Abstract
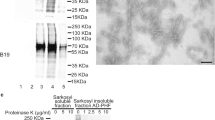
In Alzheimer’s disease (AD), tau-protein undergoes a multi-step process involving the transition from a natively unfolded monomer to large, aggregated structures such as neurofibrillary tangles (NFTs). However, it is not yet clear which events initiate the early preclinical phase of AD tauopathy and whether they have impact on the propagation of tau pathology in later disease stages. To address this question, we analyzed the distribution of tau species phosphorylated at T231, S396/S404 and S202/T205, conformationally modified at the MC1 epitope and fibrillary tau detected by the Gallyas method (Gallyas-tau), in the brains of 15 symptomatic and 20 asymptomatic cases with AD pathology as well as of 19 nonAD cases. As initial tau lesions, we identified phosphorylated-T231-tau diffusely distributed within the somatodendritic compartment (IC-tau) and phosphorylated-S396/pS404-tau in axonal lesions of the white matter and in the neuropil (IN-tau). The subcellular localization of pT231-tau in the cell body and pS396/pS404-tau in the presynapse was confirmed in hP301L mutant Drosophila larvae. Phosphorylated-S202/T205-tau, MC1-tau and Gallyas-tau were negative for these lesions. IC- and IN-tau were observed in all analyzed regions of the human brain, including early affected regions in nonAD cases (entorhinal cortex) and late affected regions in symptomatic AD cases (cerebellum), indicating that tau pathology initiation follows similar processes when propagating into previously unaffected regions. Furthermore, a sequence of AD-related maturation of tau-aggregates was observed, initiated by the appearance of IC- and IN-tau, followed by the formation of pretangles exhibiting pT231-tau, pS396/pS404-tau and pS202/pT205-tau, then by MC1-conformational tau, and, finally, by the formation of Gallyas-positive NFTs. Since cases classified as nonAD [Braak NFT stages < I (including a-1b)] already showed IC- and IN-tau, our findings suggest that these lesions are a prerequisite for the development of AD.





Similar content being viewed by others
References
Alafuzoff I, Arzberger T, Al-Sarraj S, Bodi I, Bogdanovic N, Braak H et al (2008) Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe consortium. Brain Pathol 18:484–496. https://doi.org/10.1111/j.1750-3639.2008.00147.x
Alafuzoff I, Pikkarainen M, Al-Sarraj S, Arzberger T, Bell J, Bodi I et al (2006) Interlaboratory comparison of assessments of Alzheimer disease-related lesions: a study of the BrainNet Europe consortium. J Neuropathol Exp Neurol 65:740–757. https://doi.org/10.1097/01.jnen.0000229986.17548.27
Arendt T, Stieler J, Strijkstra AM, Hut RA, Rüdiger J, Van der Zee EA et al (2003) Reversible paired helical filament-like phosphorylation of tau is an adaptive process associated with neuronal plasticity in hibernating animals. J Neurosci 23:6972–6981. https://doi.org/10.1523/jneurosci.23-18-06972.2003
Augustinack JC, Schneider A, Mandelkow EM, Hyman BT (2002) Specific tau phosphorylation sites correlate with severity of neuronal cytopathology in Alzheimer’s disease. Acta Neuropathol 103:26–35. https://doi.org/10.1007/s004010100423
Ballatore C, Lee VMY, Trojanowski JQ (2007) Tau-mediated neurodegeneration in Alzheimer’s disease and related disorders. Nat Rev Neurosci 8:663–672
Bancher C, Brunner C, Lassmann H, Budka H, Jellinger K, Wiche G et al (1989) Accumulation of abnormally phosphorylated τ precedes the formation of neurofibrillary tangles in Alzheimer’s disease. Brain Res 477:90–99. https://doi.org/10.1016/0006-8993(89)91396-6
Braak E, Braak H, Mandelkow EM (1994) A sequence of cytoskeleton changes related to the formation of neurofibrillary tangles and neuropil threads. Acta Neuropathol 87:554–567. https://doi.org/10.1007/BF00293315
Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Tredici K (2006) Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol 112:389–404. https://doi.org/10.1007/s00401-006-0127-z
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259
Braak H, Braak E (1991) Demonstration of amyloid deposits and neurofibrillary changes in whole brain sections. Brain Pathol 1:213–216. https://doi.org/10.1111/j.1750-3639.1991.tb00661.x
Braak H, Thal DR, Ghebremedhin E, Del Tredici K (2011) Stages of the pathologic process in alzheimer disease: age categories from 1 to 100 years. J Neuropathol Exp Neurol 70:960–969. https://doi.org/10.1097/NEN.0b013e318232a379
Braak H, Del Tredici K (2011) The pathological process underlying Alzheimer’s disease in individuals under thirty. Acta Neuropathol 121:171–181. https://doi.org/10.1007/s00401-010-0789-4
Braak H, Del Tredici K, Rüb U, De Vos RAI, Jansen Steur ENH, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211. https://doi.org/10.1016/S0197-4580(02)00065-9
Brettschneider J, Del Tredici K, Lee VMY, Trojanowski JQ (2015) Spreading of pathology in neurodegenerative diseases: a focus on human studies. Nat Rev Neurosci 16:109–120
De Calignon A, Polydoro M, Suárez-Calvet M, William C, Adamowicz DH, Kopeikina KJ et al (2012) Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron 73:685–697. https://doi.org/10.1016/j.neuron.2011.11.033
Chapuis J, Hansmannel F, Gistelinck M, Mounier A, Van Cauwenberghe C, Kolen KV et al (2013) Increased expression of BIN1 mediates Alzheimer genetic risk by modulating tau pathology. Mol Psychiatry 18:1225–1234. https://doi.org/10.1038/mp.2013.1
Corbett GT, Wang Z, Hong W, Colom-Cadena M, Rose J, Liao M et al (2020) PrP is a central player in toxicity mediated by soluble aggregates of neurodegeneration-causing proteins. Acta Neuropathol 139:503–526. https://doi.org/10.1007/s00401-019-02114-9
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I et al (2014) Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol 128:755–766. https://doi.org/10.1007/s00401-014-1349-0
Deane R, Wu Z, Sagare A, Davis J, Du Yan S, Hamm K et al (2004) LRP/amyloid β-peptide interaction mediates differential brain efflux of Aβ isoforms. Neuron 43:333–344. https://doi.org/10.1016/j.neuron.2004.07.017
DeVos SL, Corjuc BT, Oakley DH, Nobuhara CK, Bannon RN, Chase A et al (2018) Synaptic tau seeding precedes tau pathology in human Alzheimer’s disease brain. Front Neurosci 12:267. https://doi.org/10.3389/fnins.2018.00267
Dickson DW, Kouri N, Murray ME, Josephs KA (2011) Neuropathology of frontotemporal lobar degeneration-Tau (FTLD-Tau). J Mol Neurosci 45:384–389. https://doi.org/10.1007/s12031-011-9589-0
Duyckaerts C, Braak H, Brion JP, Buée L, Del Tredici K, Goedert M et al (2015) PART is part of Alzheimer disease. Acta Neuropathol 129:749–756. https://doi.org/10.1007/s00401-015-1390-7
Fitzpatrick AWP, Falcon B, He S, Murzin AG, Murshudov G, Garringer HJ et al (2017) Cryo-EM structures of tau filaments from Alzheimer’s disease. Nature 547:185–190. https://doi.org/10.1038/nature23002
Glennon EB, Lau DHW, Gabriele RMC, Taylor MF, Troakes C, Opie-Martin S et al (2020) Bridging integrator 1 protein loss in Alzheimer’s disease promotes synaptic tau accumulation and disrupts tau release. Brain Commun. https://doi.org/10.1093/braincomms/fcaa011
Gomes LA, Hipp SA, Rijal Upadhaya A, Balakrishnan K, Ospitalieri S, Koper MJ et al (2019) Aβ-induced acceleration of Alzheimer-related τ-pathology spreading and its association with prion protein. Acta Neuropathol 138:913–941. https://doi.org/10.1007/s00401-019-02053-5
Götz J, Chen F, Van Dorpe J, Nitsch RM (2001) Formation of neurofibrillary tangles in P301L tau transgenic mice induced by Aβ42 fibrils. Science 293:1491–1495. https://doi.org/10.1126/science.1062097
Grundke-Iqbal I, Iqbal K, Quinlan M, Tung YC, Zaidi MS, Wisniewski HM (1986) Microtubule-associated protein tau. A component of Alzheimer paired helical filaments. J Biol Chem 261:6084–6089
Guo JL, Narasimhan S, Changolkar L, He Z, Stieber A, Zhang B et al (2016) Unique pathological tau conformers from Alzheimer’s brains transmit tau pathology in nontransgenic mice. J Exp Med 213:2635–2654. https://doi.org/10.1084/jem.20160833
Guo T, Noble W, Hanger DP (2017) Roles of tau protein in health and disease. Acta Neuropathol 133:665–704. https://doi.org/10.1007/s00401-017-1707-9
Haass C, Schlossmacher MG, Hung AY, Vigo-Pelfrey C, Mellon A, Ostaszewski BL et al (1992) Amyloid β-peptide is produced by cultured cells during normal metabolism. Nature 359:322–325. https://doi.org/10.1038/359322a0
Harris JA, Koyama A, Maeda S, Ho K, Devidze N, Dubal DB et al (2012) Human P301L-mutant tau expression in mouse entorhinal-hippocampal network causes tau aggregation and presynaptic pathology but no cognitive deficits. PLoS ONE 7:e45881. https://doi.org/10.1371/journal.pone.0045881
Härtig W, Oklejewicz M, Strijkstra AM, Boerema AS, Stieler J, Arendt T (2005) Phosphorylation of the tau protein sequence 199–205 in the hippocampal CA3 region of Syrian hamsters in adulthood and during aging. Brain Res 1056:100–104. https://doi.org/10.1016/j.brainres.2005.07.017
He Z, Guo JL, McBride JD, Narasimhan S, Kim H, Changolkar L et al (2018) Amyloid-β plaques enhance Alzheimer’s brain tau-seeded pathologies by facilitating neuritic plaque tau aggregation. Nat Med 24:29–38. https://doi.org/10.1038/nm.4443
Hyman BT, Augustinack JC, Ingelsson M (2005) Transcriptional and conformational changes of the tau molecule in Alzheimer’s disease. Biochim Biophys Acta Mol Basis Dis 1739:150–157
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC et al (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimer’s Dement 8:1–13. https://doi.org/10.1016/j.jalz.2011.10.007
Jeganathan S, Hascher A, Chinnathambi S, Biernat J, Mandelkow EM, Mandelkow E (2008) Proline-directed pseudo-phosphorylation at AT8 and PHF1 epitopes induces a compaction of the paperclip folding of tau and generates a pathological (MC-1) conformation. J Biol Chem 283:32066–32076. https://doi.org/10.1074/jbc.M805300200
Jellinger KA (2018) Different patterns of hippocampal tau pathology in Alzheimer’s disease and PART. Acta Neuropathol 136:811–813
Koss DJ, Jones G, Cranston A, Gardner H, Kanaan NM, Platt B (2016) Soluble pre-fibrillar tau and β-amyloid species emerge in early human Alzheimer’s disease and track disease progression and cognitive decline. Acta Neuropathol 132:875–895. https://doi.org/10.1007/s00401-016-1632-3
Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C et al (2013) Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet 45:1452–1458. https://doi.org/10.1038/ng.2802
Lasorsa A, Malki I, Cantrelle F-X, Merzougui H, Boll E, Lambert J-C et al (2018) Structural basis of tau interaction with BIN1 and regulation by tau phosphorylation. Front Mol Neurosci 11:421. https://doi.org/10.3389/fnmol.2018.00421
Leroy K, Bretteville A, Schindowski K, Gilissen E, Authelet M, De Decker R et al (2007) Early axonopathy preceding neurofibrillary tangles in mutant tau transgenic mice. Am J Pathol 171:976–992. https://doi.org/10.2353/ajpath.2007.070345
Lewis J, Dickson DW, Lin WL, Chisholm L, Corral A, Jones G et al (2001) Enhanced neurofibrillary degeneration in transgenic mice expressing mutant tau and APP. Science 293:1487–1491. https://doi.org/10.1126/science.1058189
Li X, Kumar Y, Zempel H, Mandelkow EM, Biernat J, Mandelkow E (2011) Novel diffusion barrier for axonal retention of Tau in neurons and its failure in neurodegeneration. EMBO J 30:4825–4837. https://doi.org/10.1038/emboj.2011.376
Luna-Muñoz J, Chávez-Macías L, García-Sierra F, Mena R (2007) Earliest stages of tau conformational changes are related to the appearance of a sequence of specific phospho-dependent tau epitopes in Alzheimer’s disease. J Alzheimer’s Dis 12:365–375. https://doi.org/10.3233/JAD-2007-12410
Luna-Muñoz J, García-Sierra F, Falcón V, Menéndez I, Chávez-Macías L, Mena R (2005) Regional conformational change involving phosphorylation of tau protein at the Thr231, precedes the structural change detected by Alz-50 antibody in Alzheimer’s disease. J Alzheimer’s Dis 8:29–41. https://doi.org/10.3233/JAD-2005-8104
Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K (1985) Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci USA 82:4245–4249. https://doi.org/10.1073/pnas.82.12.4245
McInnes J, Wierda K, Snellinx A, Bounti L, Wang Y-C, Stancu I-C et al (2018) Synaptogyrin-3 mediates presynaptic dysfunction induced by tau. Neuron 97:823-835.e8. https://doi.org/10.1016/J.NEURON.2018.01.022
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement 7:263–269. https://doi.org/10.1016/j.jalz.2011.03.005
Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM et al (1991) The consortium to establish a registry for Alzheimer’s disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41:479–486. https://doi.org/10.1212/wnl.41.4.479
Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G et al (1989) The consortium to establish a registry for Alzheimer’s disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39:1159–1165. https://doi.org/10.1212/wnl.39.9.1159
Oh KJ, Perez SE, Lagalwar S, Vana L, Binder L, Mufson EJ (2010) Staging of Alzheimer’s pathology in triple transgenic mice: a light and electron microscopic analysis. Int J Alzheimers Dis. https://doi.org/10.4061/2010/780102
Neddens J, Temmel M, Flunkert S, Kerschbaumer B, Hoeller C, Loeffler T et al (2018) Phosphorylation of different tau sites during progression of Alzheimer’s disease. Acta Neuropathol Commun 6:52. https://doi.org/10.1186/s40478-018-0557-6
Nelson PT, Dickson DW, Trojanowski JQ, Jack CR, Boyle PA, Arfanakis K et al (2019) Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain 142:1503–1527. https://doi.org/10.1093/brain/awz099
Pickett EK, Herrmann AG, McQueen J, Abt K, Dando O, Tulloch J et al (2019) Amyloid beta and tau cooperate to cause reversible behavioral and transcriptional deficits in a model of Alzheimer’s disease. Cell Rep 29:3592-3604.e5. https://doi.org/10.1016/j.celrep.2019.11.044
Probst A, Tolnay M, Langui D, Goedert M, Spillantini MG (1996) Pick’s disease: hyperphosphorylated tau protein segregates to the somatoaxonal compartment. Acta Neuropathol 92:588–596. https://doi.org/10.1007/s004010050565
Reed LA, Schmidt ML, Wszolek ZK, Balin BJ, Soontornniyomkij V, Lee VMY et al (1998) The neuropathology of a chromosome 17-linked autosomal dominant parkinsonism and dementia (‘pallido-ponto-nigral degeneration’). J Neuropathol Exp Neurol 57:588–601. https://doi.org/10.1097/00005072-199806000-00006
Rijal Upadhaya A, Capetillo-Zarate E, Kosterin I, Abramowski D, Kumar S, Yamaguchi H et al (2012) Dispersible amyloid β-protein oligomers, protofibrils, and fibrils represent diffusible but not soluble aggregates: their role in neurodegeneration in amyloid precursor protein (APP) transgenic mice. Neurobiol Aging 33:2641–2660. https://doi.org/10.1016/J.NEUROBIOLAGING.2011.12.032
Rijal Upadhaya A, Kosterin I, Kumar S, Von Arnim CAF, Yamaguchi H, Fändrich M et al (2014) Biochemical stages of amyloid-β peptide aggregation and accumulation in the human brain and their association with symptomatic and pathologically preclinical Alzheimer’s disease. Brain 137:887–903. https://doi.org/10.1093/brain/awt362
Roberts BR, Lind M, Wagen AZ, Rembach A, Frugier T, Li QX et al (2017) Biochemically-defined pools of amyloid-β in sporadic Alzheimer’s disease: correlation with amyloid PET. Brain 140:1486–1498. https://doi.org/10.1093/brain/awx057
Sartori M, Mendes T, Desai S, Lasorsa A, Herledan A, Malmanche N et al (2019) BIN1 recovers tauopathy-induced long-term memory deficits in mice and interacts with Tau through Thr348 phosphorylation. Acta Neuropathol. https://doi.org/10.1007/s00401-019-02017-9
Scholz T, Mandelkow E (2014) Transport and diffusion of Tau protein in neurons. Cell Mol Life Sci 71:3139–3150
Sottejeau Y, Bretteville A, Cantrelle FX, Malmanche N, Demiaute F, Mendes T et al (2015) Tau phosphorylation regulates the interaction between BIN1’s SH3 domain and Tau’s proline-rich domain. Acta Neuropathol Commun 3:58. https://doi.org/10.1186/s40478-015-0237-8
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM et al (2011) Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement 7:280–292. https://doi.org/10.1016/j.jalz.2011.03.003
Spires-Jones TL, Attems J, Thal DR (2017) Interactions of pathological proteins in neurodegenerative diseases. Acta Neuropathol 134:187–205. https://doi.org/10.1007/s00401-017-1709-7
Takahashi M, Weidenheim KM, Dickson DW, Ksiezak-Reding H (2002) Morphological and biochemical correlations of abnormal tau filaments in progressive supranuclear palsy. J Neuropathol Exp Neurol 61:33–45. https://doi.org/10.1093/jnen/61.1.33
Thal DR, Capetillo-Zarate E, Del Tredici K, Braak H (2006) The development of amyloid beta protein deposits in the aged brain. Sci Aging Knowl Environ 2006:re1
Thal DR, Rüb U, Orantes M, Braak H (2002) Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology 58:1791–1800. https://doi.org/10.1212/WNL.58.12.1791
Thal DR, Rüb U, Schultz C, Sassin I, Ghebremedhin E, Del Tredici K et al (2000) Sequence of Aβ-protein deposition in the human medial temporal lobe. J Neuropathol Exp Neurol 59:733–748. https://doi.org/10.1093/jnen/59.8.733
Thal DR, Del Tredici K, Braak H (2004) Neurodegeneration in normal brain aging and disease. Sci Aging Knowl Environ 2004:PE26
Trinczek B, Ebneth A, Mandelkow EM, Mandelkow E (1999) Tau regulates the attachment/detachment but not the speed of motors in microtubule-dependent transport of single vesicles and organelles. J Cell Sci 112:2355–2367
Wang Y, Mandelkow E (2016) Tau in physiology and pathology. Nat Rev Neurosci 17:5–21. https://doi.org/10.1038/nrn.2015.1
Weaver CL, Espinoza M, Kress Y, Davies P (2000) Conformational change as one of the earliest alterations of tau in Alzheimer’s disease. Neurobiol Aging 21:719–727. https://doi.org/10.1016/S0197-4580(00)00157-3
Welikovitch LA, Do Carmo S, Maglóczky Z, Szocsics P, Lőke J, Freund T et al (2018) Evidence of intraneuronal Aβ accumulation preceding tau pathology in the entorhinal cortex. Acta Neuropathol 136:901–917. https://doi.org/10.1007/s00401-018-1922-z
Wittmann CW, Wszolek MF, Shulman JM, Salvaterra PM, Lewis J, Hutton M et al (2001) Tauopathy in Drosophila: neurodegeneration without neurofibrillary tangles. Science 293:711–714. https://doi.org/10.1126/science.1062382
Wu H-Y, Kuo P-C, Wang Y-T, Lin H-T, Roe AD, Wang BY et al (2018) β-Amyloid induces pathology-related patterns of tau hyperphosphorylation at synaptic terminals. J Neuropathol Exp Neurol 77:814–826. https://doi.org/10.1093/jnen/nly059
Zempel H, Dennissen FJA, Kumar Y, Luedtke J, Biernat J, Mandelkow EM et al (2017) Axodendritic sorting and pathological missorting of Tau are isoform-specific and determined by axon initial segment architecture. J Biol Chem 292:12192–12207. https://doi.org/10.1074/jbc.M117.784702
Zhou L, McInnes J, Wierda K, Holt M, Herrmann AG, Jackson RJ et al (2017) Tau association with synaptic vesicles causes presynaptic dysfunction. Nat Commun 8:15295. https://doi.org/10.1038/ncomms15295
Zhou XW, Li X, Bjorkdahl C, Sjogren MJ, Alafuzoff I, Soininen H et al (2006) Assessments of the accumulation severities of amyloid β-protein and hyperphosphorylated tau in the medial temporal cortex of control and Alzheimer’s brains. Neurobiol Dis 22:657–668. https://doi.org/10.1016/j.nbd.2006.01.006
Acknowledgements
We thank Dr. Peter Davies, Department of Pathology, Albert Einstein College of Medicine, USA, for the gift of the PHF1, TG3 and MC1 antibodies. We gratefully thank the J. David Gladstone Institutes (San Francisco, USA) for the gift of the acK274-tau antibody (MAB359). Support: Fonds Wetenschappelijk Onderzoek (FWO) G0F8516N (DRT, RV); Vlaamse Impulsfinanciering voor Netwerken voor Dementie-onderzoek (IWT 135043) (RV, DRT).
Author information
Authors and Affiliations
Contributions
Study design: LAG, DRT; immunohistochemistry: LAG, DLS, SOT; histological assessment: LAG, DLS, SOT; neuropathology: DRT, TT; clinical neurology: RV, MV, CAFvA; Drosophila experiments: VU, PV; statistical analysis: LAG, DRT, VU; data interpretation: LAG, DRT, VU, SOT; manuscript preparation: LAG, DRT, VU; critical manuscript review: DL, VU, SOT, TT, RV, MV, PV, CAFvA.
Corresponding authors
Ethics declarations
Conflict of interest
DLS is currently an employee of Novartis Oncology Spain. CAFvA received honoraria from serving on the scientific advisory board of Roche (2018–2019) and Dr. Willmar Schwabe GmbH & Co. KG (2019) and has received funding for travel and Speaker honoraria from Nutricia GmbH (2014–2015), Lilly Deutschland GmbH (2013–2016), Biogen (2016–2018), Roche (2017–2019) and Dr. Willmar Schwabe GmbH & Co. KG (2014–2015). RV was PI of the first-in-human trial with 18F-MK6240 (Merck) and global PI of the phase 1 and 2 trials of 18F-flutemetamol (GE). RV’s institution has consultancy agreements (RV as consultant) with Novartis and AC-Immune as well as clinical trial agreements (RV as PI) with AbbVie, Roche, Prevail and Alector. DRT received speaker honorary from Novartis Pharma AG (Switzerland), Biogen (USA), travel reimbursement from GE-Healthcare (UK) and UCB (Belgium) and collaborated with Novartis Pharma AG (Switzerland), Probiodrug (Germany), GE-Healthcare (UK), and Janssen Pharmaceutical Companies (Belgium).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aragão Gomes, L., Uytterhoeven, V., Lopez-Sanmartin, D. et al. Maturation of neuronal AD-tau pathology involves site-specific phosphorylation of cytoplasmic and synaptic tau preceding conformational change and fibril formation. Acta Neuropathol 141, 173–192 (2021). https://doi.org/10.1007/s00401-020-02251-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-020-02251-6