Abstract
Cervical dystonia is a neurological movement disorder causing abnormal posture of the head. It may be accompanied by involuntary movements which are sometimes tremulous. The condition has marked effects on patients’ self-image, and adversely affects quality of life, social relationships and employment. Botulinum neurotoxin (BoNT) is the treatment of choice for CD and its efficacy and safety have been extensively studied in clinical trials. However, current guidelines do not provide enough practical information for physicians who wish to use this valuable treatment in a real-life setting. In addition, patients and physicians may have different perceptions of what successful treatment outcomes should be. Consequently, an international group of expert neurologists, experienced in BoNT treatment, met to review the literature and pool their extensive clinical experience to give practical guidance about treatment of CD with BoNT. Eight topic headings were considered: the place of BoNT within CD treatment options; patient perspectives and desires for treatment; assessment and goal setting; starting treatment with BoNT-A; follow-up sessions; management of side effects; management of non-response; switching between different BoNT products. One rapporteur took responsibility for summarising the current literature for each topic, while the consensus statements were developed by the entire expert group. These statements are presented here along with a discussion of the background information.
Similar content being viewed by others
Introduction
Cervical dystonia (CD) is a movement disorder characterised by inappropriate contractions of the cervical musculature related to a dysfunction of sensorimotor neural circuits. It causes involuntary movements of the neck and head, which may be accompanied by tremor, and results in abnormal postures. In addition to the impaired neck mobility and abnormal posturing, chronic or frequently occurring neck pain is a recognised clinical feature of CD that occurs more frequently than in other forms of dystonia [1]. This constellation of symptoms, and a reduction in the patient’s self-image, may result in disability and adversely impact the individual’s quality of life [2, 3].
Botulinum neurotoxin (BoNT) treatment is the accepted standard of care for patients with CD and the preferred toxin type is BoNT-A. There are a number of published guidelines which deal with the general aspects, but do not cover the many practical variables that influence outcome of BoNT treatment for CD [4–6]. The success of treatment is very dependent on the experience and ability of the injector, both to identify and to treat the involved muscles, yet there is little practical guidance available to help the treating physician achieve optimal results. Additionally, as experienced injectors, we have observed that patients have different individual needs and expectations of treatment. There may also be different perceptions between the patient and the treating physician on what should be the goals of treatment and what is deemed a satisfactory outcome. Therefore, an international group of neurologists, experts in this area, were brought together to produce consensus statements about the key practical issues that can contribute to achieving the highest degree of patient satisfaction with BoNT-A treatment in CD.
Methods
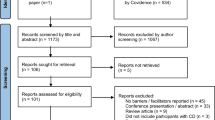
An International Consensus Committee, consisting of 15 neurologists with extensive experience in the treatment of CD with BoNT, was established to review the literature and provide a consensus. The preparatory work of the group consisted of a search and review of pertinent publications on the evaluation and treatment of cervical dystonia, with particular regard to patient perspectives and treatment with BoNT-A. Computerised MEDLINE searches including publications from 2007 to 2013 were conducted using a combination of text words and MeSH terms: [“torticollis”(MESH terms) OR “torticollis”(all fields) OR “cervical”(all fields) AND “dystonia”(all fields) OR “cervical dystonia”(all fields)] and limited to human studies. The reference lists of all known primary articles were searched for additional, relevant citations, which were also included even if they were published before 2007. No language restrictions were applied.
The topic was divided into eight sections that were chosen to address the practicalities of real-life treatment of CD: (1) place of BoNT within CD treatment options, (2) patient perspectives and desire for treatment, (3) assessment and goal setting, (4) starting treatment with BoNT-A, (5) follow-up sessions, (6) management of side effects, (7) management of non-response and (8) switching between different BoNT products. The search results were then reviewed to locate the papers relevant to each section.
Eight rapporteurs took responsibility for one section each and developed a presentation to be discussed within the entire group during a 1-day meeting, from which the consensus statements were developed. The group utilised the consensus development conference methodology to provide consensus statements on the use of BoNT-A in CD [7].
Although several formulations of BoNT are available, this consensus focuses on the most widely investigated and widely used preparations of botulinum toxin A: onabotulinumtoxinA (BoNT-A/Ona, Botox® Allergan); abobotulinumtoxinA (BoNT-A/Abo, Dysport® Ipsen) and incobotulinumtoxinA (BoNT-A/Inco, Xeomin® Merz). RimabotulinumtoxinB (BoNT-B/Rima, Myobloc® USWorldMeds, Neurobloc®, Eisai) was also mentioned.
Results
Consensus statements, key literature and commentary
The consensus statements are summarised in Table 1.
Place of BoNT within CD treatment options—Rapporteur Maja Relja
Initially, cervical dystonia was treated with oral medications, or surgical interventions, but their effects were disappointing in most cases [8, 9]. Consequently, chemodenervation using BoNT-A has become the cornerstone of treatment for CD with a good safety and efficacy profile. However, surgical treatment, particularly pallidal neurostimulation, may still be considered for patients with severe CD refractory to the combination of oral drugs and chemodenervation [10, 11]. Adjuvant physiotherapy might be proposed regardless of the therapeutic option.
Oral treatment (including anticholinergic agents, γ-aminobutyric acid (GABA) mimetic agents, dopamine receptor antagonists, dopamine-depleting agents and even dopamine receptor agonists) is limited in efficacy and there is a lack of sound scientific evidence supporting the use of most agents [4]. Systemic effects of oral therapy are non-selective, often causing generalised and problematic adverse events. The many different treatments tried over the years also testify to both their relative ineffectiveness and the recalcitrant nature of cervical dystonia. Once the efficacy of BoNT had been demonstrated in the 1980s, it rapidly assumed a place as the treatment of choice for this condition, warranting both European Federation of Neurological Societies EFNS and the American Association of Neurology (AAN) level A recommendations as first-line treatment [5, 6, 12, 13].
A recent systematic review of the current literature has supported this position, showing that BoNT is the most effective treatment for reducing dystonic symptoms and pain in patients with focal dystonia [14].
BoNT treatment has a peak effect few weeks after treatment and tends to decay variably over time. Given the chronic nature and the varying features of dystonia over time, changes in dosage and targeting may be required over repeated treatment sessions. The amplitude of the response to BoNT-A has been investigated in terms of reduction of the maximal voluntary EMG amplitude in the sternocleidomastoid muscle in a group of 34 patients with cervical dystonia undergoing regular BoNT-A therapy with BoNT-A/Ona (n = 16) or BoNT-A/Abo [15]. Dose-dependent EMG amplitude reductions were seen with both toxin preparations: with BoNT-A/Ona this ranged from 80 to 91 % in response to 20–80 units; with BoNT-A/Abo the responses ranged from 80 to 91 % with doses of 100–500 units.
The efficacy of BoNT-A has been shown to be sustained over at least 12 years (mean 15.8 ± 1.5 years) of continuous use [16] in a longitudinal follow-up study. Two reviews have also addressed the long-term efficacy and safety of botulinum toxin [17, 18]. These authors concluded that the majority of patients comply with long-term treatment because they experience positive and stable effects over time, and there is no evidence of specific adverse events through the long-term use of botulinum toxins.
Patient perspectives and expectations from treatment—–Rapporteur Inger Marie Skogseid
Alongside the clearly visible dystonic symptoms of abnormal movements or postures, patients with CD often experience functional disability, pain and other sensory disturbances including impaired proprioception [19–23] and sometimes depression and/or anxiety. Increasingly, these symptoms are being termed non-motor [24], although the term is not universally accepted, because in many patients these effects are probably, at least in part, secondary to the motor symptoms. These symptoms can cause reduced ability to work [19, 21, 25, 26], impaired social functioning and social stigma [26, 27] and sometimes impair activities of daily living, including those of personal hygiene. These factors (especially pain), which impact on employment and psychosocial functioning, are the most common reasons for patients seeking treatment.
The marked negative impact of CD on patients’ quality of life [2] can be ameliorated by effective BoNT treatment [27–29]. The majority of studies used established QoL instruments, the most popular of which was the Short Form-36 Health Survey (SF-36) [2, 27, 28, 30]. All of these showed decreased HRQoL in patients with CD compared with healthy volunteers (either control groups in the study or by comparison with the general population).
BoNT-A treatment improved several domains of the SF-36. Interestingly, the improvement seen on patient-related QoL parameters was not always correlated with physician assessments of the effect of BoNT-A using measures such as the TWSTRS score. Using a combination of patient-reported and physician-reported scores, Skogseid et al. [27] showed that the majority of the CD population undergoing long-term treatment with BoNT-A achieved a good HRQoL. Those with poorer HRQoL scores tended to be those with higher TWSTRS scores and greater degrees of depression.
Effective treatment can also improve their employment status and decrease depression among CD patients, which is one of the most important predictive factors for poor quality of life [21, 27, 28, 30].
At the outset of treatment it is essential to discuss with the patients what they can expect from the treatment and to ensure that there is sufficient understanding between patients and physicians about the treatment goals they have and which are achievable and realistic. Indeed, studies have shown that patients’ perceptions and neurologists’ perceptions of treatment satisfaction are not always aligned [20, 31].
Assessment and goal setting—Rapporteur Charalampos Tzoulis
Assessment of patients with CD is aimed at identifying the clinical features and aetiology based on the current classification [32] and rating motor and non-motor clinical features as a basis for follow-up.
The cornerstone of diagnosis is the clinical examination of abnormal involuntary movements and postures [26, 33]. Currently, there is no consensus on diagnostic criteria for CD and misdiagnosis is not a rare occurrence [34]. A recent consensus update considered two axes for classification: it provided a snapshot of the patient’s clinical features that can be repeated in time for comparison, on Axis I, and an aetiological classification that is reassessed when needed, on Axis II [32].
Patient assessment prior to injection should consider the clinical aspects that may influence the selection of muscles for injection. Patients may use compensatory movements to overcome forceful dystonic posturing, such as neck flexion, or trunk anteroflexion to overcome a retrocollis, and such movements must be distinguished from primary CD components [35]. Another aspect is muscle weakness or atrophy that may be secondary to previous BoNT treatment. Muscles involved in compensatory movements and weak muscles are usually not injected with BoNT. Pain may be caused by muscle contraction, in which case it provides a useful orientation for muscle targeting, or by overstretching of opponent muscles. Chronic pain may be sustained by local release of pain mediators or musculotendinous inflammation.
Dystonic tremor may respond less well than dystonic postures to BoNT treatment. Usually, postural abnormalities and pain are first-line criteria for muscle choice.
Rating of CD is commonly performed using dedicated scales. Scoring at baseline, at the time of peak effect (approximately, 1 month after injection) and before retreatment, allows injectors to assess outcome and plan changes in dosing and targeting, if necessary. The most commonly used dystonia scales have been the object of a recent revision by a Movement Disorders Society task force [36]. The Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS), the Cervical Dystonia Impact Scale (CDIP-58) and the Cervical Dystonia Questionnaire (CDQ-24) are “recommended” for cervical dystonia; the Functional Disability Questionnaire, the Tsui Scale and the Body Concept Scale have been rated as “suggested”. Of these, a physician-rated severity score is found in the TWSTRS and the Tsui scores. Recently, the Dystonia Discomfort Scale (DDS) has been introduced as a novel instrument to monitor the temporal profile of BoNT therapy in CD patients who can perform a self-assessment at home [37]. Furthermore, a new version of the TWSTRS is currently being validated in North America and Europe.
Starting treatment with BoNT-A—Rapporteur Elena Moro
The main goal of treating CD with BoNT is to correct both dystonic movements and abnormal postures and thus be able to reduce pain, discomfort, and functional disability and improve patient’s quality of life.
When a CD patient undergoes the initial BoNT treatment, the first step is muscle selection. This is a crucial step and relies on accurate clinical examination of the patient.
Dystonic malposture may affect only the cervical spine itself (-collis, 20 % of cases) or only the head´s position in relation to the cervical spine (-caput, 19 % of cases) or a combination of both (61 % of cases). A detailed classification of the different abnormal postures in CD patients has been recently proposed by Reichel [38]. By understanding this classification, injection of BoNT into muscles that are not involved can be avoided. As well as the anatomical location, it is important to understand the function of the involved muscles. The dystonic posture should be analysed in a 3D space and using activation and deactivation tasks.
Dystonic muscle activity may be mainly tonic, myoclonic, tremulous or a complex mixture. In simple cases, an accurate clinical examination will usually allow identification of the primary involved muscles and enable them to be separated from muscles with compensatory activity. Faster dystonic movements also need to be assessed, since their response to BoNT is not so predictable. Although clinical examination allows the evaluation of all motor components of CD, for more complex or unclear cases electromyography (EMG) mapping can be very useful for a more accurate selection of the most relevant and active dystonic muscles.
A recent study has further detailed the clinical phenotypes of dystonic posterior sagittal shift or “double chin” posture and anterior sagittal shift or “goose neck” posture. They used clinical examination and EMG to define more clearly the involved muscles and proposed specific BoNT treatment protocols for these forms of CD [39]. A new technique of injection of the longus colli, based on a laterocervical approach under EMG guidance, has also been described.
Injections may be carried out using visual inspection and palpation of muscles for the more superficial muscles; EMG or ultrasound is recommended for accurately locating deeper muscles [40, 41]. A summary of how to conduct muscle identification is given in Table 2.
The second step consists of choosing which BoNT formulation to use. All marketed BoNT brands are licensed for cervical dystonia [42–45] and can be used for treatment.
The third step concerns the use of the appropriate BoNT dose and dilution. Doses must be tailored to the individual patient, based on type of muscle, the degree of muscle activity, muscle size, and sometimes location of pain. There are different minimal starting doses suggested for each muscle. Dose recommendations by muscle are given in Table 3 (modified from [46] ).The concentration of toxin, number of units and number of injections/muscle should be recorded for each muscle.
Patients should be informed about possible side effects and action profile of BoNT. They should be told that results may not be immediate after the first injection and that it normally takes up to about a week before the clinical effects of BoNT-A start to appear and then several days (or even 1–2 weeks) to reach its maximal effect. Importantly, patients should also know that titration of doses to reduce muscle activity over two to three treatment sessions may be necessary to achieve a significant symptom reduction and functional benefit.
It has been proposed that physical therapy can potentiate the effect of BoNT [9]. However, a systematic literature search has concluded that cautious interpretation on the effectiveness of physiotherapy as an adjuvant therapy is warranted, and that additional high-quality clinical trials are needed before firm conclusions can be drawn [47].
Follow-up sessions—Rapporteur Alberto Albanese
The majority of patients with CD require long-term treatment, involving regular, repeated injections. Patients should be assessed for their response to the initial treatment and subsequent injections based on: (a) clinical evidence of magnitude of response; (b) consideration of whether other muscles should be included; (c) patient perception of efficacy and duration of response; (d) severity and duration of side effects.
The current manufacturers’ literature suggests that the minimum period before repeating the treatment should be 10–12 weeks (Botox® SmPC; Dysport® SmPC; Xeomin® SmPC) [42–44]. However, the original recommendation (which most subsequent trials followed) was based on very few patients (n = 28) and outcomes, and was using the original formulation of BoNT-A marketed by Allergan which carried a higher risk of developing immunoresistance due to its higher protein load [48].
Increasingly, patients and physicians find that an injection schedule with fixed intervals of 12 weeks may not be appropriate for all patients. Thus, the variability in duration of response to BoNT was studied in 404 patients across 38 centres [49]. Only 49.3 % of patients rated duration of response ≥ 12 weeks for all BoNT-A preparations. A further study assessed treatment duration (TD) (time between injection and patient-reported waning of effect) in 59 patients and showed that the mean TD/patient was 7.8 ± 1.4 to 21.0 ± 3.9 weeks [50]. A patient satisfaction survey conducted in patients treated with BoNT-A/Ona or BoNT-A/Abo has also shown that patient satisfaction with treatment declines prior to re-injection, and many (46 %) patients would prefer an injection schedule of less than 12 weeks [31].
Subsequently Evidente et al. [51] conducted a double-blind, randomised controlled trial of BoNT-A/Inco versus placebo in pre-treated or treatment-naive CD patients. A flexible dosing schedule was evaluated over a 68 week extension to the initial study of pre-treated or treatment-naive patients [52]. In those who received ≥ 2 injections, the median intervals were: 6 to ≤ 10 weeks in 22.5 %; > 10 to ≤ 12 weeks in 24.6 %; > 12 to ≥ 14 weeks in 19.4 % and > 14 weeks in 33.5 %.
This suggests that it might be useful to adopt a flexible dosing schedule. Flexible schedules may require some service adjustment to accommodate, but not necessarily an increase in the number of injections delivered overall, since the mean injection interval seen for these ‘flexible’ patients was still 12 weeks.
Dosing and targeting are usually varied during the first two to three treatment sessions and tend to stabilise afterwards, although adjustments also may be necessary at later sessions. Typically, the doses used in the first session are increased in some or all injected muscles and new muscles are considered for injection based on the remaining symptoms. To make these decisions, it is useful to have a patient assessment around 1 month after the preceding session, when BoNT action has peaked, and to compare it with the observed pattern of dystonia at the time of injection.
When considering dosing intervals, it is worth noting that in the study by Evidente et al. [51] in which flexible dosing intervals were employed, there were no differences in the tolerability profile between groups of patients injected at 6 to <10 weeks, 10 to ≤12 weeks or 12 to ≤14 weeks or >14 weeks and there were no instances of antibody formation.
Management of adverse events—Rapporteur Fina Marti
The adverse events of BoNT-A treatment are usually mild and self-limiting and similar in both nature and severity between the different formulations. A meta-analysis of 36 randomised controlled studies reported adverse events in 25 % (353/1425) of the BoNT-A (BoNT-A/Ona)-treated patient versus 15 % (133/884) in controls [53].
The most common adverse events related to BoNT-A are: dysphagia; neck muscle weakness; injection site pain; and ‘flu-like’ symptoms [18]. Adverse events of BoNT-A are dose related and mostly due to contiguous or distant spread of toxin. Therefore, it is important that injections are located precisely so that potential spread of toxin is minimised. Spread or diffusion of toxin into neighbouring muscles may be influenced by the injection technique, the dose employed, the concentration and also the volume of injection. Targeting can be improved by EMG- or ultrasound-guided placement of injections [41]. However, there is no agreement whether single or multiple injections should be placed in each muscle.
The chemodenervation achieved by the toxin is also dose dependent [54, 55]. It has been reported that a fivefold increase in toxin injection volume, but keeping the same dose of toxin, resulted in a 50 % increase in the affected area [56].
Using a hind limb muscle animal model, no differences were observed between different formulations of toxin (BoNT-A/Ona, BoNT-A/Abo or BoNT-A/Inco) [57] and diffusion was not affected by the molecular size of the toxin preparation and the presence of complexing proteins [58, 59]. Since all formulations have similar diffusion profiles, no specific advantages can be proposed for any particular formulation for treating the largest or smallest muscles involved in dystonia.
Recommendations for minimising adverse events include always using the lowest effective dose. Dysphagia can be reduced by giving sternocleidomastoid injections into the upper third of the muscle, increasing the concentration of toxin and by reducing the dose per muscle when giving bilateral sternocleidomastoid and hyoid muscle injections. For bilateral injections to the splenius capitis and semispinalis capitis, the individual muscle dose should also be reduced and a lower dose is advisable for any muscle weakened by previous treatment [60].
There are no adequate data from the use of botulinum toxin type A in pregnant women [61]. Studies in animals have shown reproductive toxicity. The potential risk for humans is unknown. The SPC for Botox® does not recommend use during pregnancy and in women of child-bearing potential not using contraception [42]. Dysport® should be used during pregnancy only if the benefit justifies any potential risk to the fetus [43]; Xeomin® is contraindicated, unless the potential benefit justifies the risk [44].
Management of non-response—Rapporteur Giovanni Abbruzzese
Primary non-responders are those patients who do not get benefit from the first treatment. When this occurs the physician should first review the diagnosis and confirm that the patient’s condition is actually due to dystonia.
If the diagnosis of dystonia is robust and reliable, the most obvious cause of non-response is insufficient dosage or wrong muscle selection (this may make it difficult in some cases to distinguish between non-response and insufficient response). As mentioned previously, the lowest effective dose should be used at the outset of treatment to limit the risk of adverse events and may take two to three sessions before BoNT treatment reaches it maximal potential, during which time doses may need to be adjusted and refined. Current treatment recommendations for CD have reduced the frequency of non-response to 2 % over a treatment period of 2 years [62].
Secondary non-responders are those patients who fail to benefit at some point in time, having reported adequate benefit from previous treatment sessions. There is no universally accepted definition of secondary non-response to BoNT in CD.
An insufficient improvement in posture after ≥3 unsuccessful injection cycles has been proposed as a defining criterion [63, 64]. It was originally thought that secondary non-response was due in the majority of cases to the presence of neutralising antibodies. Antibody formation is more likely when the protein load is high. Direct comparisons in an animal model showed differences in the potential for development of neutralising antibodies. After repeated intradermal injections in New Zealand white rabbits (16 U/animal for 8 administrations every 2–8 weeks for BoNT-A/Ona and BoNT-A/Inco; 40U/kg for 5 administrations over 13 week BoNT-A/Abo), the results showed that 15 rabbits developed antibodies after six injections of BoNT-A/Abo, 4 developed antibodies after nine injections of BoNT-A/Ona and none developed antibodies after BoNT-A/Inco [59, 65]. Formulations with low antigenicity may offer advantages when using high doses or if a dosing schedule with short interval is preferred for a particular patient. Most physicians would use the frontalis test or the extensor digitorum brevis test for detecting the presence of neutralising antibodies [66].
Exact and quantitative measurement of BoNT antibodies, however, is only possible by the mouse lethality test or the mouse diaphragm assay. A novel ELISA test, recently introduced, offers low-cost animal-friendly and sensitive BoNT antibody testing [67].
Another important cause of secondary non-response is insufficient dosing or inappropriate muscle selection, which can occur particularly if a fixed treatment scheme is repeated—without review—in subsequent treatment sessions [4, 60].
When secondary (or primary) non-response to BoNT-A (and BoNT-B) treatment persists, despite careful re-evaluation of both diagnosis and treatment by experienced dystonia specialists and injectors, deep brain stimulation (DBS) is a treatment option that is now under scrutiny [10, 11, 68].
Switching between different BoNT products—Rapporteur Emmanuel Roze
While it is usually considered desirable to maintain treatment with a formulation of BoNT-A that produces results judged satisfactory by both patient and physician, sometimes product switches may be required. The main causes for product switching include: non-response, changes in tenders to hospitals which may result in restricted product availability, health insurance restrictions, physician preference/experience, patient preference, when the patient requires different injection intervals and other individual needs.
Before 2005, only two formulations of BoNT-A were available: BoNT-A/Ona and BoNT-A/Abo, so this was the only product switch within BoNT-A usage that was relevant. With the introduction of BoNT-A/Inco, the scope for product switching has increased.
Considering BoNT-A/Ona to BoNT-A/Abo switch, studies showed highly variable results: the potency of BoNT-A/Ona relative to BoNT-A/Abo has been estimated to be 1:2 up to 1:11 [69, 70]. A randomised controlled trial later suggested a ratio of 1:3, but the products are still not equivalent at this ratio [71] and recent studies suggest that 1:4 may be a more appropriate ratio [72, 73]. These highly variable data led the manufacturers to warn against using a simple formula to convert dosages, since there is no simple dose equivalence. Consequently, when switching between BoNT-A/Ona and BoNT-A/Abo, it is advisable to gradually reduce the dose of BoNT-A/Ona, switch to BoNT-A/Abo and then to titrate the dose upwards, observing the patient’s response.
Where product switches have been achieved successfully, comparable efficacy can be achieved, although the doses are different. Odergren et al. [74] showed no statistical difference in Tsui scores comparing BoNT-A/Ona and BoNT-A/Abo (ratio 1:3), while clinical efficacy was better with BoNT-A/Ona compared with BoNT-A/Abo using TWSTRS (ratio 1:4 or 1:5 BoNT-A/Ona:BoNT-A/Abo) [75]. Better efficacy for BoNT-A/Abo compared with BoNT-A/Ona based on Tsui and TWSTRS (ratio 1:3 or 1:4 BoNT-A/Ona:BoNT-A/Abo) was instead reported by Ranoux et al. [76].
In comparing safety, a literature survey analysed 70 published articles in CD: 30 used BoNT-A/Ona, 24 used BoNT-A/Abo, 3 used BoNT-A/Ona + BoNT-A/Abo, 11 used BoNT-B/Rima and 2 used B-BoNT-A/Ona + BoNT-B/Rima. The mean total doses per treatment ranged from 60 to 374 U for BoNT-A/Ona, 125 to 1200 U for BoNT-A/Abo and 579 to 19,853 U for BoNT-B/Rima [77]. BoNT-A/Ona was associated with a significantly lower rate of dysphagia than BoNT-A/Abo: 10.5 % for original Botox (original 79-11 lot), 8.9 % for BoNT-A/Ona (current Botox) and 26.8 % for BoNT-A/Abo (both, P < 0.05). BoNT-B/Rima was associated with dry mouth (3.2–90.0 %) in 9 of 13 studies, but this effect was not reported in a sufficient number of BoNT-A studies (BoNT-A/Ona, n = 2; BoNT-A/Abo, n = 6) to permit statistical comparison.
Studies of the equivalence between BoNT-A/Ona to BoNT-A/Inco have produced much more consistent results. One preclinical study showed some minor differences [78], but these differences may be attributable to assay methodology. A more recent study has demonstrated equivalence between the two formulations [50]. In clinical evaluations, the equivalence of these two products has been reliably and repeatedly demonstrated [50, 59, 65, 73, 79–84].
BoNT-A/Ona and BoNT-A/Inco have been shown to have comparable efficacy and tolerability in healthy volunteers [79] and to have a similar duration of action in CD which does not show any ‘wearing off’ in up to 66 cycles of use [65, 73]. The ease of product switch, using a dose conversion ratio of 1:1, was demonstrated in a study of 263 patients, treated with BoNT-A/Ona for at least 1 year under stable conditions who were then converted to BoNT-A/Inco. After 3 years’ treatment, no subjective or objective differences were observed between BoNT-A/Ona and BoNT-A/Inco with respect to onset latency, maximum and duration of effect or adverse event profiles and there were no detectable differences in diffusion [73, 82].
When non-response is an issue, the treating physician should consider whether insufficient dosing or inappropriate or incomplete muscle selection are responsible [4]. If these approaches are not successful, then switching from BoNT-A to BoNT-B should be considered.
BoNT-A to BoNT-B switching is not a simple matter. There are large variations in conversion factors depending on the system used to compare the two toxin subtypes. The brow-furrow test suggests that conversion ratios of 50:1 or 100:1 (B:A) are effective—the latter producing a longer-lasting effect [85]; spasmodic dysphonia 52.3:1 [86]; skin model (29:1) [87]. Therefore, a practical approach is to start the new toxin at a lower dose than would be expected from conversion calculations (which are inaccurate) and then titrate upwards in relation to the patient’s response.
Conclusion
CD is a neurological movement disorder that can affect both posture and movement of the head and neck, sometimes involving the shoulders. CD has varied and complex phenomenology, involving different muscles and combinations of muscles, more superficial or deeper, which may be affected in varying degrees and show different patterns of contraction—tonic, spasmodic, tremulous or a complex mixture. Treatment of CD should thus be tailored to the patients’ specific needs. BoNT-A is the first treatment of choice for CD. The aim of this publication has been to try and supply a consensus expert opinion on practical aspects of treatment for injectors to assist them in obtaining the highest degree of treatment satisfaction for their patients.
Abbreviations
- BoNT:
-
Botulinum neurotoxin
- BoNT-A:
-
Botulinum neurotoxin type A
- BoNT-B:
-
Botulinum neurotoxin type B
- CD:
-
Cervical dystonia
- HRQoL:
-
Health related quality of life
- QoL:
-
Quality of life
References
Charles PD, Adler CH, Stay M et al (2014) Cervical dystonia and pain: characteristics and treatment patterns from CD PROBE (Cervical Dystonia Patient Registry for Observation of OnabotulinumtoxinA Efficacy). J Neurol 261:13019–13098
Camfield L, Ben-Shlomo T, Warner TT (2002) Impact of cervical dystonia on quality of life. Mov Disord 17:838–841
Jankovic J, Adler CH, Charles PD et al (2011) Rational and design of a prospective study: cervical Dystonia Patient Registry for Observation of OnaBotulinumtoxinA Efficacy (CD PROBE). BMC Neurology 11:140
Swope D, Barbano R (2008) Treatment recommendations and practical applications of botulinum toxin treatment of cervical dystonia. Neurol Clin 26(Suppl 1):54–65
Albanese A, Asmus F, Bhatia KP et al (2011) EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol 18:5–18
Simpson DM, Blitzer A, Brashear A (2008) Assessment: botulinum neurotoxin for the treatment of movement disorders (an evidence based review): report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology 70:1699–1706
Murphy MK, Black NA, Lamping DL et al (1998) Consensus development methods, and their use in clinical guideline development. Health Technol Assess 2(no 3):1–88
Jankovic J (2006) Treatment of dystonia. Lancet Neurol 5:864–872
Tassorelli C, Mancini F, Balloni L et al (2006) Botulinum toxin and neuromotor rehabilitation: an integrated approach to idiopathic cervical dystonia. Mov Disord 21:2240–2243
Volkmann J, Mueller J, Deuschl G et al (2014) DBS study group for dystonia. Pallidal neurostimulation in patients with medication-refractory cervical dystonia: a randomised, sham-controlled trial. Lancet Neurol 13(9):875–884. doi:10.1016/S1474-4422(14)70143-7 (Epub 2014 Aug 7)
Skogseid IM, Ramm-Pettersen J, Volkmann J, Kerty E, Dietrichs E, Røste GK (2012) Good long-term efficacy of pallidal stimulation in cervical dystonia: a prospective, observer-blinded study. Eur J Neurol 19(4):610–615. doi:10.1111/j.1468-1331.2011.03591.x Epub 2011 Nov 25
Albanese A, Barnes MP, Bhatia KP et al (2006) A systematic review on the diagnosis and treatment of primary (idiopathic) dystonia and dystonia plus syndromes: report of an EFNS/MDS-ES task force. Eur J Neurol 13:433–444
Colosimo C, Supa A, Fabbrini G et al (2010) Craniocervical dystonia: clinical and pathophysiological features. Eur J Neurol 17(Suppl 1):15–21
Zoons E, Dijkgraaf MGW, Dijk JM et al (2012) Botulinum toxin as treatment for focal dystonia: a systematic review of the pharmaco-therapeutic and pharmaco-economic value. J Neurol 259:2519–2526
Dressler D, Rothwell JC (2000) Electromyograpjc quantification of the paralysing effect of botulinum toxin in the sternocleidomastoid muscle. Eur Neurol 43(1):13–16
Meija NI, Vuong KD, Jankovic J (2005) Long-term botulinum toxin efficacy, safety, and immunogenicity. Mov Disord 20(5):592–597
Colosimo C, Tiple D, Berardelli A (2012) Efficacy and safety of long-term botulinum treatment in craniocervical dystonia: a systematic review. Neurotox Res 22:265–273
Truong D (2012) Botulinum toxins in the treatment of primary focal dystonias. J Neurolog Sci 316:9–14
Jankovic J, Leder S, Warner D, Schwartz K (1991) Cervical dystonia: clinical findings and associated movement disorders. Neurology 41:1088–1091
Skogseid IM, Kerty E (2005) The course of cervical dystonia and patient satisfaction with long-term botulinum toxin A treatment. Eur J Neurol 12(3):163–170
Skogseid IM, Røislien J (2005) Claussen, Kerty E. Long-term botulinum toxin treatment increases employment rate in patients with cervical dystonia. Mov Disord 20:1604–1609
Bove M, Brichetto G, Abbruzzese G, Marchese R, Schieppate M (2004) Neck proprioception and spatial orientation in cervical dystonia. Brain 127(Pt 12):2764–2778
Pelosin E, Bove M, Marinelli L, Abbruzzese G, Ghilardi MF (2009) Cervical dystonia affects aimed movements of nonodystonic segments. Mov Disord 24(13):1955–1961
Stamelou M, Edwards MJ, Hallett M, Bhatia KP (2012) The non-motor syndrome of primary dystonia: clinical and pathophysiological implications. Brain 135:1668–1681
Comella CL, Stebbins GT, Miller S (1996) Specific dystonic factors contributing to work limitation and disability in cervical dystonia. Neurology 46(Suppl 2):A259
Stacy M (2008) Epidemiology, clinical presentation, and diagnosis of cervical dystonia. Neurol Clin 26(Suppl 1):23–42
Skogseid IM, Malt UF, Røislien J, Kerty E (2007) Determinants and status of quality of life after long-term botulinum toxin therapy for cervical dystonia. Eur J Neurol 14:1129–1137
Slawek J, Friedman A, Potulska A et al (2007) Factors affecting health-related quality of life of patients with cervical dystonia and the impact of botulinum toxin type A injections. Funct Neurol 22(2):95–100
Hefter H, Benecke R, Erbguth F et al (2013) An open-label cohort study of the improvement in quality of life and pain in de novo cervical dystonia patients after injections with 500U botulinum toxin (Dysport). BMJ Open. doi:10.1136/bmjopen-2112-001853
Ben-Shlomo Y, Camfield L, Warner T, ESDE collaborative group (2002) what are the determinants of quality of life in people with cervical dystonia? J Neurol Neurosurg Psychiatry 72:608–614
Sethi KD, Rodriguez R, Olayinka B (2012) Satisfaction with botulinum toxin treatment: a cross-sectional survey of patients with cervical dystonia. J Med Econ 15:1–5
Albanese A, Bhatia K, Bressman SB et al (2013) Phenomenology and classification of dystonia: a consensus update. Mov Disord 28(7):863–873
Albanese A, Lalli S (2009) Is this dystonia? Mov Disord 24(12):1725–1731
Lalli S, Albanese A (2010) The diagnostic challenge of primary dystonia: evidence from misdiagnosis. Mov Disord 25(11):1619–1626
Moore P, Naumann M (2003) General and clinical aspects of treatment with botulinum toxin. In: Moore P, Naumann M (eds) Handbook of botulinum toxin treatment, 2nd edn. Blackwell Science, Oxford
Albanese A, Sorbo FD, Comella C et al (2013) Dystonia rating scale: critique and recommendations. Mov Disord 28:874–883
Dressler D, Kupsch A, Seitzinger A, Paus S (2014) The Dystonia Discomfort Scale (DDS): a novel instrument to monitor the temporal profile of botulinum toxin therapy in cervical dystonia. Eur J Neurol. doi:10.1111/ene.12330
Reichel G (2011) Cervical dystonia: a new phenomenological classification for botulinum toxin therapy. Basal Ganglia 1:5–12
Flowers JM, Hicklin LA, Marion M-H (2011) Anterior and posterior sagittal shift in cervical dystonia: a clinical and electromyographic study, including a new EMG approach of the longus colli muscle. Mov Disord 26(13):2409–2414. doi:10.1002/mds.23905
Dressler D (2000) Electromyographic evaluation of cervical dystonia for planning of botulinum toxin therapy. Eur J Neurol 7(6):713–718
Lim ECH, Quek AML, Seet RCS (2012) Accurate targeting of botulinum toxin injections: how to and why. Parkinson Rel Dis 17:S34–S39
Botox SmPC. http://www.medicines.org.uk/emc/medicine/112
Dysport SmPC. http://www.medicines.org.uk/emc/medicine/870
Xeomin SmPC. http://www.medicines.org.uk/emc/medicine/20666
Neurobloc SmPC. http://www.medicines.org.uk/emc/medicine/20568/SPC
Bentovglio AR, Bagella CF, Albanese A (2015) Botulinum toxin in movement disorders. In: Jankovic J, Tolosa E (eds) Parkinson’s disease & Movement Disorders, 6th edn. Wolters Kluver, Philadelphia, pp. 480–495
De Pauw J, Van der Velden K, Meirte J et al (2014) The effectiveness of physiotherapy for cervical dystonia: a systematic literature review. J Neurol 261(10):1857–1865. doi:10.1007/s00415-013-7220-8
Greene P, Kang U, Fahn S et al (1990) Double-blind, placebo-controlled trial of botulinum toxin injections for the treatment of spasmodic torticollis. Neurology 40:1213–1218
Misra VP, Ehler E (2012) Zakine B et al Factors influencing response to Botulinum toxin type A in patients with idiopathic cervical dystonia: results from an international observational study. BMJ Open 2:e000881
Dressler D, Tacik P, Adib Saberi F (2015) Botulinum toxin therapy of cervical dystonia: duration of therapeutic effects. J Neural Transm 122(2):297–300
Evidente VGH, Fernandez HH, LeDoux MS et al (2013) A randomized, double-blind study of repeated incobotulinum toxinA (Xeomin®) in cervical dystonia. J Neural Trans 120(12):1699–1707
Comella CL, Jankovic J, Truong DD et al (2011) Efficacy and safety of incobotulinumtoxin A (NT 201, Xeomin® botulinum neurotoxin type A, without accessory proteins) in patients with cervical dystonia. J Neurol Sci 208:103–109
Naumann M, Jankovic J (2004) Safety of botulinum toxin type A: a systematic review and meta-analysis. Curr Med Res Opin 20:981–990
Borodic GE, Joseph M, Fay L et al (1990) Botulinum toxin for the treatment of spasmodic torticollis: dysphagia and regional toxin spread. Head Neck 12:392–399
Borodic GE, Ferrante R, Pearce LB, Smith K (1994) Histologic assessment of dose-related diffusion and muscle fiber response after therapeutic botulinum-A-toxin injection. Mov Disord 9:31–39
Hsu TS, Dover JS, Arndt KA (2004) Effect of volume and concentration on the diffusion of botulinum exotoxinA. Arch Dermatol 140:1351–1354
Carli L, Montecucco C, Rossatto O (2009) Assay of diffusion of different botulinum toxin type a formulations. Musc Nerve 40:374–380
Tang-Liu DD, Aoki KR, Dolly JO et al (2003) Intramuscular injection of 125I- botulinum neurotoxin-complex versus 125I-botulinum-free neurotoxin: time course of tissue distribution. Toxicon 42:461–469
Frevert J, Dressler D (2010) Complexing proteins in botulinum toxin type A drugs: a help or a hindrance? Biologics Targets Ther 10:325–332
Benecke R, Moore P, Dressler D, Nauman M (2003) Cervical and axial dystonia. In: Moore P, Nauman M (eds) Handbook of botulinum toxin treatment, chap 8, 2nd edn. Blackwell Science, Oxford
Aranda MA, Herranz A, del Val J, Belido S, Garcia-Ruiz P (2012) Botulinum toxin A during pregnancy, still a debate. Eur J Eurol 19:e81–e82
Brin MF, Comella CL, Jankovic J et al (2008) Long-term treatment with botulinum toxin type A in cervical dystonia has low antigenicity by mouse protection assay. Mov Disord 23:1353–1360
Dressler D (1997) Botulinum toxin therapy failure: causes, evaluation procedures and management strategies. Eur J Neurol 4(suppl 2):S67–S70
Ferreria JJ, Bhidayasiri R, Colosimo C et al (2012) Survey of practices employed by neurologists for the definition and management of secondary non-response to botulinum toxin in cervical dystonia. Funct Neurol 27(4):225–230
Jost WH, Blumel J, Grafe S (2007) Botulinum neurotoxin type A free of complexing proteins (XEOMIN®) in focal dystonia. Drugs 67:669–683
Cordivari C, Misra VP, Vincent A et al (2006) Secondary nonresponsiveness to botulinum toxin A in cervical dystonia: the role of electromyogram-guided injections, botulinum toxin A antibody assay, and the extensor digitorum brevis test. Mov Disord 21:1737–1741
Dressler D, Gessler F, Tacik P, Bigalke H (2014) An enzyme-linked immunosorbent assay for detection of botulinum toxin antibodies. Mov Disord 29(10):1322–1324. doi:10.1002/mds.25956
Walsh RA, Sidiropoulos C, Lozano AM et al (2013) Bilateral pallidal stimulation in cervical dystonia: blinded evidence of benefit beyond 5 years. Brain 136:761–769
Wohlfarth K, Schwandt I, Wegner F et al (2008) Biological activity of two botulinum toxin type A complexes (Dysport and Botox) in volunteers: a double-blind, randomized, dose-ranging study. J Neurol 255(12):1932–1939
Marchetti A, Magar R et al (2005) Retrospective Evaluation of the Dose of Dysport and BOTOX in the Management of Cervical Dystonia and Blepharospasm: The REAL DOSE Study. Mov Disord 20(8):937–944
Wohlfarth K, Sycha T, Ranoux D et al (2009) Dose equivalence in two preparations of botulinum toxin type A: time for a reassessment? Curr Med Res Opin 25:1573–1584
Grosset DG, Tyrrell EG, Grosset KA (2013) Conversion from Dysport® to Xeomin® formulation of botulinum toxin: clinical experience in 257 cases. Botulinum J 2(3/4):276
Dressler D, Tacik P, Adib Saberi F (2014) Botulinum toxin therapy of cervical dystonia: comparing onabotulinumtoxin A (Botox®) and incobotulinumtoxin A (Xeomin®). J Neural Trans 121:29–31
Odergren T, Hjaltason H (1998) Kaakkola S et al A double-blind randomised, parallel-group study to investigate the dose equivalence of Dysport and Botox in the treatment of cervical dystonia. J Neurol Neurosurg Psychiatr 64:6–12
Bihari K (2005) Safety, effectiveness and duration of effect of BOTOX compared with Dysport for blepharospasm, cervical dystonia and hemifacial spasm. Curr Med Res Opin 21(3):433–438
Ranoux D et al (2002) Respective potencies of Botox and Dysport: a double blind, randomized, crossover study in cervical dystonia. J Neurol Neurosurg Psychiatry 72:459–462
Chapman MA, Barron R, Tanis DC et al (2007) Comparison of botulinum neurotoxin preparations for the treatment of cervical dystonia. Clin Ther 29:1325–1337
Hunt T, Clarke K (2009) Potency evaluation of a formulated drug product containing 150-kd botulinum neurotoxin type A. Clin Neuropharm 32:28–31
Jost WH, Kohl A, Brinkmann S, Comes G (2005) Efficacy and tolerability of a botulinum toxin type A free of complexing proteins (NT201) compared with commercially available boutlinum toxin type A (BOTOX®) in healthy volunteers. J Neural Transm 112:905–913
Benecke R, Jost WH, Kanovsky P et al (2005) A new botulinum toxin type A free of complexing proteins for treatment of cervical dystonia. Neurology 64:1949–1951
Roggenkämper P, Jost WH, Bihari K et al (2006) Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. J Neural Trans 113:303–312
Dressler D (2009) Routine use of Xeomin in patients previously treated with Botox: long-term results. Eur J Neurol 16(Suppl 2):2–5
Benecke R (2009) Current status of the use of botulinum neurotoxin type A. Eur J Neurol 16(Suppl 2):1. doi:10.1111/j.1468-1331.2009.02876.x
Benecke R, Hauschke D (2013) IncobotulinumtoxinA demonstrated equivalent efficacy to onabotulinumtoxinA in the treatment of cervical dystonia. Botulinum J 2(3/4):217
Lowe NJ, Yamauchi PS, Lask GP et al (2002) Botulinum toxins types A and B for brow furrows: preliminary experience with type B toxin dosing. J Cosmet Laser Ther 4:15–18
Blitzer A (2005) Botulinum toxin A and B: a comparative dosing study for spasmodic dysphonia. Otolaryngol Head and Neck Surg 133:836–838
Kranz G, Paul A, Voller B et al (2011) Long-term efficacy and respective potencies of botulinum toxin A and B: a randomized, double-blind study. Br J Dermatol 164:176–181
Poewe W, Deuschl G, Nebe A et al (1998) What is the optimal dose of botulinum toxin A in the treatment of cervical dystonia? Results of a double-blind placebo controlled dose ranging study of Dysport. German Dystonia Study Group. J Neurol Neurosurg Psychiatr 64:13–17
Truong D, Duane DD, Jankovic J et al (2005) Efficacy and safety of botulinum type A toxin (Dysport) in cervical dystonia: results of the first US randomised, double-blind, placebo-controlled study. Mov Disord 20:783–791
Truong DD, Brodsky M (2010) Lew M et al Long-term efficacy and safety of botulinum toxin type A (Dysport) in cervical dystonia. Parkinsonism Relat Disord 16:316–323
Brans JW, Lindeboom R (1996) Snoek JW et al Botulinum toxin versus trihexyphenidyl in cervical dystonia: a prospective, randomized, double-blind controlled trial. Neurology 46:1066–1072
Pappert EJ, Germanson T, Myobloc/Neurobloc European Cervical Dystonia Study Group (2008) Botulinum toxin type B vs. type A in toxin naive patients with cervical dystonia: randomized, double-blind, noninferiority trial. Mov Disord 23:510–517
Comella CL, Jankovic J, Shannon KM, Dystonia Study Group et al (2005) Comparison of botulinum toxin serotypes A and B for the treatment of cervical dystonia. Neurology 65:1423–1429
Novak Campbell L, Boyce M, Fung VSC (2010) Botulinum toxin assessment, intervention and aftercare for cervical dystonia and other causes of hypertonia of the neck: international consensus statement. Eur J Neurol 17(Suppl 2):94–108
Conflicts of interest
Professor Albanese has received speaker fees from Allergan, Ipsen and Merz. Dr Duzynski has received speaker fees from Allergan, Ipsen and Orion Pharma. Dr Khatkova has received training fees from Ipsen, Merz Ltd. and Allergan Inc. and meeting sponsorship from Ipsen, Merz Ltd. and Allergan Inc. Dr Marti has undertaken consultancy work for Ipsen, Merz, Allergan and Abvie. Dr Moro has received honoraria from Medtronic, Boston Scientific and UCB for consulting and lecturing. Dr Roze is the recipient of a grant “poste d’accueil” AP-HP/CNRS. He received research support from INSERM (COSSEC), AP-HP (DRC-PHRC), Fondation pour la Recherche sur le Cerveau (FRC), the Dystonia Coalition (Pilot project), Ipsen, and Merz-Pharma, Novartis, Teva, Lundbeck and Orkyn; served on scientific advisory boards for Orkyn, Ipsen and Merz-pharma; received speech honorarium from Novartis, Teva and Orkyn; received travel funding from Teva, Novartis, the Dystonia Coalition, the Movement Disorders Society, the World Federation of Neurology Association of Parkinsonism and Related Disorders and International Federation of Clinical Neurophysiology. Dr Timerbaeva has received honoraria from Allergan, Ipsen and Merz. Professor Abbruzzese, Professor Montecucco, Dr Mir, Professor Pinter, Professor Relja and Dr Tzoulis have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Albanese, A., Abbruzzese, G., Dressler, D. et al. Practical guidance for CD management involving treatment of botulinum toxin: a consensus statement. J Neurol 262, 2201–2213 (2015). https://doi.org/10.1007/s00415-015-7703-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7703-x