Abstract
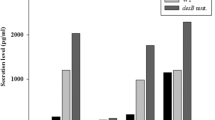
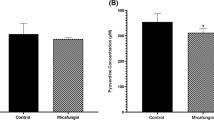
Pseudomonas aeruginosa is a Gram-negative opportunistic pathogen that causes serious infections in humans, notably cystic fibrosis. P. aeruginosa faces various stresses such as oxidative stress either in the environment or within the host during infection. In the present study, the influence of oxidative stress on both Pseudomonas antibiotic susceptibility and host pathogenesis was characterized. Prior exposure to H2O2 significantly altered P. aeruginosa susceptibility to tested antibiotics; colistin, ciprofloxacin, tobramycin, and ceftazidime. The minimum inhibitory concentrations (MICs) of tested antibiotics either increased or decreased following H2O2 exposure. Importantly, RT-qPCR revealed that expression of quorum sensing genes, that regulate virulence factors production in P. aeruginosa, was significantly higher in unstressed relative to H2O2-stressed cells. The impact of P. aeruginosa exposure to oxidative stress by H2O2 on bacterial pathogenesis was investigated using in vivo mice infection model. Interestingly, exposure to oxidative stress markedly reduces P. aeruginosa pathogenesis in mice. Unstressed P. aeruginosa was able to kill more mice as compared to H2O2-stressed bacteria. In addition, body weight of mice infected with unstressed P. aeruginosa was lower than that of mice inoculated with stressed bacteria. Isolated organs (spleen, liver, and kidney) from mice infected with unstressed bacteria exhibited increased weight as well as bacterial load in comparison with mice infected with stressed bacteria. In summary, current data highlight the impact of oxidative stress on P. aeruginosa antibiotic susceptibility as well as host pathogenesis. These findings could be helpful in treatment of infections caused by this important pathogen.






Similar content being viewed by others
References
Filiatrault MJ, Picardo KF, Ngai H, Passador L, Iglewski BH (2006) Identification of Pseudomonas aeruginosa genes involved in virulence and anaerobic growth. Infect Immunity 74(7):4237–4245
Strateva T, Yordanov D (2009) Pseudomonas aeruginosa: a phenomenon of bacterial resistance. J Med Microbiol 58(9):1133–1148
Moreau-Marquis S, Bomberger JM, Anderson GG, SwiateckaUrban A, Ye S, O'Toole GA, Stanton BA (2008) The ΔF508-CFTR mutation results in increased biofilm formation by Pseudomonas aeruginosa by increasing iron availability. Am J Physiol-Lung Cell Mol Physiol 295(1):L25–L37
Stover C, Pham X, Erwin A, Mizoguchi S, Warrener P, Hickey M, Brinkman F, Hufnagle W, Kowalik D, Lagrou M (2000) Complete genome sequence of Pseudomonas aeruginosa PAO1, an opportunistic pathogen. Nature 406(6799):959
Zhou JW, Luo HZ, Jiang H, Jian TK, Chen ZQ, Jia AQ (2018) Hordenine: a novel quorum sensing inhibitor and antibiofilm agent against Pseudomonas aeruginosa. J Agric Food Chem 66(7):1620–1628. https://doi.org/10.1021/acs.jafc.7b05035
Jimenez PN, Koch G, Thompson JA, Xavier KB, Cool RH, Quax WJ (2012) The multiple signaling systems regulating virulence in Pseudomonas aeruginosa. Microbiol Mol Biol Rev 76(1):46–65
Lister PD, Wolter DJ, Hanson ND (2009) Antibacterial-resistant Pseudomonas aeruginosa: clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clin Microbiol Rev 22(4):582–610. https://doi.org/10.1128/cmr.00040-09
Gill EE, Franco OL, Hancock RE (2015) Antibiotic adjuvants: diverse strategies for controlling drug-resistant pathogens. Chem Biol Drug Des 85(1):56–78
McMahon MA, Xu J, Moore JE, Blair IS, McDowell DA (2007) Environmental stress and antibiotic resistance in food-related pathogens. Appl Environ Microbiol 73(1):211–217. https://doi.org/10.1128/AEM.00578-06
AlNabulsi AA, Osaili TM, Elabedeen NAZ, Jaradat ZW, Shaker RR, Kheirallah KA, Tarazi YH, Holley RA (2011) Impact of environmental stress desiccation, acidity, alkalinity, heat or cold on antibiotic susceptibility of Cronobacter sakazakii. Int J Food Microbiol 146(2):137–143
Yousef AE, Courtney PD (2003) Basics of stress adaptation and implications in new generation food. In: Yousef AE, Juneja VK (eds) Microbial stress adaptation and food safety. CRC Press, Boca Raton, Florida, pp 1–30
Bower CK, Daeschel MA (1999) Resistance responses of microorganisms in food environments. Int J Food Microbiol 50(1–2):33–44
Storz G, Imlayt JA (1999) Oxidative stress. Curr Opin Microbiol 2(2):188–194
Khakimova M, Ahlgren HG, Harrison JJ, English AM, Nguyen D (2013) The stringent response controls catalases in Pseudomonas aeruginosa and is required for hydrogen peroxide and antibiotic tolerance. J Bacteriol 195(9):2011–2020. https://doi.org/10.1128/jb.02061-12
Moradali MF, Ghods S, Rehm BHA (2017) Pseudomonas aeruginosa lifestyle: a paradigm for adaptation, survival, and persistence. Front Cell Infect Microbiol. https://doi.org/10.3389/fcimb.2017.00039
Poole K (2012) Bacterial stress responses as determinants of antimicrobial resistance. J Antimicrob Chemother 67(9):2069–2089. https://doi.org/10.1093/jac/dks196
Koneman E PG, Schreckenberger P, Woods G, Winnw W, Allen S, Janda W (2006) Koneman'scolor atlas and textbook of diagnostic microbiology, 6th ed. Lippincott Williams and willkins, Philadelphia, Baltimore, New York, London
Jorgensen JH, Ferraro MJ (2009) Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin Infect Dis 49(11):1749–1755. https://doi.org/10.1086/647952
Saleh MM, Abbas HA, Askoura MM (2019) Repositioning secnidazole as a novel virulence factors attenuating agent in Pseudomonas aeruginosa. Microb Pathog 127:31–38. https://doi.org/10.1016/j.micpath.2018.11.042
Lee S, Hinz A, Bauerle E, Angermeyer A, Juhaszova K, Kaneko Y, Singh PK, Manoil C (2009) Targeting a bacterial stress response to enhance antibiotic action. Proc Natl Acad Sci USA 106(34):14570–14575. https://doi.org/10.1073/pnas.0903619106
Kobayashi F (1971) Experimental infection with Pseudomonas aeruginosa in mice. II. The fate of highly and low virulent strains in the peritoneal cavity and organs of mice. Jpn J Microbiol 15(4):301–307
Weng Y, Chen F, Liu Y, Zhao Q, Chen R, Pan X, Liu C, Cheng Z, Jin S, Jin Y, Wu W (2016) Pseudomonas aeruginosa enolase influences bacterial tolerance to oxidative stresses and virulence. Front Microbiol 7:1999. https://doi.org/10.3389/fmicb.2016.01999
Poole K (2012) Stress responses as determinants of antimicrobial resistance in Gram-negative bacteria. Trends Microbiol 20(5):227–234
Small DA, Chang W, Toghrol F, Bentley WE (2007) Comparative global transcription analysis of sodium hypochlorite, peracetic acid, and hydrogen peroxide on Pseudomonas aeruginosa. Appl Microbiol Biotechnol 76(5):1093–1105. https://doi.org/10.1007/s00253-007-1072-z
Lan L, Murray TS, Kazmierczak BI, He C (2010) Pseudomonas aeruginosa OspR is an oxidative stress sensing regulator that affects pigment production, antibiotic resistance and dissemination during infection. Mol Microbiol 75(1):76–91
Hengge-Aronis R (2000) The general stress response in Escherichia coli. Bacterial stress responses
Rowan NJ (1999) Evidence that inimical food-preservation barriers alter microbial resistance, cell morphology and virulence. Trends Food Sci Technol 10(8):261–270
Katzif S, Danavall D, Bowers S, Balthazar JT, Shafer WM (2003) The major cold shock gene, cspA, is involved in the susceptibility of Staphylococcus aureus to an antimicrobial peptide of human cathepsin G. Infect Immun 71(8):4304–4312
Alekshun MN, Levy SB (1997) Regulation of chromosomally mediated multiple antibiotic resistance: the mar regulon. Antimicrob Agents Chemother 41(10):2067
Hannum DM, Barrette WC Jr, Hurst JK (1995) Subunit sites of oxidative inactivation of Escherichia coli F1-ATPase by HOCl. Biochem Biophys Res Commun 212(3):868–874
Velkov VV (1999) How environmental factors regulate mutagenesis and gene transfer in microorganisms. J Biosci 24(4):529–559
Jolivet-Gougeon A, David-Jobert S, Tamanai-Shacoori Z, Ménard C, Cormier M (2000) Osmotic stress-induced genetic rearrangements in Escherichia coli H10407 detected by randomly amplified polymorphic DNA analysis. Appl Environ Microbiol 66(12):5484–5487
Foster PL (2000) Adaptive mutation: implications for evolution. BioEssays 22(12):1067–1074
Poole K (2008) Bacterial multidrug efflux pumps serve other functions. Microbe 3(4):179
Lipus D, Vikram A, Gulliver D, Bibby K (2019) Upregulation of peroxide scavenging enzymes and multidrug efflux proteins highlight an active sodium hypochlorite response in Pseudomonas fluorescens biofilms. Biofouling 35(3):329–339. https://doi.org/10.1080/08927014.2019.1605357
Ishiguro EE, Ramey WD (1980) Inhibition of in vitro peptidoglycan biosynthesis in Escherichia coli by guanosine 5′-diphosphate 3′-diphosphate. Can J Microbiol 26(12):1514–1518
Wu J, Long Q, Xie J (2010) (p) ppGpp and drug resistance. J Cell Physiol 224(2):300–304
Landini P (2009) Cross-talk mechanisms in biofilm formation and responses to environmental and physiological stress in Escherichia coli. Res Microbiol 160(4):259–266
Tan X, Qin N, Wu C, Sheng J, Yang R, Zheng B, Ma Z, Liu L, Peng X, Jia A (2015) Transcriptome analysis of the biofilm formed by methicillin-susceptible Staphylococcus aureus. Sci Rep 5:11997. https://doi.org/10.1038/srep11997
Strempel N, Nusser M, Neidig A, Brenner-Weiss G, Overhage J (2017) The oxidative stress agent hypochlorite stimulates c-di-GMP synthesis and biofilm formation in Pseudomonas aeruginosa. Front Microbiol 8:2311. https://doi.org/10.3389/fmicb.2017.02311
Gunn JS (2001) Bacterial modification of LPS and resistance to antimicrobial peptides. J Endotoxin Res 7(1):57–62
Kato A, Groisman EA (2008) The PhoQ/PhoP regulatory network of Salmonella enterica. In: Bacterial signal transduction: networks and drug targets. Springer, Berlin, pp 7–21
Meehl M, Herbert S, Götz F, Cheung A (2007) Interaction of the GraRS two-component system with the VraFG ABC transporter to support vancomycin-intermediate resistance in Staphylococcus aureus. Antimicrob Agents Chemother 51(8):2679–2689. https://doi.org/10.1128/AAC.00209-07
Eng RH, Padberg FT, Smith SM, Tan EN, Cherubin CE (1991) Bactericidal effects of antibiotics on slowly growing and nongrowing bacteria. Antimicrob Agents Chemother 35(9):1824–1828. https://doi.org/10.1128/aac.35.9.1824
Proctor RA, von Eiff C, Kahl BC, Becker K, McNamara P, Herrmann M, Peters G (2006) Small colony variants: a pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat Rev Microbiol 4(4):295–305. https://doi.org/10.1038/nrmicro1384
Lewis K (2010) Persister cells. Annu Rev Microbiol 64:357–372. https://doi.org/10.1146/annurev.micro.112408.134306
Miller C, Thomsen LE, Gaggero C, Mosseri R, Ingmer H, Cohen SN (2004) SOS response induction by beta-lactams and bacterial defense against antibiotic lethality. Science (New York, NY) 305(5690):1629–1631. https://doi.org/10.1126/science.1101630
Morita Y, Sobel ML, Poole K (2006) Antibiotic inducibility of the MexXY multidrug efflux system of Pseudomonas aeruginosa: involvement of the antibiotic-inducible PA5471 gene product. J Bacteriol 188(5):1847–1855. https://doi.org/10.1128/JB.188.5.1847-1855.2006
El-Mowafy SA, El Galil KHA, El-Messery SM, Shaaban MI (2014) Aspirin is an efficient inhibitor of quorum sensing, virulence and toxins in Pseudomonas aeruginosa. Microb Pathog 74:25–32
Kiratisin P, Tucker KD, Passador L (2002) LasR, a transcriptional activator of Pseudomonas aeruginosa virulence genes, functions as a multimer. J Bacteriol 184(17):4912–4919. https://doi.org/10.1128/jb.184.17.4912-4919.2002
El-Mowafy SA, Shaaban MI, Abd El Galil KH (2014) Sodium ascorbate as a quorum sensing inhibitor of Pseudomonas aeruginosa. J Appl Microbiol 117(5):1388–1399. https://doi.org/10.1111/jam.12631
Albrich JM, Gilbaugh JH 3rd, Callahan KB, Hurst JK (1986) Effects of the putative neutrophil-generated toxin, hypochlorous acid, on membrane permeability and transport systems of Escherichia coli. J Clin Investig 78(1):177–184. https://doi.org/10.1172/jci112548
Dahl J-U, Gray MJ, Jakob U (2015) Protein quality control under oxidative stress conditions. J Mol Biol 427(7):1549–1563
Halliwell B (1994) Free radicals, antioxidants, and human disease: curiosity, cause, or consequence? The lancet 344(8924):721–724
Imlay JA (2008) Cellular defenses against superoxide and hydrogen peroxide. Annu Rev Biochem 77:755–776
Imlay JA (2013) The molecular mechanisms and physiological consequences of oxidative stress: lessons from a model bacterium. Nat Rev Microbiol 11(7):443–454. https://doi.org/10.1038/nrmicro3032
Bonvillain RW, Painter RG, Ledet EM, Wang G (2011) Comparisons of resistance of CF and non-CF pathogens to hydrogen peroxide and hypochlorous acid oxidants in vitro. BMC Microbiol 11(1):112
Winter J, Ilbert M, Graf P, Özcelik D, Jakob U (2008) Bleach activates a redox-regulated chaperone by oxidative protein unfolding. Cell 135(4):691–701
Winterbourn CC (2008) Reconciling the chemistry and biology of reactive oxygen species. Nat Chem Biol 4(5):278
Mead J (1976) In Free radicals in, biology edn. Academic Press, New York, WA Pryor
Demple B, Linn S (1982) 5, 6-Saturated thymine lesions in DNA: production by ultraviolet light or hydrogen peroxide. Nucleic Acids Res 10(12):3781–3789
Levin DE, Hollstein M, Christman MF, Schwiers EA, Ames BN (1982) A new Salmonella tester strain (TA102) with A X T base pairs at the site of mutation detects oxidative mutagens. Proc Natl Acad Sci USA 79(23):7445–7449. https://doi.org/10.1073/pnas.79.23.7445
Chandler JD, Day BJ (2015) Biochemical mechanisms and therapeutic potential of pseudohalide thiocyanate in human health. Free Radic Res 49(6):695–710
Lau GW, Ran H, Kong F, Hassett DJ, Mavrodi D (2004) Pseudomonas aeruginosa pyocyanin is critical for lung infection in mice. Infect Immun 72(7):4275–4278
Lau GW, Hassett DJ, Ran H, Kong F (2004) The role of pyocyanin in Pseudomonas aeruginosa infection. Trends Mol Med 10(12):599–606
Rodriguez-Rojas A, Mena A, Martin S, Borrell N, Oliver A, Blazquez J (2009) Inactivation of the hmgA gene of Pseudomonas aeruginosa leads to pyomelanin hyperproduction, stress resistance and increased persistence in chronic lung infection. Microbiology (Reading, England) 155(Pt 4):1050–1057. https://doi.org/10.1099/mic.0.024745-0
Xia T, Kovochich M, Brant J, Hotze M, Sempf J, Oberley T, Sioutas C, Yeh JI, Wiesner MR, Nel AE (2006) Comparison of the abilities of ambient and manufactured nanoparticles to induce cellular toxicity according to an oxidative stress paradigm. Nano Lett 6(8):1794–1807
Author information
Authors and Affiliations
Contributions
MMA and GHS conceived and designed the experiments; FAM performed the experiments; MMA designed the tables & figures, interpreted the results, analyzed the data and wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in animal study were in accordance with the ethical standards of The Institutional Animal Care and Use Committee, Zagazig University (ZU-IACUC) with approval number ZU-IACUC3/F/138/2019. All animals were handled according to guidelines from the Animal Ethics Board (Zagazig University). All participants provided written informed consent prior to enrolment in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohamed, F.A., Shaker, G.H. & Askoura, M.M. Oxidative Stress Influences Pseudomonas aeruginosa Susceptibility to Antibiotics and Reduces Its Pathogenesis in Host. Curr Microbiol 77, 479–490 (2020). https://doi.org/10.1007/s00284-019-01858-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-019-01858-7