Abstract
Purpose
Despite progress in treatments, cancer pain remains underestimated, poorly assessed and under-treated. Prescribing strong opioids, because of their specificities, requires precision in management considering their pharmacology but also a clear understanding of recommendations. Some clinicians highlight the risk of addiction, excessive sedation and respiratory depression and their need for information. Our objective in this review is to suggest some clinical guidance for the positioning and daily use of opioids within cancer pain management.
Methods
Critical reflection based on literature analysis and clinical practice.
Results
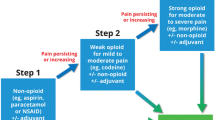
Strong opioids may be initiated as soon as pain diagnosis is defined. Factors to consider are pain aetiology, opioid pharmacokinetics and pharmacodynamics, genetic polymorphism, physiology (age, gender, weight and pregnancy), comorbidities (especially renal, hepatic, cardiovascular diseases), chronobiology, environmental factors, medication interference and treatment adherence. Achieving the best-balanced opioid treatment for background pain is complex, mainly due to the variable benefit/risk ratio between individuals and the experience of breakthrough cancer pain. Opioid initiation alongside a dynamic reassessment of pain should be fully integrated into the patient’s management to optimise analgesia. The efficacy and safety of a strong opioid treatment need to be re-evaluated and adapted to individuals constantly as it varies over time.
Conclusions
Cancer pain is multimorphic and permanently changing due to disease evolution, curative treatments and disruptive events (concomitant treatments, pain from associated disease, comorbidities and complications, modifications of the environment). Well-managed opioids are the cornerstone of a complex environment requiring multidisciplinary dynamic assessments integrated into the patient’s care pathway.



Similar content being viewed by others
References
MHJ VDB-VE, Hochstenbach LMJ, Joosten EAJ et al (2016) Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag 51:1070–1090.e9. https://doi.org/10.1016/j.jpainsymman.2015.12.340
MHJ VDB-VE, De Rijke JM, Kessels AG et al (2007) Review prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 18:1437–1449. https://doi.org/10.1093/annonc/mdm056
Breivik H, Cherny N, Collett B, de Conno F, Filbet M, Foubert AJ, Cohen R, Dow L (2009) Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol 20:1420–1433. https://doi.org/10.1093/annonc/mdp001
Valeberg BT, Rustøen T, Bjordal K, Hanestad BR, Paul S, Miaskowski C (2008) Self-reported prevalence, etiology, and characteristics of pain in oncology outpatients. Eur J Pain 12:582–590. https://doi.org/10.1016/j.ejpain.2007.09.004
Institut national du Cancer (INCA) (2012) Synthèse de l’enquête nationale 2010 sur la prise en charge de la douleur chez des patients adultes atteints de cancer. www.e-cancer.fr/content/download/63502/571325/file/ENQDOUL12.pdf. Accessed 17 July 2018
Vainio A, Auvinen A (1996) Prevalence of symptoms among patients with advanced cancer: an international collaborative study. J Pain Symptom Manag 12:3–10. https://doi.org/10.1016/0885-3924(96)00042-5
Greco MT, Roberto A, Corli O, Deandrea S, Bandieri E, Cavuto S, Apolone G (2014) Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol 32:4149–4154. https://doi.org/10.1200/JCO.2014.56.0383
Breuer B, Chang VT, Von Roenn JH et al (2015) How well do medical oncologists manage chronic cancer pain? A national survey. Oncologist 20:202–209. https://doi.org/10.1634/theoncologist.2014-0276
Mayor S (2000) Survey of patients shows that cancer pain still undertreated. BMJ 321:1309–1309. https://doi.org/10.1136/bmj.321.7272.1309/b
MacDonald N, Ayoub J, Farley J, Foucault C, Lesage P, Mayo N (2002) A Quebec survey of issues in cancer pain management. J Pain Symptom Manag 23:39–47. https://doi.org/10.1016/S0885-3924(01)00374-8
Hsieh RK (2005) Pain control in Taiwanese patients with cancer: a multicenter, patient-oriented survey. J Formos Med Assoc 104:913–919
Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330:592–596. https://doi.org/10.1056/NEJM199403033300902
Deandrea S, Montanari M, Moja L, Apolone G (2008) Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol Off J Eur Soc Med Oncol 19:1985–1991. https://doi.org/10.1093/annonc/mdn419
Efficace F, Bottomley A, Smit EF, Lianes P, Legrand C, Debruyne C, Schramel F, Smit H, Gaafar R, Biesma B, Manegold C, Coens C, Giaccone G, van Meerbeeck J, On behalf of the EORTC Lung Cancer Group and Quality of Life Unit (2006) Is a patient’s self-reported health-related quality of life a prognostic factor for survival in non-small-cell lung cancer patients? A multivariate analysis of prognostic factors of EORTC study 08975. Ann Oncol 17:1698–1704. https://doi.org/10.1093/annonc/mdl183
Armstrong AJ, Garrett-Mayer E, Ou Yang Y-C, Carducci MA, Tannock I, de Wit R, Eisenberger M (2007) Prostate-specific antigen and pain surrogacy analysis in metastatic hormone-refractory prostate cancer. J Clin Oncol 25:3965–3970. https://doi.org/10.1200/JCO.2007.11.4769
Halabi S, Vogelzang NJ, Kornblith AB, Ou SS, Kantoff PW, Dawson NA, Small EJ (2008) Pain predicts overall survival in men with metastatic castration-refractory prostate cancer. J Clin Oncol 26:2544–2549. https://doi.org/10.1200/JCO.2007.15.0367
Zylla D, Steele G, Gupta P (2017) A systematic review of the impact of pain on overall survival in patients with cancer. Support Care Cancer 25:1687–1698. https://doi.org/10.1007/s00520-017-3614-y
World Health Organization (1986) Cancer pain relief. World Health Organization Geneva
World Health Organization (ed) (1996) Cancer pain relief, 2nd edn. World Health Organization, Geneva
Zech DFJ, Grond S, Lynch J, Hertel D, Lehmann KA (1995) Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study. Pain 63:65–76. https://doi.org/10.1016/0304-3959(95)00017-M
Grond S, Zech D, Schug SA, Lynch J, Lehmann KA (1991) Validation of World Health Organization guidelines for cancer pain relief during the last days and hours of life. J Pain Symptom Manag 6:411–422. https://doi.org/10.1016/0885-3924(91)90039-7
Grond S, Radbruch L, Meuser T et al (1999) Assessment and treatment of neuropathic cancer pain following WHO guidelines. Pain 79:15–20. https://doi.org/10.1016/S0304-3959(98)00138-9
Hanks GW, Conno F, Cherny N, Hanna M, Kalso E, McQuay H, Mercadante S, Meynadier J, Poulain P, Ripamonti C, Radbruch L, Casas JR, Sawe J, Twycross RG, Ventafridda V, Expert Working Group of the Research Network of the European Association for Palliative Care (2001) Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer 84:587–593. https://doi.org/10.1054/bjoc.2001.1680
Ripamonti CI, Santini D, Maranzano E, Berti M, Roila F, on behalf of the ESMO Guidelines Working Group (2012) Management of cancer pain: ESMO clinical practice guidelines. Ann Oncol 23:vii139–vii154. https://doi.org/10.1093/annonc/mds233
National Institute for Health and Care Excellence (NICE) (2004) Guidance on cancer services. Improving supportive and palliative care for adults with cancer. The manual. https://www.nice.org.uk/guidance/csg4. Accessed 17 July 2018
Krakowski I, Vautrin CA, Collin E et al (2002) Summary version of the Standards, Options and Recommendations for the use of analgesia for the treatment of nociceptive pain in adults with cancer (update 2002). Br J Cancer 89 Suppl 1:S67–S72
Gunnarsdottir S, Sigurdardottir V, Kloke M, Radbruch L, Sabatowski R, Kaasa S, Klepstad P (2017) A multicenter study of attitudinal barriers to cancer pain management. Support Care Cancer 25:3595–3602. https://doi.org/10.1007/s00520-017-3791-8
McQuay H (1999) Opioids in pain management. Lancet 353:2229–2232. https://doi.org/10.1016/S0140-6736(99)03528-X
Peacock S, Patel S (2008) Cultural influences on pain. Rev Pain 1:6–9. https://doi.org/10.1177/204946370800100203
Bosch F, Baños JE (2002) Religious beliefs of patients and caregivers as a barrier to the pharmacologic control of cancer pain*. Clin Pharmacol Ther 72:107–111. https://doi.org/10.1067/mcp.2002.126180
Delorme T, Wood C, Bartaillard A, Pichard E, Dauchy S, Orbach D, Alibeu JP, Ricard C, Suc A, Boureau F, Roiusmans S, Patte R, Vullemin N, Torloting G, Larue F, Lassauniere JM, Collin E (2004) 2003 clinical practice guideline: Standards, Options and Recommendations for pain assessment in adult and children with cancer (summary report). Bull Cancer 91:419–430
National Cancer Institute (2015) Cancer Pain (PDQ®): Health Professional Version. https://www.cancer.gov/about-cancer/treatment/side-effects/pain/pain-hp-pdq. Accessed 17 July 2018
Kim HJ, Kim YS, Park SH (2015) Opioid rotation versus combination for cancer patients with chronic uncontrolled pain: a randomized study. BMC Palliat Care 14:41. https://doi.org/10.1186/s12904-015-0038-7
Greenlee H, DuPont-Reyes MJ, Balneaves LG et al (2017) Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin 67:194–232. https://doi.org/10.3322/caac.21397
Bandieri E, Romero M, Ripamonti CI, Artioli F, Sichetti D, Fanizza C, Santini D, Cavanna L, Melotti B, Conte PF, Roila F, Cascinu S, Bruera E, Tognoni G, Luppi M, the Early Strong Opioid Treatment Study Investigators (2016) Randomized trial of low-dose morphine versus weak opioids in moderate cancer pain. J Clin Oncol 34:436–442. https://doi.org/10.1200/JCO.2015.61.0733
Marinangeli F, Ciccozzi A, Leonardis M, Aloisio L, Mazzei A, Paladini A, Porzio G, Marchetti P, Varrassi G (2004) Use of strong opioids in advanced cancer pain: a randomized trial. J Pain Symptom Manag 27:409–416. https://doi.org/10.1016/J.JPAINSYMMAN.2003.10.006
Maltoni M, Scarpi E, Modonesi C, Passardi A, Calpona S, Turriziani A, Speranza R, Tassinari D, Magnani P, Saccani D, Montanari L, Roudnas B, Amadori D, Fabbri L, Nanni O, Raulli P, Poggi B, Fochessati F, Giannunzio D, Barbagallo ML, Minnotti V, Betti M, Giordani S, Piazza E, Scapaticci R, Ferrario S (2005) A validation study of the WHO analgesic ladder: a two-step vs three-step strategy. Support Care Cancer 13:888–894. https://doi.org/10.1007/s00520-005-0807-6
Cherny NI, Baselga J, De Conno F, Radbruch L (2010) Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in Europe: a report from the ESMO/EAPC Opioid Policy Initiative. Ann Oncol 21:615–626. https://doi.org/10.1093/annonc/mdp581
Ripamonti CI, Bareggi C (2009) Pharmacology of opioid analgesia: clinical principles. In: Bruera ED, Portenoy RK (eds) Cancer pain. Cambridge University Press, Cambridge, pp 195–229
Hvilke sykepleiefaglige vurderinger ligger til grunn for smertebehandlingen til pasienter med kreft i den palliative fasen? (2011) Diakonhjemmet hogskole
Hamunen K (2018) Vahvojen opioidien käyttö syövän aiheuttaman kivun hoidossa. http://www.kaypahoito.fi/web/kh/suositukset/suositus?id=nak07802. Accessed 9 Nov 2018
Bandieri E, Chiarolanza A, Luppi M, Magrini N, Marata AM, Ripamonti C (2009) Prescription of opioids in Italy: everything, but the morphine. Ann Oncol 20:961–962. https://doi.org/10.1093/annonc/mdp041
Smith HS (2009) Opioid metabolism. Mayo Clin Proc 84:613–624. https://doi.org/10.1016/S0025-6196(11)60750-7
Roulet L, Luthy C, Garin N et al (2011) Opioid rotation: from theory to practice. Interdisciplinary recommendations from the Geneva University Hospitals pain network. Rev Med Suisse 7:1400–1404 1406
Mercadante S (2015) Opioid metabolism and clinical aspects. Eur J Pharmacol 769:71–78. https://doi.org/10.1016/j.ejphar.2015.10.049
Yaksh Tony L., Wallace Mark S. (2011) Opioids, analgesia, and pain management | Goodman & Gilman’s: The pharmacological basis of therapeutics, 12e | AccessPharmacy | McGraw-Hill Medical. In: Goodman et Gilman (eds) The pharmacological basis of therapeutics, 12th edn. McGraw-Hill, New York, pp 481–525
Bennett D, Burton AW, Fishman S et al (2005) Consensus panel recommendations for the assessment and management of breakthrough pain: part 2 management. P T 30:354–361
Hoskin PJ, Hanks GW, Aherne GW, Chapman D, Littleton P, Filshie J (1989) The bioavailability and pharmacokinetics of morphine after intravenous, oral and buccal administration in healthy volunteers. Br J Clin Pharmacol 27:499–505
Gourlay GK, Cherry DA, Cousins MJ (1986) A comparative study of the efficacy and pharmacokinetics of oral methadone and morphine in the treatment of severe pain in patients with cancer. Pain 25:297–312
Kalso E, Vainio A (1990) Morphine and oxycodone hydrochloride in the management of cancer pain. Clin Pharmacol Ther 47:639–646
Lalovic B, Kharasch E, Hoffer C, Risler L, Liuchen L, Shen D (2006) Pharmacokinetics and pharmacodynamics of oral oxycodone in healthy human subjects: role of circulating active metabolites. Clin Pharmacol Ther 79:461–479. https://doi.org/10.1016/j.clpt.2006.01.009
Heiskanen T, Olkkola KT, Kalso E (1998) Effects of blocking CYP2D6 on the pharmacokinetics and pharmacodynamics of oxycodone*. Clin Pharmacol Ther 64:603–611. https://doi.org/10.1016/S0009-9236(98)90051-0
Leow KP, Smith MT, Williams B, Cramond T (1992) Single-dose and steady-state pharmacokinetics and pharmacodynamics of oxycodone in patients with cancer. Clin Pharmacol Ther 52:487–495
Pöyhiä R, Seppälä T, Olkkola KT, Kalso E (1992) The pharmacokinetics and metabolism of oxycodone after intramuscular and oral administration to healthy subjects. Br J Clin Pharmacol 33:617–621
Murray A, Hagen NA (2005) Hydromorphone. J Pain Symptom Manag 29:57–66. https://doi.org/10.1016/j.jpainsymman.2005.01.007
Thwaites D, McCann S, Broderick P (2004) Hydromorphone neuroexcitation. J Palliat Med 7:545–550. https://doi.org/10.1089/jpm.2004.7.545
Sarhill N, Walsh D, Nelson KA (2001) Hydromorphone: pharmacology and clinical applications in cancer patients. Support Care Cancer 9:84–96
Parab PV, Ritschel WA, Coyle DE et al (1988) Pharmacokinetics of hydromorphone after intravenous, peroral and rectal administration to human subjects. Biopharm Drug Dispos 9:187–199
Vallner JJ, Stewart JT, Kotzan JA et al (1981) Pharmacokinetics and bioavailability of hydromorphone following intravenous and oral administration to human subjects. J Clin Pharmacol 21:152–156
Panagiotou I, Mystakidou K (2010) Intranasal fentanyl: from pharmacokinetics and bioavailability to current treatment applications. Expert Rev Anticancer Ther 10:1009–1021. https://doi.org/10.1586/era.10.77
Sittl R, Likar R, Nautrup BP (2005) Equipotent doses of transdermal fentanyl and transdermal buprenorphine in patients with cancer and noncancer pain: results of a retrospective cohort study. Clin Ther 27:225–237. https://doi.org/10.1016/j.clinthera.2005.02.012
Streisand JB, Busch MA, Egan TD, Smith BG, Gay M, Pace NL (1998) Dose proportionality and pharmacokinetics of oral transmucosal fentanyl citrate. Anesthesiology 88:305–309
Prommer EE (2010) Methadone for cancer pain. Palliat Care Res Treat 4:PCRT.S4847. https://doi.org/10.4137/PCRT.S4847
Eap CB, Buclin T, Baumann P (2002) Interindividual variability of the clinical pharmacokinetics of methadone. Clin Pharmacokinet 41:1153–1193. https://doi.org/10.2165/00003088-200241140-00003
Bourquin V, Petignat P-A, Besson M, Piguet V (2008) Analgesia and renal insufficiency. Rev Med Suisse 4:2218–2220 2222–3
Kress HG (2009) Clinical update on the pharmacology, efficacy and safety of transdermal buprenorphine. Eur J Pain 13:219–230. https://doi.org/10.1016/j.ejpain.2008.04.011
Sittl R (2006) Transdermal buprenorphine in cancer pain and palliative care. Palliat Med 20(Suppl 1):s25–s30
Davis MP (2005) Buprenorphine in cancer pain. Support Care Cancer 13:878–887. https://doi.org/10.1007/s00520-005-0849-9
Cone EJ, Gorodetzky CW, Yousefnejad D et al The metabolism and excretion of buprenorphine in humans. Drug Metab Dispos 12:577–581
Cote J, Montgomery L (2014) Sublingual buprenorphine as an analgesic in chronic pain: a systematic review. Pain Med 15:1171–1178. https://doi.org/10.1111/pme.12386
Lötsch J, Doehring A, Mogil JS, Arndt T, Geisslinger G, Ultsch A (2013) Functional genomics of pain in analgesic drug development and therapy. Pharmacol Ther 139:60–70. https://doi.org/10.1016/j.pharmthera.2013.04.004
Naalsund Andreassen T, Klepstad P, Davies A et al (2011) Influences on the pharmacokinetics of oxycodone: a multicentre cross-sectional study in 439 adult cancer patients. J Clin Pharmacol 67:493–506. https://doi.org/10.1007/s00228-010-0948-5
Huang P, Chen C, Mague SD et al A common single nucleotide polymorphism A118g of the Mu opioid receptor alters its N-glycosylation and protein stability. Biochem J 441:379–386. https://doi.org/10.1042/BJ20111050
Bond C, LaForge KS, Tian M et al (1998) Single-nucleotide polymorphism in the human mu opioid receptor gene alters beta-endorphin binding and activity: possible implications for opiate addiction. Proc Natl Acad Sci U S A 95:9608–9613
Mura E, Govoni S, Racchi M et al (2013) Consequences of the 118A>G polymorphism in the OPRMI gene: translation from bench to bedside? J Pain Res 6:331–353. https://doi.org/10.2147/JPR.S42040
Riley J, Branford R, Droney J, Gretton S, Sato H, Kennett A, Oyebode C, Thick M, Wells A, Williams J, Welsh K, Ross J (2015) Morphine or oxycodone for cancer-related pain? A randomized, open-label, controlled trial. J Pain Symptom Manag 49:161–172. https://doi.org/10.1016/J.JPAINSYMMAN.2014.05.021
Cazaban-Mazerolles J (2005) Oxycodone et douleur cancéreuse. Med Palliat 4:53–57. https://doi.org/10.1016/S1636-6522(05)81561-2
King SJ, Reid C, Forbes K, Hanks G (2011) A systematic review of oxycodone in the management of cancer pain. Palliat Med 25:454–470. https://doi.org/10.1177/0269216311401948
Bruera E, Paice JA (2015) Cancer pain management: safe and effective use of opioids. Am Soc Clin Oncol Educ B 35:e593–e599. https://doi.org/10.14694/EdBook_AM.2015.35.e593
Reddy A, De M, Cruz LA, et al Symptom management and supportive care patterns of storage, use, and disposal of opioids among cancer outpatients. https://doi.org/10.1634/theoncologist.2014-0071, 2014
Droney J, Riley J, Ross J (2012) Opioid genetics in the context of opioid switching. Curr Opin Support Palliat Care 6:10–16. https://doi.org/10.1097/SPC.0b013e32834f6a07
Söderberg Löfdal KC, Andersson ML, Gustafsson LL (2013) Cytochrome P450-mediated changes in oxycodone pharmacokinetics/pharmacodynamics and their clinical implications. Drugs 73:533–543. https://doi.org/10.1007/s40265-013-0036-0
Innaurato G, Piguet V, Simonet ML (2015) [Analgesia in patients with hepatic impairment) Rev Med Suisse 11(1380):1382–1384
King S, Forbes K, Hanks G, Ferro CJ, Chambers EJ (2011) A systematic review of the use of opioid medication for those with moderate to severe cancer pain and renal impairment: a European Palliative Care Research Collaborative opioid guidelines project. Palliat Med 25:525–552. https://doi.org/10.1177/0269216311406313
Sande TA, Laird BJA, Fallon MT (2017) The use of opioids in cancer patients with renal impairment—a systematic review. Support Care Cancer 25:661–675. https://doi.org/10.1007/s00520-016-3447-0
Mallappallil M, Sabu J, Friedman EA, Salifu M (2017) What do we know about opioids and the kidney? Int J Mol Sci 18:223
Ingrasciotta Y, Sultana J, Giorgianni F, Caputi AP, Arcoraci V, Tari DU, Linguiti C, Perrotta M, Nucita A, Pellegrini F, Fontana A, Cavagna L, Santoro D, Trifirò G (2014) The burden of nephrotoxic drug prescriptions in patients with chronic kidney disease: a retrospective population-based study in southern Italy. PLoS One 9:e89072. https://doi.org/10.1371/journal.pone.0089072
Murtagh FEM, Chai M-O, Donohoe P, Edmonds PM, Higginson IJ (2007) The use of opioid analgesia in end-stage renal disease patients managed without dialysis: recommendations for practice. J Pain Palliat Care Pharmacother 21:5–16
Aronoff G, Bennet W, Burns J, et al (2007) Drug prescribing in renal failure : dosing guidelines for adults and children. Philladelphia Am Coll Physician 272
Böger RH (2006) Renal impairment: a challenge for opioid treatment? The role of buprenorphine. Palliat Med 20(Suppl 1):s17–s23
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Pergolizzi J, Böger RH, Budd K, Dahan A, Erdine S, Hans G, Kress HG, Langford R, Likar R, Raffa RB, Sacerdote P (2008) Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract 8:287–313. https://doi.org/10.1111/j.1533-2500.2008.00204.x
Hui D, Bruera E (2014) A personalized approach to assessing and managing pain in patients with cancer. J Clin Oncol 32:1640–1646. https://doi.org/10.1200/JCO.2013.52.2508
Portenoy RK, Hagen NA (1990) Breakthrough pain: definition, prevalence and characteristics. Pain. 41:273–281. https://doi.org/10.1016/0304-3959(90)90004-W
Mercadante S, Portenoy RK (2016) Breakthrough cancer pain. Pain 157:2657–2663. https://doi.org/10.1097/j.pain.0000000000000721
Greco MT, Corli O, Montanari M, Deandrea S, Zagonel V, Apolone G (2011) Epidemiology and pattern of care of breakthrough cancer pain in a longitudinal sample of cancer patients. Clin J Pain 27:9–18. https://doi.org/10.1097/AJP.0b013e3181edc250
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G, Science Committee of the Association for Palliative Medicine of Great Britain and Ireland (2009) The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain 13:331–338. https://doi.org/10.1016/j.ejpain.2008.06.014
Mercadante S, Radbruch L, Caraceni A, Cherny N, Kaasa S, Nauck F, Ripamonti C, de Conno F, Steering Committee of the European Association for Palliative Care (EAPC) Research Network (2002) Episodic (breakthrough) pain: consensus conference of an expert working group of the European Association for Palliative Care. Cancer 94:832–839
Davies AN, Dickman A, Farquhar-Smith P, Webber K, Zeppetella J (2016) Incorrect use of the English language term “episodic”. J Pain Symptom Manag 52:e1. https://doi.org/10.1016/j.jpainsymman.2016.06.002
Portenoy R, Koh M (2010) Cancer pain syndromes. In: Bruera E, Portenoy RK (eds) Cancer pain: assessment and management, 4th edn. Cambridge University Press, Cambridge, pp 53–88
Caraceni A, Davies A, Poulain P, Cortés-Funes H, Panchal SJ, Fanelli G (2013) Guidelines for the management of breakthrough pain in patients with cancer. J Natl Compr Cancer Netw 11(Suppl 1):S29–S36
Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W, Slama O, Korhonen T, Filbet M, Poulain P, Mystakidou K, Ardavanis A, O’Brien T, Wilkinson P, Caraceni A, Zucco F, Zuurmond W, Andersen S, Damkier A, Vejlgaard T, Nauck F, Radbruch L, Sjolund KF, Stenberg M (2013) Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain Symptom Manag 46:619–628. https://doi.org/10.1016/j.jpainsymman.2012.12.009
HAS (2014) Les médicaments des accès douloureux paroxystiques du cancer. http://www.has-sante.fr/portail/jcms/c_952643/les-medicaments-des-acces-douloureux-paroxystique
Zeppetella G, O’Doherty CA, Collins S (2000) Prevalence and characteristics of breakthrough pain in cancer patients admitted to a hospice. J Pain Symptom Manag 20:87–92
Poulain P, Filbet M, Ammar D, Morere JF, Krakowski I, Delorme C, Serrie A (2012) Caractéristiques et traitements des accès douloureux paroxystiques (ADPc) chez les patients cancéreux : résultats de l’enquête ADEPI. Douleurs Eval - Diagnostic - Trait 13:163–168. https://doi.org/10.1016/j.douler.2012.07.002
Pautex S, Vogt-Ferrier N, Zulian GB (2014) Breakthrough pain in elderly patients with cancer: treatment options. Drugs Aging 31:405–411. https://doi.org/10.1007/s40266-014-0181-5
Daviesl A, Zeppetellal G, Andersenl S, Damkierl A, Vejlgaardl T, Nauckl F, Radbruchl L, Sjolundl KF, Stenbergl M, Buchananl A (2011) Multi-centre European study of breakthrough cancer pain: pain characteristics and patient perceptions of current and potential management strategies. Eur J Pain 15:756–763. https://doi.org/10.1016/j.ejpain.2010.12.004
Hagen NA, Fisher K, Victorino C, Farrar JT (2007) A titration strategy is needed to manage breakthrough cancer pain effectively: observations from data pooled from three clinical trials. J Palliat Med 10:47–55. https://doi.org/10.1089/jpm.2006.0151
Bedard G, Davies A, McDonald R, Hawley P, Buchanan A, Popovic M, Wong E, Chow E (2015) Breakthrough cancer pain: a comparison of surveys with European and Canadian patients. Support Care Cancer 23:791–796. https://doi.org/10.1007/s00520-014-2426-6
Nelson AD, Camilleri M (2016) Opioid-induced constipation: advances and clinical guidance. Ther Adv Chronic Dis 7:121–134. https://doi.org/10.1177/2040622315627801
DePriest AZ, Miller K (2014) Oxycodone/naloxone: role in chronic pain management, opioid-induced constipation, and abuse deterrence. Pain Ther 3:1–15. https://doi.org/10.1007/s40122-014-0026-2
Porter J, Jick H (1980) Addiction rare in patients treated with narcotics. N Engl J Med 302:123–123. https://doi.org/10.1056/NEJM198001103020221
Veevaete L, Lavand′homme P (2014) Opioid-induced hyperalgesia: new insights into the chronicization of pain. Tech Reg Anesth Pain Manag 18:100–104. https://doi.org/10.1053/j.trap.2015.10.004
Joly V, Richebe P, Guignard B, Fletcher D, Maurette P, Sessler DI, Chauvin M (2005) Remifentanil-induced postoperative hyperalgesia and its prevention with small-dose ketamine. Anesthesiology 103:147–155
Samuelsen P-J, Nielsen CS, Wilsgaard T, Stubhaug A, Svendsen K, Eggen AE (2017) Pain sensitivity and analgesic use among 10,486 adults: the Tromsø study. BMC Pharmacol Toxicol 18(45):45. https://doi.org/10.1186/s40360-017-0149-2
Bruera E, Franco JJ, Maltoni M, Watanabe S, Suarez-Almazor M (1995) Changing pattern of agitated impaired mental status in patients with advanced cancer: association with cognitive monitoring, hydration, and opioid rotation. J Pain Symptom Manag 10:287–291. https://doi.org/10.1016/0885-3924(95)00005-J
Dale O, Moksnes K, Kaasa S (2011) European Palliative Care Research Collaborative pain guidelines: opioid switching to improve analgesia or reduce side effects. A systematic review. Palliat Med 25:494–503. https://doi.org/10.1177/0269216310384902
Mercadante S, Valle A, Porzio G, Fusco F, Aielli F, Adile C, Casuccio A, Home Care—Italy Group (2013) Opioid switching in patients with advanced cancer followed at home. A retrospective analysis. J Pain Symptom Manag 45:298–304. https://doi.org/10.1016/j.jpainsymman.2012.02.025
Røttingen J-A, Kongsgaard U, Kaasa S, et al Palliative treatment of cancer-related pain Title Palliative treatment of cancer-related pain Norwegian title Lindring av smerter hos kreftpasienter Institution Norwegian Knowledge Centre for the Health Services https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2009-og-eldre/rapport_0509_palliativ_nettversjon.pdf. Accessed 17 July 2018
Takagi Y, Aruga E (2018) New opioid options in Japan - methadone, tapentadol and hydromorphone. Gan To Kagaku Ryoho 45:205–211
Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL (2009) Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manag 38:409–417. https://doi.org/10.1016/j.jpainsymman.2009.06.004
Deer TR, Gunn J Blood testing in chronic pain management. Pain Physician 18:E157–E161
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpää M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice ASC, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M (2015) Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14:162–173. https://doi.org/10.1016/S1474-4422(14)70251-0
Beaulieu P, I Lussier D (2010) Toward a rational taxonomy of analgesic treatments. In: Beaulieu P, Lussier D, Porreca F, Dickenson AH (eds) Pharmacology of pain. IASP Press, Seattle, pp 27–40
Hoskin P (2006) Cancer pain: treatment overview. In: Wall and Melzack’s textbook of pain, 5th ed. Elsevier Churchill Livingstone, pp 1141–57
Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S (2001) Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain 93:247–257
Wilson J, Stack C, Hester J (2014) Recent advances in cancer pain management. F1000Prime Rep 6:10. https://doi.org/10.12703/P6-10
Hochberg U, Elgueta MF, Perez J (2017) Interventional analgesic management of lung cancer pain. Front Oncol 7:17. https://doi.org/10.3389/fonc.2017.00017
Chwistek M (2017) Recent advances in understanding and managing cancer pain. F1000Research 6:945. https://doi.org/10.12688/f1000research.10817.1
Swarm R, Karanikolos M, Cousins M (2010) (No Title) Injections, neural blockade and implant therapies for pain control. In: Oxford University Press O (ed) Hanks G, Cherny NI, Christaskis NA, et al. (eds) Oxford textbook of palliative medicine, 4th edn. pp 734–755
Miguel R (2000) Interventional treatment of cancer pain: the fourth step in the World Health Organization analgesic ladder? Cancer Control 7:149–156. https://doi.org/10.1177/107327480000700205
Buga S, Sarria JE (2012) The management of pain in metastatic bone disease. Cancer Control 19:154–166. https://doi.org/10.1177/107327481201900210
Mathiesen O, Dahl B, Thomsen BA, Kitter B, Sonne N, Dahl JB, Kehlet H (2013) A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 22:2089–2096. https://doi.org/10.1007/s00586-013-2826-1
AFSSAPS (2010) Recommandations de bonne pratique douleur rebelle en situation palliative avancée chez l’adulte. Modalites d’utilisation, notamment hors-AMM, de certains médicaments : anesthésiques locaux par voie périmédullaire, parentérale et topique ; fentanyl, sufentanil ; kétamine ; MEOPA ; méthadone ; midazolam ; morphine par voie périmédullaire et intracérébroventriculaire ; propofol. AFSSAPS, Paris. http://ansm.sante.fr/var/ansm_site/storage/original/application/0f8ed3dd2a116934a6fe38cf56367eb8.pdf. Accessed 17 July 2018
Ciechanowicz SJ, Ma D (2016) Anaesthesia for oncological surgery - can it really influence cancer recurrence? Anaesthesia 71:127–131. https://doi.org/10.1111/anae.13342
Langley RR, Fidler IJ (2007) Tumor cell-organ microenvironment interactions in the pathogenesis of cancer metastasis. Endocr Rev 28:297–321. https://doi.org/10.1210/er.2006-0027
Rudd RA, Seth P, David F, Scholl L (2016) Increases in drug and opioid-involved overdose deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 65:1445–1452. https://doi.org/10.15585/mmwr.mm655051e1
Starr TD, Rogak LJ, Passik SD (2010) Substance abuse in cancer pain. Curr Pain Headache Rep 14:268–275. https://doi.org/10.1007/s11916-010-0118-6
Fallon M, Cherny N (2015) Opioid therapy: optimizing analgesic outcomes. In: Cherny N, Fallon M, Kaasa S, et al (eds) Oxford textbook of palliative medicine. Oxford University Press, pp 521–59
Webster LR, Webster RM (2005) Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med 6:432–442. https://doi.org/10.1111/j.1526-4637.2005.00072.x
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI, ESMO Guidelines Committee (2018) Management of cancer pain in adult patients: ESMO clinical practice guidelines†. Ann Oncol 29:iv166–iv191. https://doi.org/10.1093/annonc/mdy152
Kasasbeh MAM, McCabe C, Payne S (2017) Cancer-related pain management: a review of knowledge and attitudes of healthcare professionals. Eur J Cancer Care (Engl) 26:e12625. https://doi.org/10.1111/ecc.12625
Chow R, Saunders K, Burke H, Belanger A, Chow E (2017) Needs assessment of primary care physicians in the management of chronic pain in cancer survivors. Support Care Cancer 25:3505–3514. https://doi.org/10.1007/s00520-017-3774-9
Kasasbeh MAM, McCabe C, Payne S (2017) Action learning: an effective way to improve cancer-related pain management. J Clin Nurs 26:3430–3441. https://doi.org/10.1111/jocn.13709
Acknowledgements
Support was provided by Xavier Amores, M.D.; Viorica Braniste, M.D. & Ph.D. (Kyowa Kirin); Robert Campos Oriola, Ph.D and Marie-Odile Barbaza, MD, (Auxesia) for manuscript preparation.
Funding
This article was funded by Kyowa Kirin.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Brigitte George reports non-financial support from Kyowa Kirin, during the conduct of the submitted work; personal fees and non-financial support from Mundipharma, non-financial support from Grunenthal and Kyowa Kirin, outside the submitted work; participation to a clinical study without honoraria from Bouchara. Christian Minello reports non-financial support from Kyowa Kirin, during the conduct of the submitted work; personal fees and non-financial support from Takeda, and non-financial support from Kyowa Kirin, Mundi Pharma, Mylan Pharma and Grunenthal, outside the submitted work. Gilles Allano reports non-financial support from Kyowa Kirin, during the conduct of the submitted work; personal fees and non-financial support from Grunenthal, Mundipharma and Medtronic, and non-financial support from Kyowa Kirin, outside the submitted work. Caroline Maindet reports non-financial support from Kyowa Kirin, during the conduct of the submitted work; personal fees and non-financial support from Mundipharma, and non-financial support from Kyowa Kirin, Grunenthal, Hospira, Takeda, and Janssen Cilag, outside the submitted work. Alexis Burnod reports non-financial support from Kyowa Kirin, during the conduct of the submitted work; non-financial support from Kyowa Kirin, outside the submitted work. Antoine Lemaire reports non-financial support from Kyowa Kirin France, during the conduct of the submitted work; personal fees and non-financial support from Kyowa Kirin International, Mundi Pharma, Grunenthal and Takeda, personal fees from Mylan, and non-financial support from Kyowa Kirin France, Archimèdes Pharma, Teva, Prostrakan, outside the submitted work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
George, B., Minello, C., Allano, G. et al. Opioids in cancer-related pain: current situation and outlook. Support Care Cancer 27, 3105–3118 (2019). https://doi.org/10.1007/s00520-019-04828-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04828-8