Abstract
Introduction
Inflammatory pseudotumor (IPT) in the sinonasal cavity and skull base region is benign non-neoplastic inflammatory process. However, IPT can mimic malignant tumor or infectious disease and there are difficulties in confirmation of diagnosis. The aim of study is to evaluate the clinical significance of immunoglobulin G4 (IgG4) in IPT in terms of steroid response and differential diagnosis with other skull base infiltrative lesions.
Methods
Medical records were reviewed retrospectively from 1998 to 2016. Subjects diagnosed with IPT by surgical biopsy were enrolled. IgG4 positivity was defined as IgG4/IgG ratio > 0.4. Additionally, IgG4/IgG ratio was calculated in eight skull base osteomyelitis (SBO) patients.
Results
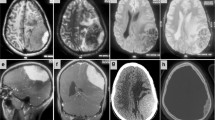
Twenty-six IPT patients were included and the average age was 52.3 years, and 57.7% were male and 42.3% were female. Most lesions were involved in the sinuses (88.5%) and the incidence of extension beyond the sinuses itself was as follows: the cheek/hard palate/parapharynx (15.4%), orbit (61.5%), skull base (57.7%), and dura or brain (23.1%). All IPT cases revealed IgG4 + plasma cells and IgG4/IgG ratio over 0.4 was detected in 42.3% (11/26) of cases. In case of SBO, no patients had IgG4/IgG ratio exceed 0.4. Main treatment modality was systemic steroids (61.5%) and other modalities were used: surgery (3.8%), immunosuppressant (7.7%), radiotherapy (30.8%), or a combination of these modalities (15.4%). Steroid responses were not significantly different, but IgG4-positive group tended to have better response to steroid therapy.
Conclusions
IgG4-positive and IgG4-negative IPT patients revealed no differences in involvement sites, clinical course, and steroid responses. However, IgG4/IgG ratio and IgG4 + plasma cell count can provide a diagnostic clue for infiltrative skull base lesions such as IPT and a differential diagnosis of SBO.




Similar content being viewed by others
References
Garg V, Temin N, Hildenbrand P, Silverman M, Catalano PJ (2010) Inflammatory pseudotumor of the skull base. Otolaryngol Head Neck Surg 142:129–131
Ginat DT, Bokhari A, Bhatt S, Dogra V (2012) Inflammatory pseudotumors of the head and neck in pathology-proven cases. J Neuroradiol 39:110–115
Alyono JC, Shi Y, Berry GJ, Recht LD, Harsh GRt, Jackler RK, Corrales CE (2015) Inflammatory pseudotumors of the skull base: meta-analysis. Otol Neurotol 36:1432–1438
Narla LD, Newman B, Spottswood SS, Narla S, Kolli R (2003) Inflammatory pseudotumor. Radiographics 23:719–729
Desai SV, Spinazzi EF, Fang CH, Huang G, Tomovic S, Liu JK, Baredes S, Eloy JA (2015) Sinonasal and ventral skull base inflammatory pseudotumor: a systematic review. Laryngoscope 125:813–821
Han MH, Chi JG, Kim MS, Chang KH, Kim KH, Yeon KM, Han MC (1996) Fibrosing inflammatory pseudotumors involving the skull base: MR and CT manifestations with histopathologic comparison. AJNR Am J Neuroradiol 17:515–521
Park SB, Lee JH, Weon YC (2009) Imaging findings of head and neck inflammatory pseudotumor. AJR Am J Roentgenol 193:1180–1186
Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, Kloppel G, Heathcote JG, Khosroshahi A, Ferry JA, Aalberse RC, Bloch DB, Brugge WR, Bateman AC, Carruthers MN, Chari ST, Cheuk W, Cornell LD, Fernandez-Del Castillo C, Forcione DG, Hamilos DL, Kamisawa T, Kasashima S, Kawa S, Kawano M, Lauwers GY, Masaki Y, Nakanuma Y, Notohara K, Okazaki K, Ryu JK, Saeki T, Sahani DV, Smyrk TC, Stone JR, Takahira M, Webster GJ, Yamamoto M, Zamboni G, Umehara H, Stone JH (2012) Consensus statement on the pathology of IgG4-related disease. Mod Pathol 25:1181–1192
Stone JH, Zen Y, Deshpande V (2012) IgG4-related disease. N Engl J Med 366:539–551
Chougule A, Bal A (2016) IgG4-related inflammatory pseudotumor: a systematic review of histopathological features of reported cases. Mod Rheumatol 27(2):320–325
Carruthers MN, Stone JH, Deshpande V, Khosroshahi A (2012) Development of an IgG4-RD responder index. Int J Rheumatol 2012:259408
Gao Y, Zheng M, Cui L, Chen N, Wang YN, Zhan YT, Wang ZG (2018) IgG4-related disease: association between chronic rhino-sinusitis and systemic symptoms. Eur Arch Otorhinolaryngol 275:2013–2019
Betancur-Vasquez L, Gonzalez-Hurtado D, Arango-Isaza D, Rojas-Villarraga A, Hernandez-Parra D, Carmona S, Diaz-Coronado JC (2019) IgG4-related disease: is rituximab the best therapeutic strategy for cases refractory to conventional therapy? Results of a systematic review. Reumatol Clin. https://doi.org/10.1016/j.reuma.2018.11.011
Fernandez-Codina A, Pinilla B, Pinal-Fernandez I, Lopez C, Fraile-Rodriguez G, Fonseca-Aizpuru E, Carballo I, Brito-Zeron P, Feijoo-Masso C, Lopez-Dupla M, Cid MC, Martinez-Valle F (2018) Treatment and outcomes in patients with IgG4-related disease using the IgG4 responder index. Jt Bone Spine 85:721–726
Dehner LP (2000) The enigmatic inflammatory pseudotumours: the current state of our understanding, or misunderstanding. J Pathol 192:277–279
Cain RB, Colby TV, Balan V, Patel NP, Lal D (2014) Perplexing lesions of the sinonasal cavity and skull base: IgG4-related and similar inflammatory diseases. Otolaryngol Head Neck Surg 151:496–502
Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S, Hamano H, Kamisawa T, Shimosegawa T, Shimatsu A, Nakamura S, Ito T, Notohara K, Sumida T, Tanaka Y, Mimori T, Chiba T, Mishima M, Hibi T, Tsubouchi H, Inui K, Ohara H (2012) Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol 22:21–30
Lee DK, Cho YS, Hong SH, Chung WH, Ahn YC (2006) Inflammatory pseudotumor involving the skull base: response to steroid and radiation therapy. Otolaryngol Head Neck Surg 135:144–148
Heeringa JJ, Karim AF, van Laar JAM, Verdijk RM, Paridaens D, van Hagen PM, van Zelm MC (2018) Expansion of blood IgG4(+) B, TH2, and regulatory T cells in patients with IgG4-related disease. J Allergy Clin Immunol 141:1831.e1810–1843.e1810
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (2017R1A2B4006453). In addition, this work was supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Ethical approval
Obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ryu, G., Cho, HJ., Lee, K.E. et al. Clinical significance of IgG4 in sinonasal and skull base inflammatory pseudotumor. Eur Arch Otorhinolaryngol 276, 2465–2473 (2019). https://doi.org/10.1007/s00405-019-05505-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05505-6