Abstract
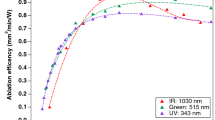
This study aimed to evaluate the possibility of introducing ultra-short pulsed lasers (USPL) in restorative dentistry by maintaining the well-known benefits of lasers for caries removal, but also overcoming disadvantages, such as thermal damage of irradiated substrate. USPL ablation of dental hard tissues was investigated in two phases. Phase 1—different wavelengths (355, 532, 1,045, and 1,064 nm), pulse durations (picoseconds and femtoseconds) and irradiation parameters (scanning speed, output power, and pulse repetition rate) were assessed for enamel and dentin. Ablation rate was determined, and the temperature increase measured in real time. Phase 2—the most favorable laser parameters were evaluated to correlate temperature increase to ablation rate and ablation efficiency. The influence of cooling methods (air, air–water spray) on ablation process was further analyzed. All parameters tested provided precise and selective tissue ablation. For all lasers, faster scanning speeds resulted in better interaction and reduced temperature increase. The most adequate results were observed for the 1064-nm ps-laser and the 1045-nm fs-laser. Forced cooling caused moderate changes in temperature increase, but reduced ablation, being considered unnecessary during irradiation with USPL. For dentin, the correlation between temperature increase and ablation efficiency was satisfactory for both pulse durations, while for enamel, the best correlation was observed for fs-laser, independently of the power used. USPL may be suitable for cavity preparation in dentin and enamel, since effective ablation and low temperature increase were observed. If adequate laser parameters are selected, this technique seems to be promising for promoting the laser-assisted, minimally invasive approach.







Similar content being viewed by others
References
Peters MC, McLean ME (2001) Minimally invasive operative care. II. Contemporary techniques and materials: an overview. J Adhes Dent 3(1):17–31
Setien VJ, Cobb DS, Denehy GE, Vargas MA (2001) Cavity preparation devices: effect on microleakage of class V resin-based composite restorations. Am J Dent 14(3):157–162
Cozean C, Arcoria CJ, Pelagalli J, Powell GL (1997) Dentistry for the 21st century? Erbium:YAG laser for teeth. J Am Dent Assoc 128(8):1080–1087
Keller U, Hibst R, Geurtsen W, Schilke R, Heidemann D, Klaiber B, Raab WH (1998) Erbium:YAG laser application in caries therapy. Evaluation of patient perception and acceptance. J Dent 26(8):649–656
Keller U, Hibst R (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances: II. Light microscopic and SEM investigations. Lasers Surg Med 9(4):345–351
Dostalova T, Jelinkova H, Kucerova H (1998) Er:YAG laser ablation-evaluation after two-years long clinical treatment. Proc SPIE 3248:23–32
Gouw-Soares S, Gutknecht N, Conrads G, Lampert F, Matson E, Eduardo CP (2000) The bactericidal effect of Ho:YAG laser irradiation within contaminated root dentinal samples. J Clin Laser Med Surg 18(2):81–87
Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ (2000) Minimal intervention dentistry—a review. FDI Commission Project 1–97. Int Dent J 50(1):1–12
Rode AV, Gamaly EG, Luther-Davies B, Taylor BT, Graessel M, Dawes JM, Chan A, Lowe RM, Hannaford P (2003) Precision ablation of dental enamel using a subpicosecond pulsed laser. Aust Dent J 48(4):233–239
Chan A, Rode A, Gamaly E, Luther-Davies B, Taylor B, Dawes J, Lowe M, Hannaford P (2003) Ablation of dental enamel using subpicosecond pulsed lasers. Int Congr Ser 1248:117–119
Fahey M, Onyejekwe O, Mason HL, Mitra K (2008) Precise dental ablation using ultra-short-pulsed 1552 nm laser. Int J Heat Mass Transf 51:5732–5739
Sheth KK, Staninec M, Sarma AV, Fried D (2004) Selective targeting of protein, water, and mineral in dentin using UV and IR pulse lasers: the effect on the bond strength to composite restorative materials. Lasers Surg Med 35(4):245–253
Wheeler CR, Fried D, Featherstone JD, Watanabe LG, Le CQ (2003) Irradiation of dental enamel with Q-switched lambda = 355-nm laser pulses: surface morphology, fluoride adsorption, and adhesion to composite resin. Lasers Surg Med 32(4):310–317
van Gemert MJ, Welch AJ (1989) Time constants in thermal laser medicine. Lasers Surg Med 9(4):405–421
Dela Rosa A, Sarma AV, Le CQ, Jones RS, Fried D (2004) Peripheral thermal and mechanical damage to dentin with microsecond and sub-microsecond 9.6 microm, 2.79 microm, and 0.355 microm laser pulses. Lasers Surg Med 35(3):214–228
Niemz MH (1998) Ultrashort laser pulses in dentistry, advantages and limitations. SPIE 3255:84–91
Kurtz RM, Elner V, Liu X, Juhasz T (1997) Plasma-mediated ablation of biological tissue with picosecond and femtosecond laser pulses. SPIE 2975:192–200
Perry MD, Stuart BC, Banks PS, Feit MD, Yanovsky V, Rubenchik AM (1999) Ultrashort-pulse laser machining of dielectric materials. J Appl Phys 9(85):6803–6810
Lizarelli RF, Kurachi C, Misoguti L, Bagnato VS (2000) A comparative study of nanosecond and picosecond laser ablation in enamel: morphological aspects. J Clin Laser Med Surg 18(3):151–157
Niemz M (1996) Laser tissue interactions: fundamentals and applications. Springer, Berlin
Lizarelli RF, Moriyama LT, Bagnato VS (2006) Temperature response in the pulpal chamber of primary human teeth exposed to Nd:YAG laser using a picosecond pulsed regime. Photomed Laser Surg 24(5):610–615
de Lizarelli FZR, Moriyama LT, Bagnato VS (2002) Ablation rate and micromorphological aspects with Nd:YAG picosecond pulsed laser on primary teeth. Lasers Surg Med 31(3):177–185
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530
Ceballo L, Toledano M, Osorio R, Tay FR, Marshall GW (2002) Bonding to Er-YAG-laser-treated dentin. J Dent Res 81(2):119–122
Uhrig G, Meyer D, Foth HJ (2001) Transient FEM calculation of the spatial heat distribution in hard dental tissue during and after IR laser ablation. Proc SPIE 4249:61–71
Braun A, Wehry RJ, Brede O, Dehn C, Frentzen M, Schelle F (2012) Heat generation caused by ablation of restorative materials with an ultrashort pulse laser (USPL) system. Lasers Med Sci. 27(2):297–303
Visuri SR, Walsh JT Jr, Wigdor HA (1996) Erbium laser ablation of dental hard tissue: effect of water cooling. Lasers Surg Med 18(3):294–300
Meister J, Franzen R, Forner K, Grebe H, Stanzel S, Lampert F, Apel C (2006) Influence of the water content in dental enamel and dentin on ablation with erbium YAG and erbium YSGG lasers. J Biomed Opt 11(3):34030
Staninec M, Xie J, Le CQ, Fried D (2003) Influence of an optically thick water layer on the bond-strength of composite resin to dental enamel after IR laser ablation. Lasers Surg Med 33(4):264–269
Fried D, Ashouri N, Breunig T, Shori R (2002) Mechanism of water augmentation during IR laser ablation of dental enamel. Lasers Surg Med 31(3):186–193
Hibst R, Keller U (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med 9(4):338–344
Altshuler GB, Belikov AV, Sinelnik YA (2001) A laser-abrasive method for the cutting of enamel and dentin. Lasers Surg Med 28(5):435–444
Bader C, Krejci I (2006) Indications and limitations of Er:YAG laser applications in dentistry. Am J Dent 19(3):178–186
Kim BM, Eichler J, Da Silva LB (1999) Frequency doubling of ultrashort laser pulses in biological tissues. Appl Opt 38(34):7145–7150
Mehl A, Kremers L, Salzmann K, Hickel R (1997) 3D volume-ablation rate and thermal side effects with the Er:YAG and Nd:YAG laser. Dent Mater 13(4):246–251
Hossain M, Nakamura Y, Yamada Y, Kimura Y, Nakamura G, Matsumoto K (1999) Ablation depths and morphological changes in human enamel and dentin after Er:YAG laser irradiation with or without water mist. J Clin Laser Med Surg 17(3):105–109
Kim BM, Feit MD, Rubenchik AM, Joslin EJ, Celliers PM, Eichler J, Da Silva LB (2001) Influence of pulse duration on ultrashort laser pulse ablation of biological tissues. J Biomed Opt 6(3):332–338
Acknowledgments
The authors would like to express their gratitude to DAAD and CAPES (BEX3095/08-8) for their financial support of the sandwich-type doctor program, FAPESP (2008/00668-3) for the PhD scholarship, and Washington Steagall Jr. for the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bello-Silva, M.S., Wehner, M., de Paula Eduardo, C. et al. Precise ablation of dental hard tissues with ultra-short pulsed lasers. Preliminary exploratory investigation on adequate laser parameters. Lasers Med Sci 28, 171–184 (2013). https://doi.org/10.1007/s10103-012-1107-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-012-1107-2