Abstract
Background
Artificial neural networks (ANNs) can be used to develop predictive tools to enable the clinical decision-making process. This study aimed to investigate the use of an ANN in predicting the outcomes from enhanced recovery after colorectal cancer surgery.
Methods
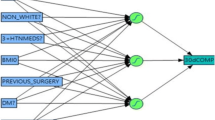
Data were obtained from consecutive colorectal cancer patients undergoing laparoscopic surgery within the enhanced recovery after surgery (ERAS) program between 2002 and 2009 in a single center. The primary outcomes assessed were delayed discharge and readmission within a 30-day period. The data were analyzed using a multilayered perceptron neural network (MLPNN), and a prediction tools were created for each outcome. The results were compared with a conventional statistical method using logistic regression analysis.
Results
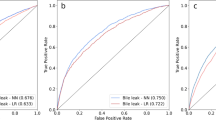
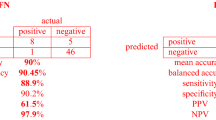
A total of 275 cancer patients were included in the study. The median length of stay was 6 days (range 2–49 days) with 67 patients (24.4 %) staying longer than 7 days. Thirty-four patients (12.5 %) were readmitted within 30 days. Important factors predicting delayed discharge were related to failure in compliance with ERAS, particularly with the postoperative elements in the first 48 h. The MLPNN for delayed discharge had an area under a receiver operator characteristic curve (AUROC) of 0.817, compared with an AUROC of 0.807 for the predictive tool developed from logistic regression analysis. Factors predicting 30-day readmission included overall compliance with the ERAS pathway and receiving neoadjuvant treatment for rectal cancer. The MLPNN for readmission had an AUROC of 0.68.
Conclusions
These results may plausibly suggest that ANN can be used to develop reliable outcome predictive tools in multifactorial intervention such as ERAS. Compliance with ERAS can reliably predict both delayed discharge and 30-day readmission following laparoscopic colorectal cancer surgery.







Similar content being viewed by others
References
Varadhan KK, Neal KR, Dejong CHC, Fearon KCH, Ljungqvist O, Lobo DN (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 29:434–440
Teeuwen PHE, Bliechrodt RP, Strik C et al (2010) Enhanced recovery after surgery (ERAS) versus conventional postoperative care in colorectal surgery. J Gastrointest Surg 14:88–95
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38:1531–1541
Ahmed J, Khan S, Lim M, Chandrasekaran TV, MacFie J (2012) Enhanced recovery after surgery protocols–compliance and variations in practice during routine colorectal surgery. Colorectal Dis 14:1045–1051
Lyon A, Solomon MJ, Harrison JD (2014) A qualitative study assessing the barriers to implementation of enhanced recovery after surgery. World J Surg 38:1374–1380
Maessen J, Dejong CHC, Hausel J et al (2007) A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg 94:224–231
Tu JV (1996) Advantages and disadvantages of using artificial neural networks versus logistic regression for predicting medical outcomes. J Clin Epidimiol 49:1225–1231
Ramesh AN, Kambhampati C, Monson JRT, Drew PJ (2004) Artificial intelligence in medicine. Ann R Coll Surg Engl 86:334–338
Prabhudesai SG, Gould S, Rekhaj S, Tekkis PP, Glazer G, Ziprin P (2008) Artificial neural networks: useful aid in diagnosing acute appendicitis. World J Surg 32:305–309
Bottaci L, Drew PJ, Hartley JE et al (1997) Artficial neural networks applied to outcome prediction for colorectal cancer patients in separate institutions. Lancet 16:470–472
Shi HY, Lee KT, Wang JJ, Sun DP, Lee HH, Chiu CC (2012) Artificial neural network model for predicting 5-year mortality after surgery for hepatocellular carcinoma: a nationwide study. J Gastrointest Surg 16:2126–2131
Tsai JT, Hou MF, Chen YM, Wan THT, Kao HY, Shi HY (2013) Predicting quality of life after breast cancer surgery using ANN-based models: performance comparison with MR. Support Care Cancer 21:1341–1350
Grossman R, Kamath CPK, Kumar V, Namburu R (2001) Data mining for scientific and engineering applications. Kluwer Academic Publishers, Dordrecht, The Netherlands
Kattan MW (2008) Editorial comment on: development, validation, and head-to-head comparison of logistic regression-based nomograms and artificial neural network models predicting prostate cancer on initial extended biops. Eur Urol 54:611
Zurada JM (1992) Artificial neural systems. West Publishing Company, New York, NY
Haykin S (1994) Neural networks: a comprehensive foundation. Macmillan College Publishing Company, New York, NY
Boulind C, Allison A, Burkill C, Wett A, Kennedy R, Francis N (2012) Factors predicting outcome in Enhanced Recovery after Laparoscopic colorectal surgery. Colorectal Dis 14:e103
Smart NJ, White P, Allison AS, Ockrim JB, Kennedy RH, Francis NK (2012) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 14:727–734
Hendry PO, Hausel J, Nygren J et al (2009) Determinants of outcome after colorectal resection within an enhanced recovery programme. Br J Surg 96:197–205
Birgisson H, Pahlman L, Gunnarsson U, Glimelius B, Swedisch Rectal Cancer Trial Group (2005) Adverse effects of preoperative radiation therapy for rectal cancer: long-term follow-up of the Swedish Rectal Cancer Trial. J Clin Oncol 34:8697–8705
Komori K, Kimura K, Kinoshita T et al (2014) Complications associated with postoperative adjuvant radiation therapy for advanced rectal cancer. Int Surg 2:100–105
Conflict of interest
None.
Ethical approval
Institutional approval for the study was obtained from the Research ethics board at Yeovil District Hospital NHS Foundation Trust.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Francis, N.K., Luther, A., Salib, E. et al. The use of artificial neural networks to predict delayed discharge and readmission in enhanced recovery following laparoscopic colorectal cancer surgery. Tech Coloproctol 19, 419–428 (2015). https://doi.org/10.1007/s10151-015-1319-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-015-1319-0