Abstract
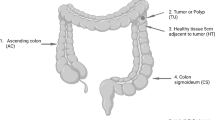
Microbiota refers to a colony of microorganisms, and they are found in all multicellular organisms. This colony plays a major role in both the physiology and disease of the organism it inhabits. Much attention has been paid to host–microbiota interactions, but there has been little investigation on its role in carcinogenesis. In this study, we characterized a fecal mycobiota, also known as fungal signature, for the first time with 131 subjects, comprising polyp and colorectal cancer (CRC) patients, as well as a healthy control population. The data obtained were analyzed to assess the biodiversity and composition of the fungi. The impacts of anatomic position and tumor stage on the mycobiota were also evaluated. Correlations between fungi were investigated using the Spearman test. We observed fungal dysbiosis in colon polyps and CRC, including decreased diversity in polyp patients, an increased Ascomycota/Basidiomycota ratio, and an increased proportion of opportunistic fungi Trichosporon and Malassezia, which might favor the progression of CRC. Subsequent analysis with regard to tumor stage demonstrated a lower diversity and significant mycobiota alteration in early-stage tumors. Finally, the fungal correlation showed a close relationship within the community and concomitantly revealed a dramatically structured discrepancy in each clinical phenotype. In conclusion, our study has uncovered a distinct fungal dysbiosis and an alteration in the fungal network, which could play important roles in polyp and CRC pathogenesis.




Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2017) Cancer Statistics, 2017. CA Cancer J Clin 67(1):7–30
Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, Starling N (2010) Colorectal cancer. Lancet 375(9719):1030–1047
Collins D, Hogan AM, Winter DC (2011) Microbial and viral pathogens in colorectal cancer. Lancet Oncol 12(5):504–512
Kamada N, Chen GY, Inohara N, Núñez G (2013) Control of pathogens and pathobionts by the gut microbiota. Nat Immunol 14(7):685–690
Rooks MG, Garrett WS (2016) Gut microbiota, metabolites and host immunity. Nat Rev Immunol 16(6):341–352
Round JL, Mazmanian SK (2009) The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol 9(5):313–323
Ohtani N, Yoshimoto S, Hara E (2014) Obesity and cancer: a gut microbial connection. Cancer Res 74(7):1885–1889
Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, Nielsen J, Bäckhed F (2013) Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498(7452):99–103
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490(7418):55–60
Tang WH, Kitai T, Hazen SL (2017) Gut microbiota in cardiovascular health and disease. Circ Res 120(7):1183–1196
Strati F, Cavalieri D, Albanese D, De Felice C, Donati C, Hayek J, Jousson O, Leoncini S, Renzi D, Calabrò A, De Filippo C (2017) New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome 5(1):24
Tian H, Ge X, Nie Y, Yang L, Ding C, McFarland LV, Zhang X, Chen Q, Gong J, Li N (2017) Fecal microbiota transplantation in patients with slow-transit constipation: a randomized, clinical trial. PLoS One 12(2):e0171308
Qin N, Yang F, Li A, Prifti E, Chen Y, Shao L, Guo J, Le Chatelier E, Yao J, Wu L, Zhou J, Ni S, Liu L, Pons N, Batto JM, Kennedy SP, Leonard P, Yuan C, Ding W, Chen Y, Hu X, Zheng B, Qian G, Xu W, Ehrlich SD, Zheng S, Li L (2014) Alterations of the human gut microbiome in liver cirrhosis. Nature 513(7516):59–64
Imhann F, Vich Vila A, Bonder MJ, Fu J, Gevers D, Visschedijk MC, Spekhorst LM, Alberts R, Franke L, van Dullemen HM, Ter Steege RW, Huttenhower C, Dijkstra G, Xavier RJ, Festen EA, Wijmenga C, Zhernakova A, Weersma RK (2016) Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut. doi:10.1136/gutjnl-2016-312135
Plottel CS, Blaser MJ (2011) Microbiome and malignancy. Cell Host Microbe 10(4):324–335
Shanahan F (2013) The colonic microbiota in health and disease. Curr Opin Gastroenterol 29(1):49–54
Feng Q, Liang S, Jia H, Stadlmayr A, Tang L, Lan Z, Zhang D, Xia H, Xu X, Jie Z, Su L, Li X, Li X, Li J, Xiao L, Huber-Schönauer U, Niederseer D, Xu X, Al-Aama JY, Yang H, Wang J, Kristiansen K, Arumugam M, Tilg H, Datz C, Wang J (2015) Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun 6:6528
Flemer B, Lynch DB, Brown JM, Jeffery IB, Ryan FJ, Claesson MJ, O’Riordain M, Shanahan F, O’Toole PW (2017) Tumour-associated and non-tumour-associated microbiota in colorectal cancer. Gut 66:633–643. doi:10.1136/gutjnl-2015-309595
Tsoi H, Chu ESH, Zhang X, Sheng J, Nakatsu G, Ng SC, Chan AWH, Chan FKL, Sung JJY, Yu J (2017) Peptostreptococcus anaerobius induces intracellular cholesterol biosynthesis in colon cells to induce proliferation and causes dysplasia in mice. Gastroenterology 152:1419–1433.e5
Gao R, Gao Z, Huang L, Qin H (2017) Gut microbiota and colorectal cancer. Eur J Clin Microbiol Infect Dis 36(5):757–769
Gao R, Kong C, Huang L, Li H, Qu X, Liu Z, Lan P, Wang J, Qin H (2017) Mucosa-associated microbiota signature in colorectal cancer. Eur J Clin Microbiol Infect Dis. doi:10.1007/s10096-017-3026-4
Kostic AD, Gevers D, Pedamallu CS, Michaud M, Duke F, Earl AM, Ojesina AI, Jung J, Bass AJ, Tabernero J, Baselga J, Liu C, Shivdasani RA, Ogino S, Birren BW, Huttenhower C, Garrett WS, Meyerson M (2012) Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res 22(2):292–298
Abed J, Emgård JE, Zamir G, Faroja M, Almogy G, Grenov A, Sol A, Naor R, Pikarsky E, Atlan KA, Mellul A, Chaushu S, Manson AL, Earl AM, Ou N, Brennan CA, Garrett WS, Bachrach G (2016) Fap2 mediates Fusobacterium nucleatum colorectal adenocarcinoma enrichment by binding to tumor-expressed Gal-GalNAc. Cell Host Microbe 20(2):215–225
Kostic AD, Chun E, Robertson L, Glickman JN, Gallini CA, Michaud M, Clancy TE, Chung DC, Lochhead P, Hold GL, El-Omar EM, Brenner D, Fuchs CS, Meyerson M, Garrett WS (2013) Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe 14(2):207–215
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW (2013) Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/beta-catenin signaling via its FadA adhesin. Cell Host Microbe 14(2):195–206
Gouba N, Drancourt M (2015) Digestive tract mycobiota: a source of infection. Med Mal Infect 45(1–2):9–16
Sokol H, Leducq V, Aschard H, Pham HP, Jegou S, Landman C, Cohen D, Liguori G, Bourrier A, Nion-Larmurier I, Cosnes J, Seksik P, Langella P, Skurnik D, Richard ML, Beaugerie L (2017) Fungal microbiota dysbiosis in IBD. Gut 66:1039–1048
Monteiro-da-Silva F, Sampaio-Maia B, Pereira Mde L, Araujo R (2013) Characterization of the oral fungal microbiota in smokers and non-smokers. Eur J Oral Sci 121(2):132–135
Mukherjee PK, Chandra J, Retuerto M, Sikaroodi M, Brown RE, Jurevic R, Salata RA, Lederman MM, Gillevet PM, Ghannoum MA (2014) Oral mycobiome analysis of HIV-infected patients: identification of Pichia as an antagonist of opportunistic fungi. PLoS Pathog 10(3):e1003996
Krause R, Moissl-Eichinger C, Halwachs B, Gorkiewicz G, Berg G, Valentin T, Prattes J, Högenauer C, Zollner-Schwetz I (2017) Mycobiome in the lower respiratory tract—a clinical perspective. Front Microbiol 7:2169
Alonso R, Pisa D, Aguado B, Carrasco L (2017) Identification of fungal species in brain tissue from Alzheimer’s disease by next-generation sequencing. J Alzheimers Dis 58(1):55–67
Luan C, Xie L, Yang X, Miao H, Lv N, Zhang R, Xiao X, Hu Y, Liu Y, Wu N, Zhu Y, Zhu B (2015) Dysbiosis of fungal microbiota in the intestinal mucosa of patients with colorectal adenomas. Sci Rep 5:7980
Schoch CL, Seifert KA, Huhndorf S, Robert V, Spouge JL, Levesque CA, Chen W; Fungal Barcoding Consortium; Fungal Barcoding Consortium Author List (2012) Nuclear ribosomal internal transcribed spacer (ITS) region as a universal DNA barcode marker for Fungi. Proc Natl Acad Sci U S A 109(16):6241–6246
Liu W, Zhang J, Wu C, Cai S, Huang W, Chen J, Xi X, Liang Z, Hou Q, Zhou B, Qin N, Zhang H (2016) Unique features of ethnic Mongolian gut microbiome revealed by metagenomic analysis. Sci Rep 6:34826
Masella AP, Bartram AK, Truszkowski JM, Brown DG, Neufeld JD (2012) PANDAseq: paired-end assembler for illumina sequences. BMC Bioinformatics 13:31
Edgar RC (2010) Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26(19):2460–2461
Cole JR, Wang Q, Fish JA, Chai B, McGarrell DM, Sun Y, Brown CT, Porras-Alfaro A, Kuske CR, Tiedje JM (2014) Ribosomal Database Project: data and tools for high throughput rRNA analysis. Nucleic Acids Res 42(Database issue):D633–D642
Lozupone C, Lladser ME, Knights D, Stombaugh J, Knight R (2011) UniFrac: an effective distance metric for microbial community comparison. ISME J 5(2):169–172
Kim YH, Min BH, Kim SJ, Choi HK, Kim KM, Chun HK, Lee H, Kim JY, Chang DK, Son HJ, Rhee PL, Rhee JC, Kim JJ (2010) Difference between proximal and distal microsatellite-unstable sporadic colorectal cancers: analysis of clinicopathological and molecular features and prognoses. Ann Surg Oncol 17(5):1435–1441
Strati F, Di Paola M, Stefanini I, Albanese D, Rizzetto L, Lionetti P, Calabrò A, Jousson O, Donati C, Cavalieri D, De Filippo C (2016) Age and gender affect the composition of fungal population of the human gastrointestinal tract. Front Microbiol 7:1227
Ott SJ, Kühbacher T, Musfeldt M, Rosenstiel P, Hellmig S, Rehman A, Drews O, Weichert W, Timmis KN, Schreiber S (2008) Fungi and inflammatory bowel diseases: alterations of composition and diversity. Scand J Gastroenterol 43(7):831–841
Mukherjee PK, Sendid B, Hoarau G, Colombel JF, Poulain D, Ghannoum MA (2015) Mycobiota in gastrointestinal diseases. Nat Rev Gastroenterol Hepatol 12(2):77–87
Hong G, Miller HB, Allgood S, Lee R, Lechtzin N, Zhang SX (2017) Use of selective fungal culture media increases rates of detection of fungi in the respiratory tract of cystic fibrosis patients. J Clin Microbiol 55(4):1122–1130
de Almeida Júnior JN, Hennequin C (2016) Invasive trichosporon infection: a systematic review on a re-emerging fungal pathogen. Front Microbiol 7:1629
Montoya AM, González GM, Martinez-Castilla AM, Aguilar SA, Franco-Molina MA, Coronado-Cerda E, Rosas-Taraco AG (2017) Cytokines profile in immunocompetent mice during Trichosporon asahii infection. Med Mycol. doi:10.1093/mmy/myx018
Kushima H, Tokimatsu I, Ishii H, Kawano R, Watanabe K, Kadota JI (2017) A new amino acid substitution at G150S in lanosterol 14-alpha demethylase (Erg11 protein) in multi-azole-resistant Trichosporon asahii. Med Mycol J 58(1):E23–E28
Angiolella L, Leone C, Rojas F, Mussin J, de Los Angeles Sosa M, Giusiano G (2017) Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur. Med Mycol. doi:10.1093/mmy/myx014
Yu YN, Yu TC, Zhao HJ, Sun TT, Chen HM, Chen HY, An HF, Weng YR, Yu J, Li M, Qin WX, Ma X, Shen N, Hong J, Fang JY (2015) Berberine may rescue Fusobacterium nucleatum-induced colorectal tumorigenesis by modulating the tumor microenvironment. Oncotarget 6(31):32013–32026
Zhang X, Zhao Y, Xu J, Xue Z, Zhang M, Pang X, Zhang X, Zhao L (2015) Modulation of gut microbiota by berberine and metformin during the treatment of high-fat diet-induced obesity in rats. Sci Rep 5:14405
Cong L, Liao Y, Yang S, Yang R (2017) In vitro activity of berberine alone and in combination with antifungal drugs against planktonic forms and biofilms of Trichosporon asahii. Mycopathologia. doi:10.1007/s11046-017-0119-7
Pande A, Non LR, Romee R, Santos CA (2017) Pseudozyma and other non-Candida opportunistic yeast bloodstream infections in a large stem cell transplant center. Transpl Infect Dis 19(2)
Ilahi A, Hadrich I, Goudjil S, Kongolo G, Chazal C, Léké A, Ayadi A, Chouaki T, Ranque S (2017) Molecular epidemiology of a Malassezia pachydermatis neonatal unit outbreak. Med Mycol. doi:10.1093/mmy/myx022
Prohić A, Jovović Sadiković T, Kuskunović-Vlahovljak S, Baljić R (2016) Distribution of Malassezia species in patients with different dermatological disorders and healthy individuals. Acta Dermatovenerol Croat 24(4):274–281
Cheikhrouhou F, Guidara R, Masmoudi A, Trabelsi H, Neji S, Sellami H, Makni F, Ayadi A (2017) Molecular identification of Malassezia species in patients with Malassezia folliculitis in Sfax, Tunisia. Mycopathologia 182:583–589
Celis AM, Vos AM, Triana S, Medina CA, Escobar N, Restrepo S, Wösten HA, de Cock H (2017) Highly efficient transformation system for Malassezia furfur and Malassezia pachydermatis using Agrobacterium tumefaciens-mediated transformation. J Microbiol Methods 134:1–6
Ianiri G, Averette AF, Kingsbury JM, Heitman J, Idnurm A (2016) Gene function analysis in the ubiquitous human commensal and pathogen Malassezia genus. mBio 7(6):e01853-16
Park M, Cho YJ, Lee YW, Jung WH (2017) Whole genome sequencing analysis of the cutaneous pathogenic yeast Malassezia restricta and identification of the major lipase expressed on the scalp of patients with dandruff. Mycoses 60(3):188–197
Selander C, Engblom C, Nilsson G, Scheynius A, Andersson CL (2009) TLR2/MyD88-dependent and -independent activation of mast cell IgE responses by the skin commensal yeast Malassezia sympodialis. J Immunol 182(7):4208–4216
Al-Yasiri MH, Normand AC, L’Ollivier C, Lachaud L, Bourgeois N, Rebaudet S, Piarroux R, Mauffrey JF, Ranque S (2016) Opportunistic fungal pathogen Candida glabrata circulates between humans and yellow-legged gulls. Sci Rep 6:36157
Rizzetto L, De Filippo C, Cavalieri D (2014) Richness and diversity of mammalian fungal communities shape innate and adaptive immunity in health and disease. Eur J Immunol 44(11):3166–3181
Acknowledgements
We thank all the subjects who participated in the study. We also want to thank Shanghai Realbio technology Co., Ltd. for their technical assistance in this study.
Funding
This work was supported by grants from the National Natural Science Foundation of China (nos. 81230057, 81372615, 81472262, and 81200264); Emerging Cutting-Edge Technology Joint Research projects of Shanghai (SHDC12012106) and Tongji University Subject Pilot Program (no. 162385).
Author information
Authors and Affiliations
Contributions
R.Y. and H.L. designed the study; R.Y. and H.L. collected the samples; R.Y., L.S., and C.K. performed the experiments and data analysis, R.Y. and N.Q. interpreted the results; and R.Y. and H.L. wrote the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committee of Shanghai Tenth People’s Hospital (no. SHSY-IEC-KY-4.0/17-139/01) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflicts of interest associated with this study or its results.
Electronic supplementary material
Below are the links to the electronic supplementary material.
Fig. S1
Sequencing depth represented by Chao 1 (a) and observed species (b) in all samples from the colorectal cancer (C), polyp (P), and healthy control (N) groups (GIF 78 kb)
Fig. S2
Operational taxonomic units (OTUs) detected and diversity in the colorectal cancer (C), polyp (P), and healthy control (N) groups. a Shared and specific OTUs in the C, P, and N groups. b Number of core OTU (Y axis) changes in all samples of the three groups, along with the fraction of samples increasing. Calculated α diversity, including observed species diversity index (c), Chao 1 diversity index (d), and Shannon diversity index (e), in the C, P, and N groups (GIF 78 kb)
Fig. S3
The change in fungal diversity in early- and late-stage colorectal cancer. Shannon diversity index (a) and Simpson index (b) were calculated and showed statistical significance between the early and late cancer stages (p Shannon = 0.004; p Simpson = 0.01) (GIF 24 kb)
Rights and permissions
About this article
Cite this article
Gao, R., Kong, C., Li, H. et al. Dysbiosis signature of mycobiota in colon polyp and colorectal cancer. Eur J Clin Microbiol Infect Dis 36, 2457–2468 (2017). https://doi.org/10.1007/s10096-017-3085-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3085-6