Abstract
Summary
Low body mass index (BMI) is an established risk factor for fractures in postmenopausal women but the interaction of obesity with bone microarchitecture is not fully understood. In this study, obesity was associated with more favourable bone microarchitecture parameters but not after parameters were normalised for body weight.
Introduction
To examine bone microarchitecture in relation to fat mass and examine both areal bone mineral density (aBMD) and microarchitecture in relation to BMI categories in the UK arm of the Global Longitudinal Study of Osteoporosis in Women.
Methods
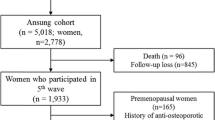
Four hundred and ninety-one women completed questionnaires detailing medical history; underwent anthropometric assessment; high-resolution peripheral quantitative computed tomography (HRpQCT) scans of the radius and tibia and DXA scans of whole body, proximal femur and lumbar spine. Fat mass index (FMI) residuals (independent of lean mass index) were derived. Linear regression was used to examine HRpQCT and DXA aBMD parameters according to BMI category (unadjusted) and HRpQCT parameters in relation to FMI residuals (with and without adjustment for anthropometric, demographic and lifestyle covariates).
Results
Mean (SD) age was 70.9 (5.4) years; 35.0% were overweight, 14.5% class 1 obese and 7.7% class 2/3 obese. There were significant increasing trends according to BMI category in aBMD of whole body, hip, femoral neck and lumbar spine (p ≤ 0.001); cortical area (p < 0.001), thickness (p < 0.001) and volumetric density (p < 0.03), and trabecular number (p < 0.001), volumetric density (p < 0.04) and separation (p < 0.001 for decreasing trend) at the radius and tibia. When normalised for body weight, all HRpQCT and DXA aBMD parameters decreased as BMI increased (p < 0.001). FMI residuals were associated with bone size and trabecular architecture at the radius and tibia, and tibial cortical microarchitecture.
Conclusion
Significant trends in HRpQCT parameters suggested favourable bone microarchitecture at the radius and tibia with increasing BMI but these were not proportionate to increased weight.
Similar content being viewed by others
References
(1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. In: The American Journal of Medicine. pp 646–650
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8. https://doi.org/10.1007/s11657-013-0136-1
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:4–9. https://doi.org/10.1016/j.bone.2005.11.024
US Department of Health and Human Services (2004) Bone health and osteoporosis: a report of the Surgeon General. US Heal Hum Serv 32:219–228. https://doi.org/10.2165/00002018-200932030-00004
Van Staa TP, Dennison EM, Leufkens HGM, Cooper C (2001) Epidemiology of fractures in England and Wales. Bone 29:517–522. https://doi.org/10.1016/S8756-3282(01)00614-7
Burge R, Dawson-Hughes B, Solomon DH et al (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. https://doi.org/10.1359/jbmr.061113
De Laet C, Kanis JA, Odén A et al (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338. https://doi.org/10.1007/s00198-005-1863-y
Compston JE, Watts NB, Chapurlat R et al (2011) Obesity is not protective against fracture in postmenopausal women: Glow. Am J Med. https://doi.org/10.1016/j.amjmed.2011.06.013
Beck TJ, Petit MA, Wu G et al (2009) Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone Miner Res. https://doi.org/10.1359/jbmr.090307
Prieto-Alhambra D, Premaor MO, Fina Avilés F et al (2012) The association between fracture and obesity is site-dependent: A population-based study in postmenopausal women. J Bone Miner Res. https://doi.org/10.1002/jbmr.1466
Premaor MO, Pilbrow L, Tonkin C et al (2010) Obesity and fractures in postmenopausal women. J Bone Miner Res. https://doi.org/10.1359/jbmr.091004
Gnudi S, Sitta E, Lisi L (2009) Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab. https://doi.org/10.1007/s00774-009-0056-8
Sornay-Rendu E, Boutroy S, Vilayphiou N et al (2013) In obese postmenopausal women, bone microarchitecture and strength are not commensurate to greater body weight: The OS des femmes de Lyon (OFELY) study. J Bone Miner Res. https://doi.org/10.1002/jbmr.1880
Friedman AW (2006) Important determinants of bone strength: beyond bone mineral density. J Clin Rheumatol 12:70–77. https://doi.org/10.1353/psg.2006.0122
Pollock NK, Laing EM, Baile CA et al (2007) Is adiposity advantageous for bone strength? A peripheral quantitative computed tomography study in late adolescent females. Am J Clin Nutr. https://doi.org/10.1093/ajcn/86.5.1530
Farr JN, Chen Z, Lisse JR et al (2010) Relationship of total body fat mass to weight-bearing bone volumetric density, geometry, and strength in young girls. Bone. https://doi.org/10.1016/j.bone.2009.12.033
Edwards MH, Ward KA, Ntani G et al (2015) Lean mass and fat mass have differing associations with bone microarchitecture assessed by high resolution peripheral quantitative computed tomography in men and women from the Hertfordshire Cohort Study. Bone. https://doi.org/10.1016/j.bone.2015.07.013
Gibbs JC, Giangregorio LM, Wong AKO et al (2017) Appendicular and whole body lean mass outcomes are associated with finite element analysis-derived bone strength at the distal radius and tibia in adults aged 40 years and older. Bone. https://doi.org/10.1016/j.bone.2017.06.006
Evans AL, Paggiosi MA, Eastell R, Walsh JS (2015) Bone density, microstructure and strength in obese and normal weight men and women in younger and older adulthood. J Bone Miner Res 30:920–928. https://doi.org/10.1002/jbmr.2407
Hooven FH, Adachi JD, Adami S et al (2009) The Global Longitudinal Study of Osteoporosis in Women (GLOW): Rationale and study design. Osteoporos Int. https://doi.org/10.1007/s00198-009-0958-2
Pialat JB, Burghardt AJ, Sode M, Link TM, Majumdar S (2012) Visual grading of motion induced image degradation in high resolution peripheral computed tomography: impact of image quality on measures of bone density and micro-architecture. Bone 50:111–118. https://doi.org/10.1016/j.bone.2011.10.003
Burghardt AJ, Kazakia GJ, Ramachandran S, Link TM, Majumdar S (2010) Age- and gender-related differences in the geometric properties and biomechanical significance of intracortical porosity in the distal radius and tibia. J Bone Miner Res 25:983–993. https://doi.org/10.1359/jbmr.091104
Morin S, Leslie WD (2009) High bone mineral density is associated with high body mass index. Osteoporos Int 20:1267–1271. https://doi.org/10.1007/s00198-008-0797-6
Pesonen J, Sirola J, Tuppurainen M, Jurvelin J, Alhava E, Honkanen R, Kr H (2005) High bone mineral density among perimenopausal women. Osteoporos Int 16:1899–1906. https://doi.org/10.1007/s00198-005-1958-5
Nielson CM, Bouxsein ML, Freitas SS, Ensrud KE, Orwoll ES, for the Osteoporotic Fractures in Men (MrOS) Research Group (2009) Trochanteric soft tissue thickness and hip fracture in older men. J Clin Endocrinol Metab 94:491–496. https://doi.org/10.1210/jc.2008-1640
Sukumar D, Schlussel Y, Riedt CS, Gordon C, Stahl T, Shapses SA (2011) Obesity alters cortical and trabecular bone density and geometry in women. Osteoporos Int 22:635–645. https://doi.org/10.1007/s00198-010-1305-3
Mitrou P, Lambadiari V, Maratou E et al (2011) Skeletal muscle insulin resistance in morbid obesity: The role of interleukin-6 and leptin. Exp Clin Endocrinol Diabetes. https://doi.org/10.1055/s-0030-1269846
Thomas T, Burguera B (2002) Is leptin the link between fat and bone mass? J Bone Miner Res. https://doi.org/10.1359/jbmr.2002.17.9.1563
Kawai M, Devlin MJ, Rosen CJ (2009) Fat targets for skeletal health. Nat Rev Rheumatol 5(7):365–372
Gomez R, Lago F, Gomez-Reino J et al (2009) Adipokines in the skeleton: Influence on cartilage function and joint degenerative diseases. J Mol Endocrinol 43(1):11–18
Gómez-Ambrosi J, Rodríguez A, Catalán V, Frühbeck G (2008) The bone-adipose axis in obesity and weight loss. Obes Surg 18(9):1134–1143
Schett G (2011) Effects of inflammatory and anti-inflammatory cytokines on the bone. Eur J Clin Invest 41(12):1361–1366
Wellen KE, Hotamisligil GS (2005) Inflammation, stress, and diabetes. J Clin Invest 115(5):1111–1119
Fain JN, Madan AK, Hiler ML et al (2004) Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology. https://doi.org/10.1210/en.2003-1336
Fain JN (2006) Release of interleukins and other inflammatory cytokines by human adipose tissue is enhanced in obesity and primarily due to the nonfat cells. Vitam Horm
Perneger TV (1998) What’s wrong with Bonferroni adjustments. Br Med J 316:1236–1238
Availability of data and material
Not applicable.
Funding
We thank the Arthritis Research UK for their support: Arthritis Research UK grant number 20380.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A.E. Litwic, L.D. Westbury and K.A. Ward declare that they have no conflict of interest. C Cooper reports personal fees (outside the submitted work) from Amgen, Danone, Eli Lilly, GSK, Kyowa Kirin, Medtronic, Merck, Nestle, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB. EM Dennison reports personal fees (outside the submitted work) from Pfizer Healthcare and UCB.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Litwic, A., Westbury, L., Ward, K. et al. Adiposity and bone microarchitecture in the GLOW study. Osteoporos Int 32, 689–698 (2021). https://doi.org/10.1007/s00198-020-05603-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05603-w