Abstract
Purpose
Evolutionary discordance may contribute to the high burden of chronic disease-related mortality in modern industrialized nations. We aimed to investigate the associations of a 7-component, equal-weight, evolutionary-concordance lifestyle (ECL) score with all-cause and cause-specific mortality.
Methods
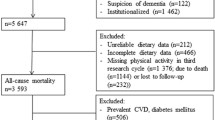
Baseline data were collected in 2003–2007 from 17,465 United States participants in the prospective REasons for Geographic and Racial Differences in Stroke (REGARDS) study. The ECL score’s components were: a previously reported evolutionary-concordance diet score, alcohol intake, physical activity, sedentary behavior, waist circumference, smoking history, and social network size. Diet was assessed using a Block 98 food frequency questionnaire and anthropometrics by trained personnel; other information was self-reported. Higher scores indicated higher evolutionary concordance. We used multivariable Cox proportional hazards regression models to estimate ECL score–mortality associations.
Results
Over a median follow-up of 10.3 years, 3771 deaths occurred (1177 from cardiovascular disease [CVD], 1002 from cancer). The multivariable-adjusted hazard ratios (HR) (95% confidence intervals [CI]) for those in the highest relative to the lowest ECL score quintiles for all-cause, all-CVD, and all-cancer mortality were, respectively, 0.45 (0.40, 0.50), 0.47 (0.39, 0.58), and 0.42 (0.34, 0.52) (all P trend < 0.01). Removing smoking and diet from the ECL score attenuated the estimated ECL score–all-cause mortality association the most, yielding fifth quintile HRs (95% CIs) of 0.56 (0.50, 0.62) and 0.50 (0.46, 0.55), respectively.
Conclusions
Our findings suggest that a more evolutionary-concordant lifestyle may be inversely associated with all-cause, all-CVD, and all-cancer mortality. Smoking and diet appeared to have the greatest impact on the ECL–mortality associations.


Similar content being viewed by others
Data availability
This study uses data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort. In order to abide by its obligations with NIH/NINDS and the Institutional Review Board of the University of Alabama at Birmingham, REGARDS facilitates data sharing through formal data use agreements. Any investigator is welcome to access the REGARDS data through this process. Requests for data access may be sent to regardsadmin@uab.edu.
Code availability
The code supporting this current study is available from the corresponding author upon request.
Abbreviations
- 95% CI:
-
95% Confidence intervals
- CVD:
-
Cardiovascular disease
- ECL:
-
Evolutionary-concordance lifestyle
- HR:
-
Hazard ratios
- REGARDS:
-
REasons for Geographic and Racial Differences in Stroke
- US:
-
United States
References
Global status report on non-communicable diseases 2010 (2011) World Health Organization, Geneva
Global health risks: mortality and burden of disease attributable to selected major risks (2009) World Health Organization, Geneva
Konner M, Eaton SB (2010) Paleolithic nutrition: twenty-five years later. Nutr Clin Pract 25:594–602. https://doi.org/10.1177/0884533610385702
Eaton SB, Konner M (1985) Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med 312:283–289. https://doi.org/10.1056/NEJM198501313120505
Eaton SB, Konner M, Shostak M (1988) Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective. Am J Med 84:739–749. https://doi.org/10.1016/0002-9343(88)90113-1
Eaton SB, Shostak M, Konner M (1989) The paleolithic prescription: a program of diet & exercise and a design for living. Harper & Row, New York
Ghaedi E, Mohammadi M, Mohammadi H et al (2019) Effects of a paleolithic diet on cardiovascular disease risk factors: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 10:634–646. https://doi.org/10.1093/advances/nmz007
de Menezes EVA, de Sampaio HAC, Carioca AAF et al (2019) Influence of Paleolithic diet on anthropometric markers in chronic diseases: systematic review and meta-analysis. Nutr J 18:41. https://doi.org/10.1186/s12937-019-0457-z
Whalen KA, McCullough ML, Flanders WD et al (2016) Paleolithic and mediterranean diet pattern scores are inversely associated with biomarkers of inflammation and oxidative balance in adults. J Nutr 146:1217–1226. https://doi.org/10.3945/jn.115.224048
Whalen KA, McCullough M, Flanders WD et al (2014) Paleolithic and Mediterranean diet pattern scores and risk of incident, sporadic colorectal adenomas. Am J Epidemiol 180:1088–1097. https://doi.org/10.1093/aje/kwu235
Whalen KA, Judd S, McCullough ML et al (2017) Paleolithic and Mediterranean diet pattern scores are inversely associated with all-cause and cause-specific mortality in adults. J Nutr 147:612–620. https://doi.org/10.3945/jn.116.241919
Cheng E, Um CY, Prizment AE et al (2018) Evolutionary-concordance lifestyle and diet and mediterranean diet pattern scores and risk of incident colorectal cancer in Iowa women. Cancer Epidemiol Biomarkers Prev 27:1195–1202. https://doi.org/10.1158/1055-9965.EPI-17-1184
Cheng E, Um CY, Prizment A et al (2018) Associations of evolutionary-concordance diet, Mediterranean diet and evolutionary-concordance lifestyle pattern scores with all-cause and cause-specific mortality. Br J Nutr. https://doi.org/10.1017/S0007114518003483
Katzmarzyk PT (2010) Physical activity, sedentary behavior, and health: paradigm paralysis or paradigm shift? Diabetes 59:2717–2725. https://doi.org/10.2337/db10-0822
Brewer MB (2004) Taking the social origins of human nature seriously: toward a more imperialist social psychology. Personal Soc Psychol Rev 8:107–113. https://doi.org/10.1207/s15327957pspr0802_3
Umberson D, Montez JK (2010) Social relationships and health: a flashpoint for health policy. J Health Soc Behav 51(Suppl):S54-66. https://doi.org/10.1177/0022146510383501
Howard VJ, Cushman M, Pulley L et al (2005) The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 25:135–143. https://doi.org/10.1159/000086678
American Association for Public Opinion Research (2004) Standard definitions: final dispositions of case codes and outcome rates for surveys, 3rd edition. merican Association for Public Opinion Research, Lenexa, KS
Howard VJ, Kleindorfer DO, Judd SE et al (2011) Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol 69:619–627. https://doi.org/10.1002/ana.22385
Boucher B, Cotterchio M, Kreiger N et al (2006) Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr 9:84–93. https://doi.org/10.1079/phn2005763
Block G, Hartman AM, Dresser CM et al (1986) A data-based approach to diet questionnaire design and testing. Am J Epidemiol 124:453–469. https://doi.org/10.1093/oxfordjournals.aje.a114416
NutritionQuest Questionnaires and Screeners—Assessment & Analysis Services—NutritionQuest. https://nutritionquest.com/assessment/list-of-questionnaires-and-screeners/. Accessed 12 Nov 2020
Washburn RA, Adams LL, Haile GT (1987) Physical activity assessment for epidemiologic research: the utility of two simplified approaches. Prev Med 16:636–646. https://doi.org/10.1016/0091-7435(87)90047-8
Washburn RA, Goldfield SR, Smith KW, McKinlay JB (1990) The validity of self-reported exercise-induced sweating as a measure of physical activity. Am J Epidemiol 132:107–113. https://doi.org/10.1093/oxfordjournals.aje.a115622
Del Boca FK, Darkes J (2003) The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction 98(Suppl 2):1–12. https://doi.org/10.1046/j.1359-6357.2003.00586.x
Del Boca FK, Noll JA (2000) Truth or consequences: the validity of self-report data in health services research on addictions. Addiction 95(Suppl 3):S347-360. https://doi.org/10.1080/09652140020004278
Salmon J, Owen N, Crawford D et al (2003) Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol 22:178–188. https://doi.org/10.1037//0278-6133.22.2.178
Berkman LF, Syme SL (1979) Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109:186–204. https://doi.org/10.1093/oxfordjournals.aje.a112674
Halanych JH, Shuaib F, Parmar G et al (2011) Agreement on cause of death between proxies, death certificates, and clinician adjudicators in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Am J Epidemiol 173:1319–1326. https://doi.org/10.1093/aje/kwr033
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Austin PC, Lee DS, Fine JP (2016) Introduction to the analysis of survival data in the presence of competing risks. Circulation 133:601–609. https://doi.org/10.1161/CIRCULATIONAHA.115.017719
Fine J, Gray R (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Ding D, Rogers K, van der Ploeg H et al (2015) Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: evidence from a large population-based Australian cohort. PLoS Med 12:e1001917. https://doi.org/10.1371/journal.pmed.1001917
Petersen KEN, Johnsen NF, Olsen A et al (2015) The combined impact of adherence to five lifestyle factors on all-cause, cancer and cardiovascular mortality: a prospective cohort study among Danish men and women. Br J Nutr 113:849–858. https://doi.org/10.1017/S0007114515000070
Prinelli F, Yannakoulia M, Anastasiou CA et al (2015) Mediterranean diet and other lifestyle factors in relation to 20-year all-cause mortality: a cohort study in an Italian population. Br J Nutr 113:1003–1011. https://doi.org/10.1017/S0007114515000318
Ford ES, Bergmann MM, Boeing H et al (2012) Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med 55:23–27. https://doi.org/10.1016/j.ypmed.2012.04.016
Yun JE, Won S, Kimm H, Jee SH (2012) Effects of a combined lifestyle score on 10-year mortality in Korean men and women: a prospective cohort study. BMC Public Health 12:673. https://doi.org/10.1186/1471-2458-12-673
Carlsson AC, Wändell PE, Gigante B et al (2013) Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all-cause mortality regardless of body mass index: a cohort study. Int J Cardiol 168:946–952. https://doi.org/10.1016/j.ijcard.2012.10.045
Veronese N, Li Y, Manson JE et al (2016) Combined associations of body weight and lifestyle factors with all cause and cause specific mortality in men and women: prospective cohort study. BMJ 355:i5855. https://doi.org/10.1136/bmj.i5855
Lee I, Kim S, Kang H (2019) Lifestyle risk factors and all-cause and cardiovascular disease mortality: data from the Korean Longitudinal Study of Aging. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16173040
Behrens G, Fischer B, Kohler S et al (2013) Healthy lifestyle behaviors and decreased risk of mortality in a large prospective study of U.S. women and men. Eur J Epidemiol 28:361–372. https://doi.org/10.1007/s10654-013-9796-9
Bonaccio M, Di Castelnuovo A, Costanzo S et al (2019) Impact of combined healthy lifestyle factors on survival in an adult general population and in high-risk groups: prospective results from the Moli-sani Study. J Intern Med 286:207–220. https://doi.org/10.1111/joim.12907
Li Y, Pan A, Wang DD et al (2018) Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138:345–355. https://doi.org/10.1161/CIRCULATIONAHA.117.032047
Larsson SC, Kaluza J, Wolk A (2017) Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Intern Med 282:209–219. https://doi.org/10.1111/joim.12637
Loef M, Walach H (2012) The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 55:163–170. https://doi.org/10.1016/j.ypmed.2012.06.017
Zhang Y-B, Pan X-F, Chen J et al (2020) Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. Br J Cancer. https://doi.org/10.1038/s41416-020-0741-x
CDCTobaccoFree (2018) 2014 SGR: The health consequences of smoking—50 Years of Progress. In: Cent Dis Control Prev. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm. Accessed 11 Apr 2020
Jha P, Ramasundarahettige C, Landsman V et al (2013) 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med 368:341–350. https://doi.org/10.1056/NEJMsa1211128
Schwingshackl L, Schwedhelm C, Hoffmann G et al (2017) Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 105:1462–1473. https://doi.org/10.3945/ajcn.117.153148
Liu RH (2013) Health-promoting components of fruits and vegetables in the diet. Adv Nutr 4:384S-S392. https://doi.org/10.3945/an.112.003517
Lampe JW (1999) Health effects of vegetables and fruit: assessing mechanisms of action in human experimental studies. Am J Clin Nutr 70:475S-490S. https://doi.org/10.1093/ajcn/70.3.475s
Demeyer D, Mertens B, De Smet S, Ulens M (2016) Mechanisms linking colorectal cancer to the consumption of (processed) red meat: a review. Crit Rev Food Sci Nutr 56:2747–2766. https://doi.org/10.1080/10408398.2013.873886
Centers for Disease Control and Prevention (US), National Center for Chronic Disease Prevention and Health Promotion (US), Office on Smoking and Health (US) (2010) How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. 1, Introduction, evaluation of evidence on mechanisms of disease production, and summary. Centers for Disease Control and Prevention (US), Atlanta, GA
Kyrou I, Randeva HS, Tsigos C et al (2000) Clinical problems caused by obesity. In: Feingold KR, Anawalt B, Boyce A, et al (eds) Endotext. MDText.com, Inc., South Dartmouth (MA)
Golemis EA, Scheet P, Beck TN et al (2018) Molecular mechanisms of the preventable causes of cancer in the United States. Genes Dev 32:868–902. https://doi.org/10.1101/gad.314849.118
Silverman MN, Deuster PA (2014) Biological mechanisms underlying the role of physical fitness in health and resilience. Interface Focus. https://doi.org/10.1098/rsfs.2014.0040
Patterson R, McNamara E, Tainio M et al (2018) Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 33:811–829. https://doi.org/10.1007/s10654-018-0380-1
Ekelund U, Steene-Johannessen J, Brown WJ et al (2016) Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388:1302–1310. https://doi.org/10.1016/S0140-6736(16)30370-1
Smith KP, Christakis NA (2008) Social networks and health. Ann Rev Sociol 34:405–429. https://doi.org/10.1146/annurev.soc.34.040507.134601
Funding
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service, and by R01 HL80477 from the National Heart Lung and Blood Institute (NHLBI). Additional funding was provided by The Anne and Wilson P. Franklin Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS, NIA, NHLBI, or The Anne and Wilson P. Franklin Foundation. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were conducted by SJ. Data analysis was performed by ANT. The first draft of the manuscript was written by ANT and all authors commented on previous versions of the manuscript. RMB provided supervision and had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Flanders owns “Epidemiologic Research & Methods, LLC” which does some consulting work for a variety of clients. He knows of no conflicts of interest. All other authors have no conflicts of interest to disclose.
Ethical approval
The institutional review boards of all participating institutions approved the study.
Informed consent to participate
All participants gave written, informed consent at enrollment.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Troeschel, A.N., Hartman, T.J., Flanders, W.D. et al. A novel evolutionary-concordance lifestyle score is inversely associated with all-cause, all-cancer, and all-cardiovascular disease mortality risk. Eur J Nutr 60, 3485–3497 (2021). https://doi.org/10.1007/s00394-021-02529-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02529-9