Abstract
Background
The appropriate extent of gastric resection for patients with proximal third gastric cancer is controversial. This study addresses whether the choice of surgical strategy (proximal gastrectomy [PG] versus total gastrectomy [TG]) influences the outcomes for proximal third gastric adenocarcinoma.
Materials and methods
Review of prospective database at Tata Memorial Hospital from January 2010 to December 2012 identified 343 patients diagnosed and treated for gastric cancer. Of these, 75 underwent curative resections with D2 lymphadenectomy for proximal third gastric adenocarcinoma, which entailed proximal gastrectomy in 43 and total gastrectomy in 32 patients, depending on the epicenter of the primary and its relation with the mid-body of the stomach. Morbidity, lymph node yield, resection margins, patterns of recurrence, and survival were compared between these two groups.
Results
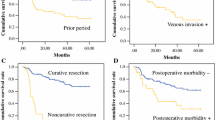
41/75 tumors were pT3 (23 cases [53.4 %] in the PG and 18 cases [56.3 %] in the TG group). Thirty-six patients [83.7 %] in PG and 29 patients [90.6 %] in TG group received neoadjuvant chemotherapy (NACT). There were no significant differences with regard to median blood loss, general complication rates and length of hospitalization between the two groups. The lymph node yield was comparable between the two procedures [PG = 14; TG = 15]. Positive proximal resection margin rates were comparable between the two groups [PG = 4.7 %; TG = 9.4 %], and there was no statistical difference observed in the distal resection margin positivity rates [PG = 4.7 %; TG = 3.1 %]. Regarding the patterns of recurrence, local recurrence in PG was 4.7 % and there was no local recurrence in the TG group (p = 0.08). Distant recurrence rates was dominant in TG [PG = 30.2 % versus TG = 53.1 %]. The overall 2-year survival following PG and TG was 73.8 and 49.9 %, respectively, and not statistically different (p = 0.10).
Conclusions
The extent of resection for proximal third gastric cancer does not influence the clinical outcome. PG and TG have similar survival rates. Both procedures can be accomplished safely. Therefore, PG should be an alternative to TG, even in locally advanced proximal gastric cancers treated by NACT, provided that the tumor size and location permit preservation of adequate remnant of stomach without compromising oncological resection margins. Future QOL studies would further lend credence to the concept of PG for proximal third gastric cancer.


Similar content being viewed by others
References
Parkin DM, Bray FI, Devesa SS (2001) Cancer burden in the year 2000. The global picture. Eur J Cancer 37(Suppl 8):S4–66
Crew KD, Neugut AI (2006) Epidemiology of gastric cancer. World J Gastroenterol 12:354–62
Shang J, Pena AS (2005) Multidisciplinary approach to understand the pathogenesis of gastric cancer. World J Gastroenterol 11:4131–9
Deans C, Yeo MSW, Soe MY, Shabbir A, Ti TK, So JBY (2011) Cancer of the gastric cardia is rising in incidence in an Asian population and is associated with adverse outcome. World J Surg 35:617–24. doi:10.1007/s00268-010-0935-0
Katai H (2006) Function-preserving surgery for gastric cancer. Int J Clin Oncol 11:357–66. doi:10.1007/s10147-006-0613-2
Gouzi JL, Huguier M, Fagniez PL, Launois B, Flamant Y, Lacaine F et al (1989) Total versus subtotal gastrectomy for adenocarcinoma of the gastric antrum. A French prospective controlled study. Ann Surg 209:162–6
Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, Gennari L (1999) Subtotal versus total gastrectomy for gastric cancer. Ann Surg 230:170
Papachristou DN, Fortner JG (1980) Adenocarcinoma of the gastric cardia. The choice of gastrectomy. Ann Surg 192:58–64
Jakl RJ, Miholic J, Koller R, Markis E, Wolner E (1995) Prognostic factors in adenocarcinoma of the cardia. Am J Surg 169:316–9
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines (ver.3). Gastric Cancer 14:113–23
Erturk MS, Cicek Y, Ersan Y (2016) Analysis of clinicopathologicalprognostic parameters in adenocarcinoma of the gastric cardia. Acta Chir Belg 103:611–5
Smith JW, Brennan MF (1992) Surgical treatment of gastric cancer. Proximal, mid, and distal stomach. Surg Clin North Am 72:381–99
Stipa S, Di Giorgio A, Ferri M (1992) Surgical treatment of adenocarcinoma of the cardia. Surgery 111:386–93
Rüdiger Siewert J, Feith M, Werner M, Stein HJ (2000) Adenocarcinoma of the esophagogastric junction: results of surgical therapy based on anatomical/topographic classification in 1,002 consecutive patients. Ann Surg 232:353–61
Hosokawa Y, Kinoshita T, Konishi M, Takahashi S, Gotohda N, Kato Y et al (2012) Clinicopathological features and prognostic factors of adenocarcinoma of the esophagogastric junction according to Siewert classification: experiences at a single institution in Japan. Ann Surg Oncol 19:677–83. doi:10.1245/s10434-011-1983-x
Slim K, Blay JY, Brouquet A, Chatelain D, Comy M, Delpero JR et al (2009) Digestive oncology: surgical practices. J Chir (Paris) 146(Suppl 2):S11–80. doi:10.1016/S0021-7697(09)72398-1
Van Cutsem E, Van de Velde C, Roth A, Lordick F, Köhne C-H, Cascinu S et al (2008) Expert opinion on management of gastric and gastro-oesophageal junction adenocarcinoma on behalf of the European Organisation for Research and Treatment of Cancer (EORTC)-gastrointestinal cancer group. Eur J Cancer 44:182–94. doi:10.1016/j.ejca.2007.11.001
DeMeester SR (2006) Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment. Ann Surg Oncol 13:12–30. doi:10.1245/ASO.2005.12.025
Shrikhande SV, Shukla PJ, Qureshi S, Siddachari R, Upasani V, Ramadwar M et al (2006) D2 lymphadenectomy for gastric cancer in Tata Memorial Hospital: Indian data can now be incorporated in future international trials. Dig Surg 23:192–7. doi:10.1159/000094537
Japanese Gastric Cancer Association (1998) Japanese classification of gastric carcinoma—2nd English edition. Gastric Cancer 1:10–24. doi:10.1007/s101209800016
Yu W, Choi GS, Chung HY (2006) Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg 93:559–63. doi:10.1002/bjs.5353
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–8. doi:10.1016/j.surg.2007.05.005
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–13
Dikshit R, Gupta PC, Ramasundarahettige C, Gajalakshmi V, Aleksandrowicz L, Badwe R et al (2012) Cancer mortality in India: a nationally representative survey. Lancet 379:1807–16. doi:10.1016/S0140-6736(12)60358-4
Borch K, Jönsson B, Tarpila E, Franzén T, Berglund J, Kullman E et al (2000) Changing pattern of histological type, location, stage and outcome of surgical treatment of gastric carcinoma. Br J Surg 87:618–26. doi:10.1046/j.1365-2168.2000.01425.x
Blomjous JG, Hop WC, Langenhorst BL, ten Kate FJ, Eykenboom WM, Tilanus HW (1992) Adenocarcinoma of the gastric cardia. Recurrence and survival after resection. Cancer 70:569–74
de Manzoni G, Pedrazzani C, Pasini F, Durante E, Gabbani M, Grandinetti A et al (2003) Pattern of recurrence after surgery in adenocarcinoma of the gastro-oesophageal junction. Eur J Surg Oncol 29:506–10
Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K et al (1999) Adenocarcinoma of the gastroesophageal junction in Japan: relevance of Siewert’s classification applied to 177 cases resected at a single institution. J Am Coll Surg 189:594–601
Kaibara N, Nishimura O, Nishidoi H, Kimura O, Koga S (1987) Proximal gastrectomy as the surgical procedure of choice for upper gastric carcinoma. J Surg Oncol 36:110–2
Yoo CH, Sohn BH, Han WK, Pae WK (2004) Long-term results of proximal and total gastrectomy for adenocarcinoma of the upper third of the stomach. Cancer Res Treat 36:50–5. doi:10.4143/crt.2004.36.1.50
Harrison LE, Karpeh MS, Brennan MF (1998) Total gastrectomy is not necessary for proximal gastric cancer. Surgery 123:127–30
Buhl K, Schlag P, Herfarth C (1990) Quality of life and functional results following different types of resection for gastric carcinoma. Eur J Surg Oncol 16:404–9
Hsu CP, Chen CY, Hsieh YH, Hsia JY, Shai SE, Kao CH (1997) Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am J Gastroenterol 92:1347–50
Kobayashi T, Sugimura H, Kimura T (2002) Total gastrectomy is not always necessary for advanced gastric cancer of the cardia. Dig Surg 19:15–21
Okamura T, Tsujitani S, Korenaga D, Haraguchi M, Baba H, Hiramoto Y et al (1988) Lymphadenectomy for cure in patients with early gastric cancer and lymph node metastasis. Am J Surg 155:476–80
Kitamura K, Nishida S, Yamamoto K, Ichikawa D, Okamoto K, Taniguchi H et al (1998) Lymph node metastasis in gastric cancer in the upper third of the stomach—surgical treatment on the basis of the anatomical distribution of positive node. Hepatogastroenterology 45:281–5
Maruyama K, Gunvén P, Okabayashi K, Sasako M, Kinoshita T (1989) Lymph node metastases of gastric cancer. General pattern in 1931 patients. Ann Surg 210:596–602
Kitamura K, Yamaguchi T, Nishida S, Yamamoto K, Ichikawa D, Okamoto K et al (1997) The operative indications for proximal gastrectomy in patients with gastric cancer in the upper third of the stomach. Surg Today 27:993–8
Shimada H, Suzuki T, Nakajima K, Hori S, Hayashi H, Takeda A et al (1999) Lymph node metastasis with adenocarcinoma of the gastric cardia: clinicopathological analysis and indication for D1 dissection. Int Surg 84:13–7
Moreaux J, Msika S (1988) Carcinoma of the gastric cardia: surgical management and long-term survival. World J Surg 12:229–35
Goto H, Tokunaga M, Miki Y, Makuuchi R, Sugisawa N, Tanizawa Y et al (2014) The optimal extent of lymph node dissection for adenocarcinoma of the esophagogastric junction differs between Siewert type II and Siewert type III patients. Gastric Cancer. doi:10.1007/s10120-014-0364-0
An JY, Youn HG, Choi MG, Noh JH, Sohn TS, Kim S (2008) The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg 196:587–91. doi:10.1016/j.amjsurg.2007.09.040
Kondoh Y, Okamoto Y, Morita M, Nabeshima K, Nakamura K, Soeda J et al (2007) Clinical outcome of proximal gastrectomy in patients with early gastric cancer in the upper third of the stomach. Tokai J Exp Clin Med 32:48–53
Zhou Y, Pan J, Sheng Y, Liu H, Fan Z (2007) Surgical treatment effects in cancer of the cardia and esophagogastric junction. Chin Ger J Clin Oncol 6:P220–1. doi:10.1007/s10330-006-0040-x
Kim JH, Park SS, Kim J, Boo YJ, Kim SJ, Mok YJ et al (2006) Surgical outcomes for gastric cancer in the upper third of the stomach. World J Surg 30:1870–6. doi:10.1007/s00268-005-0703-8, discussion 1877–8
Shrikhande SV, Barreto SG, Talole SD, Vinchurkar K, Annaiah S, Suradkar K et al (2013) D2 lymphadenectomy is not only safe but necessary in the era of neoadjuvant chemotherapy. World J Surg Oncol 11:31. doi:10.1186/1477-7819-11-31
Shiraishi N, Adachi Y, Kitano S, Kakisako K, Inomata M, Yasuda K (2002) Clinical outcome of proximal versus total gastrectomy for proximal gastric cancer. World J Surg 26:1150–4. doi:10.1007/s00268-002-6369-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institution.
Informed consent
Informed consent was obtained from all individual participants included in the study
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(SAV 57 kb)
Rights and permissions
About this article
Cite this article
Sugoor, P., Shah, S., Dusane, R. et al. Proximal gastrectomy versus total gastrectomy for proximal third gastric cancer: total gastrectomy is not always necessary. Langenbecks Arch Surg 401, 687–697 (2016). https://doi.org/10.1007/s00423-016-1422-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1422-3