Abstract
Background
Amyotrophic lateral sclerosis (ALS) is a global disease, which adversely affects the life quality of patients and significantly increases the burden of families and society. We aimed to assess the changing incidence, prevalence of ALS around the world.
Methods
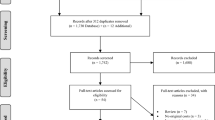
We searched Medline, Embase, Web of Science, and Cochrane library to identify articles published until September 9, 2018. Each included study was independently reviewed for methodological quality by two reviewers. We used a random-effects model to summarize individual studies and assessed heterogeneity (I2) with the χ2 test on Cochrane’s Q statistic.
Results
We identified 124 studies that were eligible for final inclusion, including 110 studies of incidence and 58 studies of prevalence. The overall crude worldwide ALS prevalence and incidence were 4.42 (95% CI 3.92–4.96) per 1,00,000 population and 1.59 (95% CI 1.39–1.81) per 1,00,000 person-years, respectively. ALS prevalence and incidence increased by age until the age of 70–79. Since 1957, incidence has been significantly rising year by year, and this upward trend was weakened after standardization. The longest survival time were in Asia (ranging from 3.74 years in South Asia to 9.23 years in West Asia).
Conclusions
With the aggravation of population aging and the rapid growth of economy, developing regions following the development pattern of the developed regions may suffer rising ALS prevalence and incidence which may increase their disease burden as well. These data highlight the need for research into underlying mechanism and innovations in health-care systems.





Similar content being viewed by others
References
Brown RH, Al-Chalabi A (2017) Amyotrophic lateral sclerosis. N Engl J Med 377:162–172. https://doi.org/10.1056/NEJMra1603471
Montuschi A, Iazzolino B, Calvo A, Moglia C, Lopiano L, Restagno G, Brunetti M, Ossola I, Lo Presti A, Cammarosano S, Canosa A, Chio A (2015) Cognitive correlates in amyotrophic lateral sclerosis: a population-based study in Italy. J Neurol Neurosurg Psychiatry 86:168–173. https://doi.org/10.1136/jnnp-2013-307223
Phukan J, Elamin M, Bede P, Jordan N, Gallagher L, Byrne S, Lynch C, Pender N, Hardiman O (2012) The syndrome of cognitive impairment in amyotrophic lateral sclerosis: a population-based study. J Neurol Neurosurg Psychiatry 83:102–108. https://doi.org/10.1136/jnnp-2011-300188
Logroscino G, Piccininni M, Marin B, Nichols E, Abd-Allah F, Abdelalim A, Alahdab F, Asgedom SW, Awasthi A, Chaiah Y, Daryani A, Do HP, Dubey M, Elbaz A, Eskandarieh S, Farhadi F, Farzadfar F, Fereshtehnejad S-M, Fernandes E, Filip I, Foreman KJ, Gebre AK, Gnedovskaya EV, Hamidi S, Hay SI, Irvani SSN, Ji JS, Kasaeian A, Kim YJ, Mantovani LG, Mashamba-Thompson TP, Mehndiratta MM, Mokdad AH, Nagel G, Nguyen TH, Nixon MR, Olagunju AT, Owolabi MO, Piradov MA, Qorbani M, Radfar A, Reiner RC, Sahraian MA, Sarvi S, Sharif M, Temsah O, Tran BX, Truong NT, Venketasubramanian N, Winkler AS, Yimer EM, Feigin VL, Vos T, Murray CJL (2018) Global, regional, and national burden of motor neuron diseases 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 17:1083–1097. https://doi.org/10.1016/s1474-4422(18)30404-6
Baeza-Yates R, Sangal PM, Villoslada P (2017) Burden of neurological diseases in the US revealed by web searches. PLoS ONE 12:e0178019. https://doi.org/10.1371/journal.pone.0178019
Tysnes OB, Vollset SE, Aarli JA (1991) Epidemiology of amyotrophic lateral sclerosis in Hordaland county, western Norway. Acta Neurol Scand 83:280–285
Benjaminsen E, Alstadhaug KB, Baloch F, Gulsvik M, Odeh F (2017) Amyotrophic lateral sclerosis in Nordland County, Norway 2000–2015. Eur J Neurol 24:28
Tsai C-P, Wang K-C, Hwang C-S, Lee IT, Lee CT-C (2015) Incidence, prevalence, and medical expenditures of classical amyotrophic lateral sclerosis in Taiwan, 1999–2008. J Formos Med Assoc 114:612–619. https://doi.org/10.1016/j.jfma.2013.01.008
McKenzie JE, Beller EM, Forbes AB (2016) Introduction to systematic reviews and meta-analysis. Respirology 21:626–637. https://doi.org/10.1111/resp.12783
Marin B, Boumediene F, Logroscino G, Couratier P, Babron MC, Leutenegger AL, Copetti M, Preux PM, Beghi E (2017) Variation in worldwide incidence of amyotrophic lateral sclerosis: a meta-analysis. Int J Epidemiol 46:57–74. https://doi.org/10.1093/ije/dyw061
Chio A, Logroscino G, Traynor BJ, Collins J, Simeone JC, Goldstein LA, White LA (2013) Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology 41:118–130. https://doi.org/10.1159/000351153
D'Ovidio F, d'Errico A, Farina E, Calvo A, Costa G, Chio A (2016) Amyotrophic lateral sclerosis incidence and previous prescriptions of drugs for the nervous system. Neuroepidemiology 47:59–66. https://doi.org/10.1159/000448618
Moura MC, Casulari LA, Carvalho Garbi Novaes MR (2016) Ethnic and demographic incidence of amyotrophic lateral sclerosis (ALS) in Brazil: a population based study. Amyotroph Lateral Scler Frontotemporal Degener 17:275–281. https://doi.org/10.3109/21678421.2016.1140210
Scialo C, Novi G, Bandettini di Poggio M, Canosa A, Sormani MP, Mandich P, Origone P, Truffelli R, Mancardi GL, Caponnetto C (2016) Clinical epidemiology of amyotrophic lateral sclerosis in Liguria, Italy: an update of LIGALS register. Amyotroph Lateral Scler Frontotemporal Degener 17:535–542. https://doi.org/10.1080/21678421.2016.1197942
Tesauro M, Consonni M, Filippini T, Mazzini L, Pisano F, Chio A, Esposito A, Vinceti M (2017) Incidence of amyotrophic lateral sclerosis in the province of Novara, Italy, and possible role of environmental pollution. Amyotroph Lateral Scler Frontotemporal Degener 18:284–290. https://doi.org/10.1080/21678421.2017.1281961
Weil C, Zach N, Rishoni S, Shalev V, Chodick G (2016) Epidemiology of amyotrophic lateral sclerosis: a population-based study in Israel. Neuroepidemiology 47:76–81. https://doi.org/10.1159/000448921
Demetriou CA, Hadjivasiliou PM, Kleopa KA, Christou YP, Leonidou E, Kyriakides T, Zamba-Papanicolaou E (2017) Epidemiology of amyotrophic lateral sclerosis in the Republic of Cyprus: a 25-year retrospective study. Neuroepidemiology 48:79–85. https://doi.org/10.1159/000477126
Kahana E, Alter M, Feldman S (1976) Amyotrophic lateral sclerosis: a population study. J Neurol 212:205–213
Okumiya K, Wada T, Fujisawa M, Ishine M, Garcia Del Saz E, Hirata Y, Kuzuhara S, Kokubo Y, Seguchi H, Sakamoto R, Manuaba I, Watofa P, Rantetampang AL, Matsubayashi K (2014) Amyotrophic lateral sclerosis and parkinsonism in Papua, indonesia: 2001–2012 survey results. BMJ open 4:e004353. https://doi.org/10.1136/bmjopen-2013-004353
Boyle MH (1998) Guidelines for evaluating prevalence studies. Evid Based Ment Health 1:37–39
Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW (1998) Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can 19:170–176
Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, Pringsheim T, Lorenzetti DL, Jette N (2017) Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology 88:296–303. https://doi.org/10.1212/wnl.0000000000003509
Noubiap JJ, Bigna JJ, Nansseu JR, Nyaga UF, Balti EV, Echouffo-Tcheugui JB, Kengne AP (2018) Prevalence of dyslipidaemia among adults in Africa: a systematic review and meta-analysis. Lancet Glob Health 6:e998–e1007. https://doi.org/10.1016/s2214-109x(18)30275-4
Noubiap JJ, Nansseu JR, Nyaga UF, Nkeck JR, Endomba FT, Kaze AD, Agbor VN, Bigna JJ (2019) Global prevalence of diabetes in active tuberculosis: a systematic review and meta-analysis of data from 2.3 million patients with tuberculosis. Lancet Glob Health 7:e448–e460. https://doi.org/10.1016/s2214-109x(18)30487-x
Etminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A (2019) Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA neurol 76:588–597. https://doi.org/10.1001/jamaneurol.2019.0006
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG (2018) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390:2769–2778. https://doi.org/10.1016/s0140-6736(17)32448-0
Freeman J, Hutchison GB (1980) Prevalence, incidence and duration. Am J Epidemiol 112:707–723. https://doi.org/10.1093/oxfordjournals.aje.a113043
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Marin B, Fontana A, Arcuti S, Copetti M, Boumediene F, Couratier P, Beghi E, Preux PM, Logroscino G (2018) Age-specific ALS incidence: a dose-response meta-analysis. Eur J Epidemiol 33:621–634. https://doi.org/10.1007/s10654-018-0392-x
Taskent RO, Gokcumen O (2017) The Multiple histories of Western Asia: perspectives from ancient and modern genomes. Hum Biol 89:107–117
Anne MB, Judith RK, Joanna LM, Joan MH, Luciano C, Kenneth KK, Luca LC (1991) Drift, admixture, and selection in human evolution: a study with DNA polymorphisms. Proc Nati Acad Sci 88:839–843
Luca LCS (1997) Genes, peoples, and languages. Proc Natl Acad Sci 94:7719–7724
van Es MA, Veldink JH, Saris CG, Blauw HM, van Vught PW, Birve A, Lemmens R, Schelhaas HJ, Groen EJ, Huisman MH, van der Kooi AJ, de Visser M, Dahlberg C, Estrada K, Rivadeneira F, Hofman A, Zwarts MJ, van Doormaal PT, Rujescu D, Strengman E, Giegling I, Muglia P, Tomik B, Slowik A, Uitterlinden AG, Hendrich C, Waibel S, Meyer T, Ludolph AC, Glass JD, Purcell S, Cichon S, Nothen MM, Wichmann HE, Schreiber S, Vermeulen SH, Kiemeney LA, Wokke JH, Cronin S, McLaughlin RL, Hardiman O, Fumoto K, Pasterkamp RJ, Meininger V, Melki J, Leigh PN, Shaw CE, Landers JE, Al-Chalabi A, Brown RH Jr, Robberecht W, Andersen PM, Ophoff RA, van den Berg LH (2009) Genome-wide association study identifies 19p13.3 (UNC13A) and 9p21.2 as susceptibility loci for sporadic amyotrophic lateral sclerosis. Nat Genet 41:1083–1087. https://doi.org/10.1038/ng.442
Diekstra FP, Saris CG, van Rheenen W, Franke L, Jansen RC, van Es MA, van Vught PW, Blauw HM, Groen EJ, Horvath S, Estrada K, Rivadeneira F, Hofman A, Uitterlinden AG, Robberecht W, Andersen PM, Melki J, Meininger V, Hardiman O, Landers JE, Brown RH Jr, Shatunov A, Shaw CE, Leigh PN, Al-Chalabi A, Ophoff RA, van den Berg LH, Veldink JH (2012) Mapping of gene expression reveals CYP27A1 as a susceptibility gene for sporadic ALS. PLoS ONE 7:e35333. https://doi.org/10.1371/journal.pone.0035333
Uyan O, Omur O, Agim ZS, Ozoguz A, Li H, Parman Y, Deymeer F, Oflazer P, Koc F, Tan E, Ozcelik H, Basak AN (2013) Genome-wide copy number variation in sporadic amyotrophic lateral sclerosis in the Turkish population: deletion of EPHA3 is a possible protective factor. PLoS ONE 8:e72381. https://doi.org/10.1371/journal.pone.0072381
Fogh I, Ratti A, Gellera C, Lin K, Tiloca C, Moskvina V, Corrado L, Soraru G, Cereda C, Corti S, Gentilini D, Calini D, Castellotti B, Mazzini L, Querin G, Gagliardi S, Del Bo R, Conforti FL, Siciliano G, Inghilleri M, Sacca F, Bongioanni P, Penco S, Corbo M, Sorbi S, Filosto M, Ferlini A, Di Blasio AM, Signorini S, Shatunov A, Jones A, Shaw PJ, Morrison KE, Farmer AE, Van Damme P, Robberecht W, Chio A, Traynor BJ, Sendtner M, Melki J, Meininger V, Hardiman O, Andersen PM, Leigh NP, Glass JD, Overste D, Diekstra FP, Veldink JH, van Es MA, Shaw CE, Weale ME, Lewis CM, Williams J, Brown RH, Landers JE, Ticozzi N, Ceroni M, Pegoraro E, Comi GP, D'Alfonso S, van den Berg LH, Taroni F, Al-Chalabi A, Powell J, Silani V (2014) A genome-wide association meta-analysis identifies a novel locus at 17q11.2 associated with sporadic amyotrophic lateral sclerosis. Hum Mol Genet 23:2220–2231. https://doi.org/10.1093/hmg/ddt587
Du Y, Wen Y, Guo X, Hao J, Wang W, He A, Fan Q, Li P, Liu L, Liang X, Zhang F (2018) A Genome-wide expression association analysis identifies genes and pathways associated with amyotrophic lateral sclerosis. Cell Mol Neurobiol 38:635–639. https://doi.org/10.1007/s10571-017-0512-2
Shatunov A, Mok K, Newhouse S, Weale ME, Smith B, Vance C, Johnson L, Veldink JH, van Es MA, van den Berg LH, Robberecht W, Van Damme P, Hardiman O, Farmer AE, Lewis CM, Butler AW, Abel O, Andersen PM, Fogh I, Silani V, Chio A, Traynor BJ, Melki J, Meininger V, Landers JE, McGuffin P, Glass JD, Pall H, Leigh PN, Hardy J, Brown RH Jr, Powell JF, Orrell RW, Morrison KE, Shaw PJ, Shaw CE, Al-Chalabi A (2010) Chromosome 9p21 in sporadic amyotrophic lateral sclerosis in the UK and seven other countries: a genome-wide association study. Lancet Neurol 9:986–994. https://doi.org/10.1016/s1474-4422(10)70197-6
Balendra R, Isaacs AM (2018) C9orf72-mediated ALS and FTD: multiple pathways to disease. Nat Rev Neurol 14:544–558. https://doi.org/10.1038/s41582-018-0047-2
Lloyd-Sherlock P (1982) (2000) Population ageing in developed and developing regions: implications for health policy. Soc Sci Med 51:887–895
A Chio G Mora C Moglia U Manera A Canosa S Cammarosano A Ilardi D Bertuzzo E Bersano P Cugnasco M Grassano F Pisano L Mazzini A Calvo VD Piemonte Register for ALS 2017 Secular trends of amyotrophic lateral sclerosis: the piemonte and valle d'aosta register, JAMA Neurol 74: 1097–1104 10.1001/jamaneurol.2017.1387
Arthur KC, Calvo A, Price TR, Geiger JT, Chio A, Traynor BJ (2016) Projected increase in amyotrophic lateral sclerosis from 2015 to 2040. Nat Commun 7:12408. https://doi.org/10.1038/ncomms12408
Shahrizaila N, Sobue G, Kuwabara S, Kim SH, Birks C, Fan DS, Bae JS, Hu CJ, Gourie-Devi M, Noto Y, Shibuya K, Goh KJ, Kaji R, Tsai CP, Cui L, Talman P, Henderson RD, Vucic S, Kiernan MC (2016) Amyotrophic lateral sclerosis and motor neuron syndromes in Asia. J Neurol Neurosurg Psychiatry 87:821–830. https://doi.org/10.1136/jnnp-2015-312751
Chen L, Zhang B, Chen R, Tang L, Liu R, Yang Y, Yang Y, Liu X, Ye S, Zhan S, Fan D (2015) Natural history and clinical features of sporadic amyotrophic lateral sclerosis in China. J Neurol Neurosurg Psychiatry 86:1075–1081. https://doi.org/10.1136/jnnp-2015-310471
Dorst J, Chen L, Rosenbohm A, Dreyhaupt J, Hubers A, Schuster J, Weishaupt JH, Kassubek J, Gess B, Meyer T, Weyen U, Hermann A, Winkler J, Grehl T, Hagenacker T, Lingor P, Koch JC, Sperfeld A, Petri S, Grosskreutz J, Metelmann M, Wolf J, Winkler AS, Klopstock T, Boentert M, Johannesen S, Storch A, Schrank B, Zeller D, Liu XL, Tang L, Fan DS, Ludolph AC (2019) Prognostic factors in ALS: a comparison between Germany and China. J Neurol 266:1516–1525. https://doi.org/10.1007/s00415-019-09290-4
Lee CT, Chiu YW, Wang KC, Hwang CS, Lin KH, Lee IT, Tsai CP (2013) Riluzole and prognostic factors in amyotrophic lateral sclerosis long-term and short-term survival: a population-based study of 1149 cases in Taiwan. J Epidemiol 23:35–40. https://doi.org/10.2188/jea.je20120119
Rabkin J, Ogino M, Goetz R, McElhiney M, Marziliano A, Imai T, Atsuta N, Morita M, Tateishi T, Matsumura T, Mitsumoto H (2013) Tracheostomy with invasive ventilation for ALS patients: neurologists' roles in the US and Japan. Amyotroph Lateral Scler Frontotemporal Degener 14:116–123. https://doi.org/10.3109/17482968.2012.726226
Floeter MK, Traynor BJ, Farren J, Braun LE, Tierney M, Wiggs EA, Wu T (2017) Disease progression in C9orf72 mutation carriers. Neurology 89:234–241. https://doi.org/10.1212/wnl.0000000000004115
Trojsi F, Siciliano M, Femiano C, Santangelo G, Lunetta C, Calvo A, Moglia C, Marinou K, Ticozzi N, Ferro C, Scialo C, Soraru G, Conte A, Falzone YM, Tortelli R, Russo M, Sansone VA, Chio A, Mora G, Silani V, Volanti P, Caponnetto C, Querin G, Sabatelli M, Riva N, Logroscino G, Messina S, Fasano A, Monsurro MR, Tedeschi G, Mandrioli J (2019) Comparative analysis of C9orf72 and sporadic disease in a large multicenter als population: the effect of male sex on survival of C9orf72 positive patients. Front Neurosci 13:485. https://doi.org/10.3389/fnins.2019.00485
Al-Chalabi A, Hardiman O (2013) The epidemiology of ALS: a conspiracy of genes, environment and time. Nat Rev Neurol 9:617–628. https://doi.org/10.1038/nrneurol.2013.203
Korner S, Kammeyer J, Zapf A, Kuzma-Kozakiewicz M, Piotrkiewicz M, Kuraszkiewicz B, Goszczynska H, Gromicho M, Grosskreutz J, Andersen PM, de Carvalho M, Petri S (2019) Influence of environment and lifestyle on incidence and progress of amyotrophic lateral sclerosis in A German ALS population. Aging Dis 10:205–216. https://doi.org/10.14336/ad.2018.0327
Beard JD, Steege AL, Ju J, Lu J, Luckhaupt SE, Schubauer-Berigan MK (2017) Mortality from amyotrophic lateral sclerosis and parkinson's disease among different occupation groups—United States, 1985–2011. MMWR Morb Mortal Wkly Rep 66:718–722. https://doi.org/10.15585/mmwr.mm6627a2
Mehta P, Kaye W, Raymond J, Punjani R, Larson T, Cohen J, Muravov O, Horton K (2018) Prevalence of amyotrophic lateral sclerosis—United States, 2015. MMWR Morb Mortal Wkly Rep 67:1285–1289. https://doi.org/10.15585/mmwr.mm6746a1
Acknowledgements
The authors would like to thank Xuefeng Lai, Jinlang Lv, Junyou Yu, Wei Zhang, and Huan Yu for retrieving and managing articles as well as extracting data.
Funding
This study was funded by the National Natural Science Foundation (grant number 91646107).
The manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, L., Liu, T., Liu, L. et al. Global variation in prevalence and incidence of amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol 267, 944–953 (2020). https://doi.org/10.1007/s00415-019-09652-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09652-y