Abstract
In this article, the authors are presenting their experience and the results with combined craniofacial resection of anterior skull base tumors based on a review of 27 constitutive cases. Our data are evaluated in comparison to other major centers in other parts of the world, and possible factors that might influence surgical outcome and survival are discussed. Twenty-seven patients diagnosed with anterior skull base tumors between 1999 and 2009 were treated by combined craniofacial resection. Of these patients, there were 19 males (70, 3%) and eight females (29, 7%). The age ranged between 11 and 75 years (mean = 45.9 ± 17.6 years). The follow-up period ranged between 14 and 123 months (avarage = 74 months). The most common presenting symptoms were nasal obstruction and vision disturbance (11 patients for each −40.7%). Total resection was achieved in 24 patients (89%), while subtotal resection was done in three patients (11%). The most common complication was CSF fistule with rhinorrhea, which occurred in five patients (18.5%). Eight patients had recurrences at the time of this long-term follow-up. There were two mortalities in the early postoperative period and seven deaths in the long-term follow-up (overall mortality, 33.3%). The overall 5-year overall survival for all patients in our series was 70.4%. The 5-year overall survival was 62% for patients with malignant tumors and 100% for patients with benign tumors. Combined craniofacial resection of tumors of the anterior skull base is an effective approach for the management of these pathologies. The effectiveness is clearly demonstrated by the clinical results and outcomes of these patients’ groups. The favorable prognosis is enhanced by significantly by total resection with negative tumor margins.



Similar content being viewed by others
References
Abuzayed B, Kafadar AM, Oğuzoğlu SA, Canbaz B, Kaynar MY (2009) Duraplasty using autologous fascia lata reenforced by on-site pedicled muscle flap: technical note. J Craniofac Surg 20(2):435–438
Abuzayed B, Tanriover N, Gazioglu N, Akar Z (2010) Extended endoscopic endonasal approach to the clival region. J Craniofac Surg 21(1):245–251
Abuzayed B, Tanriover N, Gazioglu N, Cetin G, Akar Z (2009) Extended endoscopic endonasal approach to the pterygopalatine fossa: anatomic study. J Neurosurg Sci 53(2):37–44
Abuzayed B, Tanriover N, Gazioglu N, Eraslan BS, Akar Z (2009) Endoscopic endonasal approach to the orbital apex and medial orbital wall: anatomic study and clinical applications. J Craniofac Surg 20(5):1594–1600
Abuzayed B, Tanriover N, Gazioglu N, Sanus GZ, Ozlen F, Biceroglu H, Kafadar AM, Akar Z (2010) Endoscopic endonasal anatomy and approaches to the anterior skull base: a neurosurgeon’s standpoint. J Craniofac Surg 21(2):529–537
Arita N, Mori S, Sano M, Hayakawa T, Nakano K, Kanai N, Mogami H (1989) Surgical treatment of tumors in the anterior skull base using transbasal approach. Neurosurgery 24:379–384
Barrow DL, Nahai F, Tindall GT (1984) The use of greater omentum vascularized free flaps for neurosurgical disorders requiring reconstruction. J Neurosurg 60:305–311
Bilsky MH, Kraus DH, Strong EW, Harrison LB, Gutin PH, Shah JP (1997) Extended anterior craniofacial resection for intracranial extension of malignant tumors. Am J Surg 174:565–568
Blacklock JB, Weber RS, Lee YY, Goepfert H (1989) Transcranial resection of tumors of the paranasal sinuses and nasal cavity. J Neurosurg 71:10–15
Boyle JO, Shah KC, Shah JP (1998) Craniofacial resection for malignant neoplasms of the skull base: an overview. J Surg Oncol 69:275–284
Bridger GP, Baldwin M (1989) Anterior craniofacial resection for ethmoid and nasal cancer with free flap reconstruction. Arch Otolaryngol Head Neck Surg 115:308–312
Bridger GP, Baldwin M, Gonski A (1986) Craniofacial resection for paranasal sinus cancer with free flap repair. Aust N Z J Surg 56:843–847
Bridger GP, Kwok B, Baldwin M, Williams JR, Smee RI (2000) Craniofacial resection for paranasal sinus cancers. Head Neck 22:772–780
Cansiz H, Tahamiler R, Yener M, Acoğlu E, Güvenç MG, Papila I, Sekercioğlu N (2008) Modified midfacial degloving approach for sinonasal tumors. J Craniofac Surg 19(6):1518–1522
Cantù G, Riccio S, Bimbi G, Squadrelli M, Colombo S, Compan A, Rossi M, Pompilio M, Solero CL (2006) Craniofacial resection for malignant tumors involving the anterior skull base. Eur Arch Otorhinolaryngol 263:647–652
Close LG, Mickey B (1992) Transcranial resection of ethmoid sinus cancer involving the anterior skull base. Skull Base Surg 2:213–219
Dandy WE (1941) Orbital tumors. Results following the transcranial operative attack. Oskar Piest, New York
Derome PJ (1982) The transbasal approach to tumors invading the base of the skull. In: Schmidek HH, Sweet WH (eds) Operative Neurosurgical Techniques: Indications, Methods, and Results. Grune & Stratton, Boston, pp 357–379
Dias FL, Sá GM, Kligerman J, Lopes HF, Wance JR, Paiva FP, Benévolo A, Freitas EQ (1999) Complication of anterior craniofacial resection. Head Neck 21:12–20
Donald PJ (1999) Complications in skull base surgery for malignancy. Laryngoscope 1:1959–1966
Feiz-Erfan I, Spetzler RF, Horn EM, Porter RW, Beals SP, Lettieri SC, Joganic EF, Demonte F (2008) Proposed classification for the transbasal approach and its modifications. Skull Base 1:29–47
Fliss DM, Gil Z, Spektor S, Leider-Trejo L, Abergel A, Khafif A, Amir A, Gur E, Cohen JT (2002) Skull base reconstruction after anterior subcranial tumor resection. Neurosurg Focus 12:E10
Ganly I, Patel SG, Singh B, Kraus DH, Bridger PG, Cantu G, Cheesman A, De Sa G, Donald P, Fliss D, Gullane P, Janecka I, Kamata SE, Kowalski LP, Levine P, Medina LR, Pradhan S, Schramm V, Snyderman C, Wei WI, Shah JP (2005) Complications of craniofacial resection for malignant tumors of the skull base: report of an international collaborative study. Head Neck 27:575–584
Gil Z, Patel SG, Cantu G, Fliss DM, Kowalski LP, Singh B, Snyderman C, Kraus DH, Shah JP, International Collaborative Study Group, Bridger PG, Cheesman AD, Donald P, Gullane P, Janecka I, Kamata SE, Levine PA, Medina LR, Pradhan S, Schramm V, Wei WI (2009) Outcome of craniofacial surgery in children and adolescents with malignant tumors involving the skull base: an international collaborative study. Head Neck 31(3):308–317
Hao SP (2001) Facial translocation approach to the skull base: the viability of translocated facial bone graft. Otolaryngol Head Neck Surg 124:292–296
Harrison DFN (1976) The management of malignant tumors affecting the maxillary and ethmoidal sinuses. J Laryngol Otol 90:69–74
Hendryk S, Czecior E, Misiołek M, Namysłowski G, Mrówka R (2004) Surgical strategies in the removal of malignant tumors and benign lesions of the anterior skull base. Neurosurg Rev 27(3):205–213
Jackson IT, Adham NM, Marsh WR (1986) Use of the galea frontalis myofascial flap in craniofacial surgery. Plast Reconst Surg 77:905–910
Janecka IP (1996) Facial translocation approach. In: Janecka IP, Tiedemann K (eds) Transskull base surgery. Anatomy, biology and technology. Lippincott-Raven, Philadelphia, pp 183–219
Kassam A, Carrau RL, Snyderman CH, Gardner P, Mintz A (2005) Evolution of reconstructive techniques following endoscopic expanded endonasal approaches. Neurosurg Focus 19:E8
Kassam A, Gardner P, Snyderman C, Mintz A, Carrau R (2005) Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus 19:E6
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus 19:E3
Kawakami K, Yamanouchi Y, Kawamura Y, Matsumura H (1991) Operative approach to the frontal skull base: extensive transbasal approach. Neurosurgery 28:720–724
Ketcham AS, Van Buren JM (1985) Tumors of the paranasal sinuses: a therapeutic challenge. Am J Surg 150:406–413
Kobayashi M, Nakamura T, Tamura J, Kikutani T, Nishiguchi S, Mousa WF, Takahashi M, Kokubo T (1999) Osteoconductivity and bone-bonding strength of high- and low-viscous bioactive bone cements. J Biomed Mater Res 48(3):265–276
Kraus DH, Sterman BM, Levine HL, Wood BG, Tucker HM, Lavertu P (1992) Factors influencing survival in ethmoid sinus cancer. Arch Otolaryngol Head Neck Surg 118:367–372
Kryzanski JT, Annino DJ, Gopal H, Heilman CB (2008) Low complication rates of cranial and craniofacial approaches to midline anterior skull base lesions. Skull Base 18:229–241
Kryzanski JT, Annio DJ Jr, Heilman CB (2002) Complication avoidance in the treatment of malignant tumors of the skull base. Neurosurg Focus 12:E11
Langstein HN, Chang DW, Robb GL (2001) Coverage of skull base defects. Clin Plast Surg 28:375–387
Lanza DC, O’Brien DA, Kennedy DW (1996) Endoscopic repair of cerebrospinal fluid fistulae and encephaloceles. Laryngoscope 106:1119–1125
Lee F, Ogura JH (1981) Maxillary sinus carcinoma. Laryngoscope 91:133–139
Lesoin F, Thomas CE 3rd, Villette L, Pellerin P, Jomin M (1987) The midline supra-orbital approach, using a large single free bone flap. Technical note. Acta Neurochir (Wien) 87:86–89
Levine PA, Debo RF, Meredith SD, Jane JA, Constable WC, Cantrell RW (1994) Craniofacial resection at the university of Virginia (1976–1992): survival analysis. Head Neck 16:574–577
Linderman P, Eklund V, Petruson B (1987) Survival after surgical treatment for maxillary neoplasms of epithelial origin. J Laryngol Otol 101:564–568
Lund VJ, Howard DJ, Wei WI, Cheesman AD (1998) Craniofacial resection for tumors of the nasal cavity and paranasal sinuses—a 17 year experience. Head Neck 20:97–105
McCaffrey TV, Olsen KD, Yohanan JM, Lewis JE, Ebersold MJ, Piepgras DG (1994) Factors affecting survival of patients with tumors of the anterior skull base. Laryngoscope 104:940–945
Mc Cutcheon IE, Blacklock JB, Weber RS, DeMonte F, Moser RP, Byers M, Goepfert H (1996) Anterior transcranial (craniofacial) resection of tumors of the paranasal sinuses: surgical technique and results. Neurosurgery 28:471–480
McNicollW HN, Dalley VM, Shaw HJ (1984) Cancer of the paranasal sinuses and nasal cavities. Part II. Results of treatment. J Laryngol Otol 98:707–718
Morita A, Sekhar LN (2000) Skull base tumors. In: Bernstein M, Berger MS (eds) Neuro-Oncology: the essentials. Thieme, New York, pp 419–433
Ozlen F, Abuzayed B, Dashti R, Isler C, Tanriover N, Sanus GZ (2010) Low-profile 1-piece bifrontal craniotomy for anterior skull base approach and reconstruction. J Craniofac Surg 21:233–238
Patel SG, Singh B, Polluri A, Bridger PG, Cantu G, Cheesman AD, deSa GM, Donald P, Fliss D, Gullane P, Janecka I, Kamata SE, Kowalski LP, Kraus DH, Levine PA, dos Santos LR, Pradhan S, Schramm V, Snyderman C, Wei WI, Shah JP (2003) Craniofacial surgery for malignant skull base tumors. Report of an international collaborative study. Cancer 98:1179–1187
Raza SM, Conway JE, Li KW, Attenello F, Boahene K, Subramanian P, Quinones-Hinojosa A (2010) A modified frontal-nasal-orbital approach to midline lesions of the anterior cranial fossa and skull base: technical note with case illustrations. Neurosurg Rev 33(1):63–70
Rodrigues M, O’malley BW Jr, Staecker H, Tamargo R (2004) Extended pericranial flap and bone graft reconstruction in anterior skull base surgery. Otolaryngol Head Neck Surg 131:69–76
Ross DA, Marentette LJ, Moore CE, Switz KL (1999) Craniofacial resection: decreased complication rate with a modified subcranial approach. Skull Base Surg 9:95–100
Sanus GZ, Abuzayed B (2009) Rhinorrhea as a rare but disturbing complication of rhinoplasty [Comment]. J Craniofac Surg 20(5):1625
Sanus GZ, Tanriverdi T, Kafadar AM, Ulu MO, Uzan M (2005) Use of Cortoss for reconstruction of anterior cranial base: a preliminary clinical experience. Eur J Plast Surg 27:371–377
Sanus GZ, Tanriverdi T, Ulu MO, Kafadar AM, Tanriover N, Ozlen F (2008) Use of cortoss as an alternative material in calvarial defects: the first clinical results in cranioplasty. J Craniofac Surg 19(1):88–95
Sekhar JP, Nanada A, Sen CN, Snyderman CN, Janecka IP (1992) The extended frontal approach to tumors of anterior, middle, and posterior base. J Neurosurg 76:196–206
Sekhar LN, Pomeranz S, Janecka IP, Hirsch B, Ramasastry S (1992) Temporal bone neoplasms: a report on 20 surgically treated cases. J Neurosurg 76:578–587
Senyuva C, Yucel A, Okur I, Cansiz H, Sanus Z (1996) Free rectus abdominis muscle flap for the treatment of complications after neurosurgical procedures. J Craniofac Surg 7:317–321
Shah JP, Kraus DH, Arbit E, Kraus DH, Arbit E, Galicich JH, Strong EW (1992) Craniofacial resection for tumors involving the anterior skull base. Otolaryngol Head Neck Surg 106:387–393
Shah JP, Kraus DH, Bilsky MH, Gutin PH, Harrison LH, Strong EW (1997) Craniofacial resection for malignant tumors involving the anterior skull base. Arch Otolaryngol Head Neck Surg 123:1312–1317
Sinha UK, Johnson TE, Crockett D, Vadapalli S, Gruen P (2002) Three-layer reconstruction for large defects of the anterior skull base. Laryngoscope 112:424–427
Smith RR, Klopp CT, Williams JM (1954) Surgical treatment of cancer of the frontal sinus and adjacent areas. Cancer 7:991–994
Spetzler RF, Herman JM, Beals S, Joganic E, Milligan J (1993) Preservation of olfaction in anterior craniofacial approaches. J Neurosurg 79:48–52
Suarez C, Llorente JL, Fernandez De Leon R, Maseda E, Lopez A (2004) Prognostic factors in sinonasal tumors involving the anterior skull base. Head Neck 26:136–144
Tsai EC, Santoreneos S, Rutka JT (2002) Tumors of the skull base in children: review of tumor types and management strategies. Neurosurg Focus 12:E1
Van Buren JM, Ommaya AK, Ketcham AS (1968) Ten years’ experience with radical combined craniofacial resection of malignant tumors of the paranasal sinuses. J Neurosurg 28:341–350
Vrionis FD, Kienstra MA, Rivera M, Padhya TA (2004) Malignant tumors of the anterior skull base. Cancer Control 11:144–151
Wellman BJ, Traynelis VC, McCulloch TM, Funk GF, Menezes AH, Hoffman HT (1999) Midline anterior craniofacial approach for malignancy: results of en bloc versus piecemeal resections. Skull Base Surg 9:41–46
Weymuller EA, Reardon EJ, Nash D (1980) Comparison of treatment modalities in carcinoma of the maxillary sinus. Arch Otolaryngol 106:625–629
Wong LY, Lam LK, Fan YW, Yuen AP, Wei WI (2006) Outcome analysis of patients with craniofacial resection: Hong Kong experience. ANZ J Surg 76(5):313–317
Yoshioka N, Rhoton AL (2005) Vascular anatomy of the anteriorly based pericranial flap. Neurosurgery 57(suppl 1):11–16
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Dattatraya Muzumdar, Mumbai, India
Abuzayed et al. report their experience with tumors of combined craniofacial resection for the treatment of anterior skull base tumors from Turkey. It is the first to be published in the English literature from Turkey.
Combined craniofacial resection is performed with an aim to achieve an oncological cure for tumors straddling the anterior, lateral, or posterior fossa skull base. Excision of the tumor along with negative oncological margins is the paramount to justify the radical nature of surgery. A sound anatomical knowledge of the anterior, lateral, and the posterior skull base is necessary. The surgery is best performed in a tertiary oncology center by a multidisciplinary team comprising of a neurosurgeon and otolaryngologist having exposure to and training in skull base surgery. In anterior skull base tumors, combined craniofacial resection is indicated in patients with suspected cribriform plate involvement or dural invasion. In fact, a good negative margin could be achieved in tumors which involve the cribriform plate but do not erode it.
The authors correctly emphasize that the operative resection margin is an important independent prognostic factor affecting survival in patients with malignant tumor in the skull base. The overall 5-year survival was 54% for malignant tumors and 100% for benign tumors which is comparable with the international literature. However, the pathological and aggressive behavior of the tumor also has an impact on the overall prognosis.
Proper selection of the patient for anterior craniofacial resection is important for an optional outcome. A midfacial degloving approach and a low bifrontal craniotomy can also provide wide exposure of the anterior skull base and help lessen facial osteotomies. Endoscopic resection for malignant anterior skull base tumors is controversial since it defies the oncological definitions of resections with negative margins. Also the rate of CSF leak and resultant morbidity tends to be higher in endoscopic resections since it has a steep learning curve and standardization is yet to occur for it to be included in the standard of care for anterior skull base malignant tumors.
Uğur Türe and Christian Brogna, İstanbul, Turkey
The authors retrospectively analyze a 10-year institutional experience with 27 consecutive patients harboring a benign or malignant tumor of the anterior cranial base. Fourteen patients were newly diagnosed with anterior skull base tumors, and 13 were operated on previously: five through the transcranial approach alone, three with the transfacial approach alone, and five with the combined craniofacial approach. The tumor extended toward the orbit in 12 patients, the middle cranial fossa in eight, and the cavernous sinus in two.
A combined craniofacial resection—a bilateral frontobasal approach combined with a lateral rhinotomy or modified midfacial degloving or the transnasal approach—was the approach used in this series. The authors do not report how many patients underwent each type of transfacial approach.
Total resection was achieved in 24 patients, with subtotal in three patients. The authors state that the most important negative factor influencing the degree of resection was an extension toward the middle fossa, cavernous sinus, orbital apex, or superior orbital fissure and the involvement of the internal carotid artery. Nevertheless, in one of the three patients having subtotal resection, none of these structures was involved.
The series presented is heterogeneous. Histopathological examination revealed two juvenile angiofibromas, two transitional meningiomas, two atypical meningiomas, one anaplastic meningioma, five squamous cell carcinomas, two epidermoid carcinomas, two adenocystic carcinomas, three sinonasal adenocarcinomas, one hemangioendothelioma, one fibroblastic osteosarcoma, one chondrosarcoma, one mesenchymal type chondrosarcoma, one rhabdomyosarcoma, one esthesioneuroblastoma, one malignant desmoplastic small round cell tumor originating in the meninges, and one inverted papilloma.
Large dural defects were repaired with a duraplasty of the temporal muscle or a fascia lata graft. The report does not mention how many patients needed this procedure.
Only two patients had preoperative anosmia, but all patients had postoperative anosmia due to the bilateral frontobasal approach. Of the five patients having a postoperative CSF fistula, three required lumbar drainage while two needed a second surgical look. One patient died after the development of a CSF leak, which caused an abscess and cerebritis.
The 5-year overall survival for patients with benign tumors was 100%. Those with malignant tumors had a 5-year survival of 62%. The median time to recurrence was 17 months. While four patients died of recurrences, three died after progression of the residual tumor.
The authors present a relatively large surgical series of anterior cranial base tumors and we congratulate them for dealing with this complex topic with great success in terms of the percentage of patients having total removal. The best treatment and surgical approach to anterior cranial base tumors are still a matter of debate. We would like to discuss the different philosophies and surgical strategies we use in these cases.
First of all, analyzing benign and malignant tumors in the same series can be confusing. In fact, benign and malignant tumors of the anterior cranial base differ in many fundamental aspects, such as the patient’s age and clinical status at presentation, the tumor’s natural history, and the overall philosophy of the use of surgical and adjuvant treatment.
In our opinion, meningiomas of the anterior cranial base rarely require a combined craniofacial approach to be resected totally. For meningiomas arising from the olfactory groove, tuberculum sella, or the medial or lateral sphenoidal ridge, we prefer a pterional-transsylvian exploration and avoid a bilateral subfrontal approach. A subfrontal approach requires retraction of both frontal lobes and causes bilateral frontal lobe damage and postoperative anosmia because both olfactory nerves are usually damaged during this approach. On the other hand, the pterional approach provides a better orientation for the relationships between the meningioma and adjacent vital structures around the sella, without retraction of the frontal lobes. The pterional approach with dissection of the contralateral olfactory nerve from the capsule of the tumor allows the preservation of olfactory function, even in patients with olfactory groove meningiomas. If a surgeon prefers greater working space, the cranio-orbital zygomatic approach can be used.
Juvenile nasopharyngeal angiofibromas (JNAs) are rare, benign, vascular tumors. The blood supply to these lesions is most commonly from the maxillary artery, but may also come from the external carotid artery, the internal carotid artery, the common carotid artery, or the ascending pharyngeal artery. The case of JNA described by the authors involved the nasopharyngeal cavity with extension towards the left sphenoid bone, cavernous sinus, and optic canal. This patient was previously operated on with a combined craniofacial resection and the authors have chosen the same approach for the second surgery. In this case, however, we would prefer to selectively embolize feeding vessels preoperatively. The authors achieved only a subtotal resection with a combined craniofacial resection. Even though JNAs are benign lesions, the recurrence rate is high with residual pathology.
Malignant tumors, such as squamous cell carcinomas or sinonasal adenocarcinomas, require totally different management than benign tumors. In malignant cases, oncological resection is accomplished when en bloc resection includes at least 5 mm of normal tissue beyond the tumor, as determined through histological examination. Moreover, adjuvant therapies such as radiotherapy or, less commonly, chemotherapy must be administered. Treating patients with malignant tumors more complex than benign tumors. Unfortunately, some patients with malignant lesions of the anterior cranial base have already undergone radiotherapy or only partial surgical removal before the tumor reaches the skull base. Previous radiotherapy is correlated with an overall decrease in the 5-year survival and adjuvant radiotherapy carries a high risk of morbidity and local recurrence. Moreover, a delay of surgical treatment may allow the tumor to progress or invade the dura.
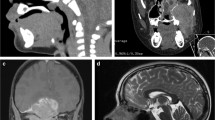
In patients with malignant tumors of the anterior cranial base, the combined craniofacial approach can be useful to effect an oncological resection. The modified midfacial degloving used by the authors provides a more cosmetically acceptable surgical route with respect to the lateral rhinotomy. However, in patients with extensive infiltration of the orbital structures, an orbital exenteration with prosthesis reconstruction may be necessary. We likely would have used a left cranio-orbital zygomatic approach to resect the epidermoid carcinoma presented by the authors as the illustrative case. The use of this approach could have gained the same total oncological resection but avoided retraction of the frontal lobes, sparing the contralateral olfactory nerve and preserving the mucosa of the nasal cavities. Unfortunately, this is the only case for which the authors present images. It would have been useful to have other cases to discuss.
The use of intraoperative lumbar drainage in selected cases, which is not mentioned in this paper, allows a good release of cerebrospinal fluid to minimize the need for brain retraction. We then make every effort to prevent cerebrospinal fluid rhinorrhea, which could be life-threatening. We prefer to close the dural defects with pericranium and fill major sinuses with autologous fat. In patients undergoing radiation therapy preoperatively or if a potential for CSF leakage occurs during surgery, we leave the lumbar drain in place for 5–7 days postoperatively.
We congratulate the authors for their efforts with these formidable lesions. Unfortunately, the controversies concerning their treatment will not be resolved in the near future.
Rights and permissions
About this article
Cite this article
Abuzayed, B., Canbaz, B., Sanus, G.Z. et al. Combined craniofacial resection of anterior skull base tumors: long-term results and experience of single institution. Neurosurg Rev 34, 101–113 (2011). https://doi.org/10.1007/s10143-010-0286-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0286-1