Abstract
Background
Prasugrel is a potent thienopyridine that may be preferentially used in younger patients with lower bleeding risk.
Objective
We compared prasugrel use and outcomes by age from the PROMETHEUS study. We also assessed age-related trends in treatment effects with prasugrel versus clopidogrel.
Methods
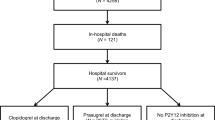
PROMETHEUS was a multicenter acute coronary syndrome (ACS) percutaneous coronary intervention (PCI) registry. We compared patients in age tertiles (T1 < 60 years, T2 60–70 years, T3 > 70 years). Major adverse cardiac events (MACE) were a composite of death, myocardial infarction, stroke or unplanned revascularization. Data were adjusted using multivariable Cox regression for age-related risks and propensity score stratification for thienopyridine effects.
Results
The study included 19,914 patients: 7045 (35.0%) in T1, 6489 (33.0%) in T2 and 6380 (32.0%) in T3. Prasugrel use decreased from T1 to T3 (29.2% vs. 23.5% vs. 7.5%, p < 0.001). Crude 1-year MACE rates were highest in T3 (17.4% vs. 16.8% vs. 22.7%, p < 0.001), but adjusted risk was similar between the groups (p-trend 0.52). Conversely, crude incidence (2.8% vs. 3.8% vs. 6.9%, p < 0.001) and adjusted bleeding risk were highest in T3 (HR 1.24, 95% CI 0.99–1.55 in T2; HR 1.83, 95% CI 1.46–2.30 in T3; p-trend < 0.001; reference = T1). Treatment effects with prasugrel versus clopidogrel did not demonstrate age-related trends for MACE (p-trend = 0.91) or bleeding (p-trend = 0.28).
Conclusions
Age is a strong determinant of clinical risk as well as prasugrel prescription in ACS PCI with much lower use among older patients. Prasugrel did not have a differential treatment effect by age for MACE or bleeding.
Graphic abstract
Frequency of prasugrel use and age-related temporal risks of all-cause death and bleeding after ACS PCI.




Similar content being viewed by others
References
Wang TY, Gutierrez A, Peterson ED (2011) Percutaneous coronary intervention in the elderly. Nat Rev Cardiol 8:79–90
Wimmer NJ, Resnic FS, Mauri L et al (2013) Risk-treatment paradox in the selection of transradial access for percutaneous coronary intervention. J Am Heart Assoc 2:e000174
Motivala AA, Cannon CP, Srinivas VS et al (2011) Changes in myocardial infarction guideline adherence as a function of patient risk: an end to paradoxical care? J Am Coll Cardiol 58:1760–1765
Ko DT, Mamdani M, Alter DA (2004) Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA 291:1864–1870
Levine GN, Bates ER, Bittl JA et al (2016) 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Thorac Cardiovasc Surg 152:1243–1275
Wiviott SD, Braunwald E, McCabe CH et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Rasania SP, Chamaria S, Vengrenyuk Y et al (2017) Percutaneous coronary intervention outcomes in very elderly patients from a single large-volume tertiary care center, specifically focusing on nonagenarians. JACC Cardiovasc Interv 10:1273–1274
Sawant AC, Josey K, Plomondon ME et al (2017) Temporal trends, complications, and predictors of outcomes among nonagenarians undergoing percutaneous coronary intervention: insights from the veterans affairs clinical assessment, reporting, and tracking program. JACC Cardiovasc Interv 10:1295–1303
Baber U, Sartori S, Aquino M et al (2017) Use of prasugrel vs clopidogrel and outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention in contemporary clinical practice: results from the PROMETHEUS study. Am Heart J 188:73–81
NIH. https://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically. 2016
Khera S, Kolte D, Gupta T et al (2015) Temporal trends and sex differences in revascularization and outcomes of st-segment elevation myocardial infarction in younger adults in the United States. J Am Coll Cardiol 66:1961–1972
Gupta A, Wang Y, Spertus JA et al (2014) Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 64:337–345
Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA (2004) Barriers to health care access among the elderly and who perceives them. Am J Public Health 94:1788–1794
Mathews R, Peterson ED, Honeycutt E et al (2015) Early medication nonadherence after acute myocardial infarction: insights into actionable opportunities from the treatment with adp receptor inhibitors: longitudinal assessment of treatment patterns and events after acute coronary syndrome (TRANSLATE-ACS) study. Circ Cardiovasc Qual Outcomes 8:347–356
Gellad WF, Grenard JL, Marcum ZA (2011) A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother 9:11–23
Cheng K, Ingram N, Keenan J, Choudhury RP (2015) Evidence of poor adherence to secondary prevention after acute coronary syndromes: possible remedies through the application of new technologies. Open Heart 2:e000166
Ansell J (2017) Stroke prevention in atrial fibrillation in the very elderly: anticoagulant therapy is no longer a sin. J Am Heart Assoc 6:e006864
Sandhu A, Seth M, Dixon S et al (2013) Contemporary use of prasugrel in clinical practice: insights from the blue cross blue shield of michigan cardiovascular consortium. Circ Cardiovasc Qual Outcomes 6:293–298
Alexopoulos D, Xanthopoulou I, Plakomyti TE et al (2013) Pharmacodynamic effect of prasugrel 5 mg vs clopidogrel 150 mg in elderly patients with high on-clopidogrel platelet reactivity. Am Heart J 165:73–79
Erlinge D, Gurbel PA, James S et al (2013) Prasugrel 5 mg in the very elderly attenuates platelet inhibition but maintains noninferiority to prasugrel 10 mg in nonelderly patients: the GENERATIONS trial, a pharmacodynamic and pharmacokinetic study in stable coronary artery disease patients. J Am Coll Cardiol 62:577–583
Erlinge D, Ten Berg J, Foley D et al (2012) Reduction in platelet reactivity with prasugrel 5 mg in low-body-weight patients is noninferior to prasugrel 10 mg in higher-body-weight patients: results from the FEATHER trial. J Am Coll Cardiol 60:2032–2040
Ferri LA, Morici N, Grosseto D et al (2016) A comparison of reduced-dose prasugrel and standard-dose clopidogrel in elderly patients with acute coronary syndromes undergoing early percutaneous revascularization: design and rationale of the randomized Elderly-ACS 2 study. Am Heart J 181:101–106
Savonitto S, Ferri LA, Piatti L et al (2018) Comparison of reduced-dose prasugrel and standard-dose clopidogrel in elderly patients with acute coronary syndromes undergoing early percutaneous revascularization. Circulation 137:2435–2445
Qaderdan K, Ishak M, Heestermans AA et al (2015) Ticagrelor or prasugrel versus clopidogrel in elderly patients with an acute coronary syndrome: optimization of antiplatelet treatment in patients 70 years and older–rationale and design of the POPular AGE study. Am Heart J 170(981):985
Funding
The PROMETHEUS study was sponsored and funded by Daiichi Sankyo, Inc. and Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chandrasekhar, J., Baber, U., Sartori, S. et al. Prasugrel use and clinical outcomes by age among patients undergoing PCI for acute coronary syndrome: from the PROMETHEUS study. Clin Res Cardiol 109, 725–734 (2020). https://doi.org/10.1007/s00392-019-01561-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01561-4