka BY, Mogi M (1986) Inorganic pyrophosphatase activity of purified bovine pulp alkaline phosphatase at physiological pH. J Dent Res 65:125–127
Shen YH, Liu WC, Lin KL, Pan HB, Darvell BW, Peng SL et al (2011) Interfacial pH: a critical factor for osteoporotic bone regeneration. Langmuir 27:2701–2708
Shen YH, Liu WC, Wen CY, Pan HB, Wang T, Darvell BW et al (2012) Bone regeneration: importance of local pH-strontium-doped borosilicate scaffold. J Mater Chem 22:8662–8670
Hench LL (2006) The story of Bioglass (R). J Mater Sci-Mater Med 17:967–978
Zhang WB, Shen YH, Pan HB, Lin KL, Liu XG, Darvell BW et al (2011) Effects of strontium in modified biomaterials. Acta Biomater 7:800–808
Ciapetti G, Cenni E, Pratelli L, Pizzoferrato A (1993) In vitro evaluation of cell/biomaterial interaction by MTT assay. Biomaterials 14:359–364
Nilsson B, Korsgren O, Lambris JD, Ekdahl KN (2010) Can cells and biomaterials in therapeutic medicine be shielded from innate immune recognition? Trends Immunol 31:32–38
Gorbet MB, Sefton MV (2004) Biomaterial-associated thrombosis: roles of coagulation factors, complement, platelets and leukocytes. Biomaterials 25:5681–5703
Korostynska O, Arshak K, Gill E, Arshak A (2008) Review paper: materials and techniques for in vivo pH monitoring. IEEE Sensors J 8:20–28
Zhou DD (2008) Microelectrodes for in-vivo determination of pH. In: Zhang XJ, Ju HX, Wang J (eds) Electrochemical sensors, biosensors and their biomedical applications. Academic Press, USA, pp 261–305
Pandolfino JE, Ghosh S, Zhang Q, Heath M, Bombeck T, Kahrilas PJ (2006) Slimline vs. glass pH electrodes: what degree of accuracy should we expect? Aliment Pharmacol Ther 23:331–340
Ruan CM, Zeng KF, Grimes CA (2003) A mass-sensitive pH sensor based on a stimuli-responsive polymer. Anal Chim Acta 497:123–131
Bock C, Sartoris FJ, Wittig RM, Portner HO (2001) Temperature-dependent pH regulation in stenothermal Antarctic and eurythermal temperate eelpout (Zoarcidae): an in-vivo NMR study. Polar Biol 24:869–874
Lee H, Akers W, Bhushan K, Bloch S, Sudlow G, Tang R et al (2011) Near-infrared pH-activatable fluorescent probes for imaging primary and metastatic breast tumors. Bioconjug Chem 22:777–784
Zhang XM, Lin YX, Gillies RJ (2010) Tumor pH and its measurement. J Nucl Med 51:1167–1170
Bartsch I, Willbold E, Rosenhahn B, Witte F (2014) Non-invasive pH determination adjacent to degradable biomaterials in vivo. Acta Biomater 10:34–39
Chakkalakal DA, Mashoof AA, Novak J, Strates BS, McGuire MH (1994) Mineralization and pH relationships in healing skeletal defects grafted with demineralized bone matrix. J Biomed Mater Res 28:1439–1443
Xu S, Lin K, Wang Z, Chang J, Wang L, Lu J et al (2008) Reconstruction of calvarial defect of rabbits using porous calcium silicate bioactive ceramics. Biomaterials 29:2588–2596
Zhu H, Guo ZK, Jiang XX, Li H, Wang XY, Yao HY et al (2010) A protocol for isolation and culture of mesenchymal stem cells from mouse compact bone. Nat Protoc 5:550–560
Lelovas PP, Xanthos TT, Thoma SE, Lyritis GP, Dontasi IA (2008) The laboratory rat as an animal model for osteoporosis research. Comp Med 58:424–430
Westendorf JJ (2008) Osteoporosis: methods and protocols. Humana Press, Totowa
An YH, Martin KL (2003) Handbook of histology methods for bone and cartilage. Humana Press, Totowa
Kadoya Y, al-Saffar N, Kobayashi A, Revell PA (1994) The expression of osteoclast markers on foreign body giant cells. Bone Miner 27:85–96
Kato K, Matsushita M (2014) Proton concentrations can be a major contributor to the modification of osteoclast and osteoblast differentiation, working independently of extracellular bicarbonate ions. J Bone Miner Metab 32:17–28
Shibutani T, Heersche JNM (1993) Effect of medium-pH on osteoclast activity and osteoclast formation in cultures of dispersed rabbit osteoclasts. J Bone Miner Res 8:331–336
Arnett T (2003) Regulation of bone cell function by acid–base balance. Proc Nutr Soc 62:511–520
Kohn DH, Sarmadi M, Helman JI, Krebsbach PH (2002) Effects of pH on human bone marrow stromal cells in vitro: implications for tissue engineering of bone. J Biomed Mater Res 60:292–299
Kaysinger KK, Ramp WK (1998) Extracellular pH modulates the activity of cultured human osteoblasts. J Cell Biochem 68:83–89
Arnett TR (2008) Extracellular pH regulates bone cell function. J Nutr 138:415S–418S
Ross MH, Ely JO, Archer JG (1951) Alkaline phosphatase activity and pH optima. J Biol Chem 192:561–568
Harrison DK, Walker WF (1979) Microelectrode measurement of skin pH in humans during ischemia, hypoxia and local hypothermia. J Physiol Lond 291:339–350
Jahde E, Rajewsky MF, Baumgartl H (1982) pH distributions in transplanted neural tumors and normal-tissues of BDIX rats as measured with pH microelectrodes. Cancer Res 42:1498–1504
Henderson RM, Bell PB, Cohen RD, Browning C, Iles RA (1986) Measurement of intracellular pH with microelectrodes in rat-kidney in vivo. Am J Physiol 250:F203–F209
Roach P, Eglin D, Rohde K, Perry CC (2007) Modern biomaterials: a review—bulk properties and implications of surface modifications. J Mater Sci Mater Med 18:1263–1277
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (No. 51272274, 51372170), the Development of Strategic Emerging Industries of the Shenzhen Basic Research Project (No. JCYJ20120617120444409), the Shenzhen Peacock Program (No. 110811003586331), Shenzhen Key Laboratory of Marine Biomedical Materials, ZDS (No. Y20130401165820356) and Hong Kong General Research Fund (No. 172057/14).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Wenlong Liu, Ting Wang and Chun Yang contributed equally to this work.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Supplementary Fig. S1
(DOCX 827 kb)
Supplementary Table S1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Liu, W., Wang, T., Yang, C. et al. Alkaline biodegradable implants for osteoporotic bone defects—importance of microenvironment pH. Osteoporos Int 27, 93–104 (2016). https://doi.org/10.1007/s00198-015-3217-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3217-8