Abstract
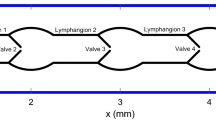
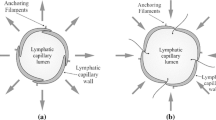
We propose a one-dimensional model for collecting lymphatics coupled with a novel Electro-Fluid-Mechanical Contraction (EFMC) model for dynamical contractions, based on a modified FitzHugh–Nagumo model for action potentials. The one-dimensional model for a deformable lymphatic vessel is a nonlinear system of hyperbolic Partial Differential Equations (PDEs). The EFMC model combines the electrical activity of lymphangions (action potentials) with fluid-mechanical feedback (circumferential stretch of the lymphatic wall and wall shear stress) and lymphatic vessel wall contractions. The EFMC model is governed by four Ordinary Differential Equations (ODEs) and phenomenologically relies on: (1) environmental calcium influx, (2) stretch-activated calcium influx, and (3) contraction inhibitions induced by wall shear stresses. We carried out a stability analysis of the stationary state of the EFMC model. Contractions turn out to be triggered by the instability of the stationary state. Overall, the EFMC model allows emulating the influence of pressure and wall shear stress on the frequency of contractions observed experimentally. Lymphatic valves are modelled by extending an existing lumped-parameter model for blood vessels. Modern numerical methods are employed for the one-dimensional model (PDEs), for the EFMC model and valve dynamics (ODEs). Adopting the geometrical structure of collecting lymphatics from rat mesentery, we apply the full mathematical model to a carefully selected suite of test problems inspired by experiments. We analysed several indices of a single lymphangion for a wide range of upstream and downstream pressure combinations which included both favourable and adverse pressure gradients. The most influential model parameters were identified by performing two sensitivity analyses for favourable and adverse pressure gradients.












Similar content being viewed by others
References
Alastruey A.J (2006) Numerical modelling of pulse wave propagation in the cardiovascular system: development, validation and clinical applications. Ph.D. thesis, University of London
Alastruey J, Parker KH, Peiró J, Sherwin SJ (2008) Lumped parameter outflow models for 1-D blood flow simulations: effect on pulse waves and parameter estimation. Commun Comput Phys 4(2):317–336
Baish JW, Kunert C, Padera TP, Munn LL (2016) Synchronization and random triggering of lymphatic vessel contractions. PLoS Comput Biol 12(12):e1005,231
Bertram C, Macaskill C, Moore J (2016) Pump function curve shape for a model lymphatic vessel. Med Eng Phys 38(7):656–663
Bertram CD, Macaskill C, Davis MJ, Moore JE (2014) Development of a model of a multi-lymphangion lymphatic vessel incorporating realistic and measured parameter values. Biomech Model Mechanobiol 13(2):401–416
Bertram C.D., Macaskill C, Davis M.J., Moore J.E (2016) Consequences of intravascular lymphatic valve properties: a study of contraction timing in a multi-lymphangion model. American Journal of Physiology: Heart and Circulatory Physiology 310(7), ajpheart.00,669.2015
Bertram CD, Macaskill C, Davis MJ, Moore JE (2017) Valve-related modes of pump failure in collecting lymphatics: numerical and experimental investigation. Biomech Model Mechanobiol 16(6):1987–2003
Bertram CD, Macaskill C, Moore JE (2011) Simulation of a chain of collapsible contracting lymphangions with progressive valve closure. J Biomech Eng 133(1):011,008
Bertram CD, Macaskill C, Moore JE (2014) Incorporating measured valve properties into a numerical model of a lymphatic vessel. Comput Methods Biomech Biomed Eng 17(14):1519–1534
Borsche R, Kall J (2016) High order numerical methods for networks of hyperbolic conservation laws coupled with ODEs and lumped parameter models. J Comput Phys 327:678–699
Breslin JW (2014) Mechanical forces and lymphatic transport. Microvasc Res 96:46–54
Caulk AW, Dixon JB, Gleason RL (2016) A lumped parameter model of mechanically mediated acute and long-term adaptations of contractility and geometry in lymphatics for characterization of lymphedema. Biomech Model Mechanobiol 15(6):1601–1618
Caulk AW, Nepiyushchikh ZV, Shaw,R, Dixon JB, Gleason RL (2015) Quantification of the passive and active biaxial mechanical behaviour and microstructural organization of rat thoracic ducts. J R Soc Interface 12(108):20150,280
Contarino C, Toro EF, Montecinos GI, Borsche R, Kall J (2016) Junction-generalized Riemann problem for stiff hyperbolic balance laws in networks: an implicit solver and ADER schemes. J Comput Phys 315:409–433
Davis MJ (2015) Is nitric oxide important for the diastolic phase of the lymphatic contraction/relaxation cycle? Proc Nat Acad Sci 113(2):E105–E105
Davis MJ, Rahbar E, Gashev AA, Zawieja DC, Moore JE (2011) Determinants of valve gating in collecting lymphatic vessels from rat mesentery. Am J Physiol Heart Circ Physiol 301(1):H48–H60
Davis MJ, Scallan JP, Wolpers JH, Muthuchamy M, Gashev AA, Zawieja DC (2012) Intrinsic increase in lymphangion muscle contractility in response to elevated afterload. Am J Physiol Heart Circ Physiol 303(7):H795–H808
Formaggia L, Quarteroni A, Veneziani A (2009) Cardiovascular Mathematics. Modeling and simulation of the circulatory system. Springer, Berlin
Franzone PC, Pavarino LF, Scacchi S (2014) Mathematical cardiac electrophysiology. Springer, Berlin
Gajani G.S, Boschetti F, Negrini D, Martellaccio R, Milanese G, Bizzarri F, Brambilla A (2015) A lumped model of lymphatic systems suitable for large scale simulations. In: 2015 European conference on circuit theory and design (ECCTD). Institute of Electrical & Electronics Engineers (IEEE)
Gashev AA (2002) Inhibition of the active lymph pump by flow in rat mesenteric lymphatics and thoracic duct. J Physiol 540(3):1023–1037
Gashev AA, Davis MM, Delp MD, Zawieja DC (2004) Regional variations of contractile activity in isolated rat lymphatics. Microcirculation 11(6):477–492
van Griensven A, Meixner T, Grunwald S, Bishop T, Diluzio M, Srinivasan R (2006) A global sensitivity analysis tool for the parameters of multi-variable catchment models. J Hydrol 324(1–4):10–23
Hodgkin AL, Huxley AF (1952) A quantitative description of membrane current and its application to conduction and excitation in nerve. J Physiol 117(4):500–544
Jamalian S, Davis MJ, Zawieja DC, Moore JE (2016) Network scale modeling of lymph transport and its effective pumping parameters. PLoS ONE 11(2):e0148,384
Kunert C, Baish JW, Liao S, Padera TP, Munn LL (2015) Mechanobiological oscillators control lymph flow. Proc Nat Acad Sci 112(35):10938–10943
LeFloch PG (2002) Hyperbolic systems of conservation laws. Springer, Berlin
Liang F, Takagi S, Himeno R, Liu H (2009) Biomechanical characterization of ventricular–arterial coupling during aging: A multi-scale model study. J Biomech 42(6):692–704
MacDonald AJ, Arkill KP, Tabor GR, McHale NG, Winlove CP (2008) Modeling flow in collecting lymphatic vessels: one-dimensional flow through a series of contractile elements. Am J Physiol Heart Circ Physiol 295(1):H305–H313
Margaris K, Black RA (2012) Modelling the lymphatic system: challenges and opportunities. J R Soc Interface 9(69):601–612
McHale NG, Roddie IC (1976) The effect of transmural pressure on pumping activity in isolated bovine lymphatic vessels. J Physiol 261(2):255–269
Müller LO, Parés C, Toro EF (2013) Well-balanced high-order numerical schemes for one-dimensional blood flow in vessels with varying mechanical properties. J Comput Phys 242:53–85
Müller LO, Toro EF (2014) Enhanced global mathematical model for studying cerebral venous blood flow. J Biomech 47(13):3361–3372
Munn LL (2015) Mechanobiology of lymphatic contractions. Semin Cell Dev Biol 38:67–74
Mynard JP, Davidson MR, Penny DJ, Smolich JJ (2012) A simple, versatile valve model for use in lumped parameter and one-dimensional cardiovascular models. Int J Numer Methods Biomed Eng 28(6–7):626–641
Nagumo J, Arimoto S, Yoshizawa S (1962) An active pulse transmission line simulating nerve axon. Proc IRE 50(10):2061–2070
Ohhashi T, Azuma T, Sakaguchi M (1980) Active and passive mechanical characteristics of bovine mesenteric lymphatics. Am J Physiol 239(1):H88–95
Quarteroni A, Lassila T, Rossi S, Ruiz-Baier R (2017) Integrated heart—coupling multiscale and multiphysics models for the simulation of the cardiac function. Comput Methods Appl Mech Eng 314:345–407
Quarteroni A, Veneziani A, Vergara C (2016) Geometric multiscale modeling of the cardiovascular system, between theory and practice. Comput Methods Appl Mech Eng 302:193–252
Rahbar E, Moore JE (2011) A model of a radially expanding and contracting lymphangion. J Biomech 44(6):1001–1007
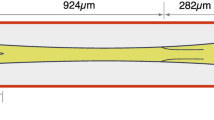
Rahbar E, Weimer J, Gibbs H, Yeh AT, Bertram CD, Davis MJ, Hill MA, Zawieja DC, Moore JE (2012) Passive pressure-diameter relationship and structural composition of rat mesenteric lymphangions. Lymphat Res Biol 10(4):152–163
Reddy N.P (1974) A discrete model of the lymphatic system. Ph.D. thesis, Texas A&M University
Scallan JP, Wolpers JH, Muthuchamy M, Zawieja DC, Gashev AA, Davis MJ (2012) Independent and interactive effects of preload and afterload on the pump function of the isolated lymphangion. Am J Physiol Heart Circ Physiol 303(7):H809–H824
Strocchi M, Contarino C, Zhang Q, Bonmassari R, Toro E (2017) A global mathematical model for the simulation of stenoses and bypass placement in the human arterial system. Appl Math Comput 300:21–39
Sun Y, Sjoberg BJ, Ask P, Loyd D, Wranne B (1995) Mathematical model that characterizes transmitral and pulmonary venous flow velocity patterns. Am J Physiol Heart Circ Physiol 268(1):H476–H489
Swartz M (2001) The physiology of the lymphatic system. Adv Drug Deliv Rev 50(1–2):3–20
Telinius N, Majgaard J, Kim S, Katballe N, Pahle E, Nielsen J, Hjortdal V, Aalkjaer C, Boedtkjer DB (2015) Voltage-gated sodium channels contribute to action potentials and spontaneous contractility in isolated human lymphatic vessels. J Physiol 593(14):3109–3122
Toro EF (2009) Riemann solvers and numerical methods for fluid dynamics, 3rd edn. Springer, Berlin
Toro EF (2016) Brain venous haemodynamics, neurological diseases and mathematical modelling. A Review. Appl Math Comput 272:542–579
Toro EF, Billett SJ (2000) Centred TVD schemes for hyperbolic conservation laws. IMA J Numer Anal 20:47–79
Toro EF, Müller L, Cristini M, Menegatti E, Zamboni P (2015) Impact of jugular vein valve function on cerebral venous haemodynamics. Curr Neurovascular Res 12(4):384–397
Toro EF, Siviglia A (2013) Flow in collapsible tubes with discontinuous mechanical properties: mathematical model and exact solutions. Commun Comput Phys 13(02):361–385
Venugopal AM, Stewart RH, Laine GA, Dongaonkar RM, Quick CM (2007) Lymphangion coordination minimally affects mean flow in lymphatic vessels. Am J Physiol Heart Circ Physiol 293(2):H1183–H1189
Wilson JT, van Loon R, Wang W, Zawieja DC, Moore JE (2015) Determining the combined effect of the lymphatic valve leaflets and sinus on resistance to forward flow. J Biomech 48(13):3584–3590
Zawieja DC (2009) Contractile physiology of lymphatics. Lymphat Res Biol 7(2):87–96
Zawieja DC, Davis KL, Schuster R, Hinds WM, Granger HJ (1993) Distribution, propagation, and coordination of contractile activity in lymphatics. Am J Physiol Heart Circ Physiol 264(4):H1283–H1291
Acknowledgements
The authors gratefully acknowledge the suggestions given by Prof. Christian Vergara from the Department of Mathematics, Politecnico di Milano, Italy. The authors also acknowledge the excellent work done by anonymous referees that greatly contributed to improve this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendices
1.1 A Mathematical analysis of the one-dimensional lymph flow equations
Here, we study the mathematical properties of (10) assuming constant parameters along the lymphatic vessel. The equations in (10) are a generalization of the one-dimensional blood flow equations (Toro 2016). As a matter of fact, the main difference is an additional term in the tube law (3). For this reason, here we summarize the main mathematical structure of the lymph flow equations without proofs. System (10) can be written in quasi-linear form as
where
The eigenvalues of matrix \(\mathbf {A}\) are
where c is the wave speed
We assume parameters \(m\ge 0\), \(n\le 0\), \(z\ge 0\), and \(C\ge 0\) for the tube law. Thus, the wave speed c is always real. The wave speed increases actively during contraction as it depends on the coefficient K. This means that during lymphatic contraction, the lymphatic wall becomes stiffer and waves propagate at a faster rate. The eigenvectors of \(\mathbf {A}\) are
where \(\gamma _1\) and \(\gamma _2\) are arbitrary scaling factors. It can be shown that system (10) is hyperbolic, as the eigenvalues are real and distinct and the eigenvectors \(\mathbf {R}_1\) and \(\mathbf {R}_2\) are linearly independent. Following proofs in Toro (2016) and references therein, the \(\lambda _1\) and \(\lambda _2\) characteristic fields are genuinely nonlinear outside the locus of the following function
With the choice of parameters m, n, z, and C in Table 1, there exists at least one solution of \(G\left( \frac{A}{A_0}\right) =0\). This means that the two characteristic fields are neither genuinely nonlinear nor linearly degenerate. The consequences of this are unclear to the authors and might require further investigations. See LeFloch (2002) for details. The Generalized Riemann Invariants (GRIs) for \(\lambda _1\) and \(\lambda _2\) characteristic fields are, respectively,

In the present work, the generalized Riemann invariants will be used to couple valves with lymphangions and to impose the pressure at the terminal interfaces of the collector.
B Numerical methods
Here, we briefly describe the finite volume schemes used for the one-dimensional lymph flow equations, explain how lymphatic valves and lymphangions are coupled, and illustrate the treatment of the boundary conditions at the terminal interfaces of the lymphangion. Then, we summarize the numerical methods used for the valves and the EFMC models.
1.1 B.1 A finite volume method for the one-dimensional model
Consider the system of m hyperbolic balance laws
By integrating (58) over the control volume \(V=[x_{i-\frac{1}{2}},x_{i+\frac{1}{2}}]\times [t^n,t^{n+1}]\), we obtain the exact formula
with definitions


Eq. (60) gives the spatial–integral average at time \(t=t^n\) of the conserved variable \(\mathbf {Q}\) while Eqs. (60) give the time-integral average at interface \(x=x_{i+\frac{1}{2}}\) of the physical flux \(\mathbf {F}\) and the volume-integral average in V of the source term \(\mathbf {S}\). Spatial mesh size and time step are \(\varDelta x=x_{i+\frac{1}{2}}-x_{i-\frac{1}{2}}\) and \(\varDelta t=t^{n+1}-t^n\), respectively. Finite volume methods for (58) depart from (59) to (60), where integrals are approximated, and then formula (59) becomes a finite volume method, where the approximated integrals in (60) are called numerical flux and numerical source, respectively. Here, index i runs from 1 to M, where the cell \(i=1\) is the leftmost cell with \(x_{\frac{1}{2}}\) being the first interface, and the cell \(i=M\) is the rightmost cell with \(x_{M+\frac{1}{2}}\) being the last interface. See Fig. 13 for an illustration of the finite volume framework. To compute the time step \(\varDelta t\), the Courant–Friedrichs–Lewy condition is applied for each lymphangion
with \(CFL=0.9\). Superindex j indicates the j-th lymphangion. Then, the time step \(\varDelta t\) to be used is the minimum of all the time steps, namely \(\varDelta t=\min \limits _{j}\left( \varDelta t^j\right) \).
In the present paper, we used the SLIC method to evaluate the numerical fluxes within the domain (\(\mathbf {F}_{\frac{3}{2}},\dots , \mathbf {F}_{M-\frac{1}{2}}\)) (Toro and Billett 2000). This method is second order, accurate in space and time and is based on the MUSCL-Hancock scheme where the Godunov upwind flux is replaced by the FORCE flux; see Section 14.5.3 of Toro (2009) and references therein. The numerical source was approximated using a second order in space and time method; see Chapter 19 of Toro (2009). For the numerical fluxes at the boundaries (\(\mathbf {F}_{\frac{1}{2}}\) and \(\mathbf {F}_{M+\frac{1}{2}}\)), we used a first-order Godunov-type method based on the solution of a classical Riemann problem at the interface.
1.2 B.2 Coupling between valves and lymphangions
Here, we aim to couple valves and lymphangions. For each lymphangion, we need to calculate the numerical flux at the interface in which the valve is located, which can be either \(\mathbf {F}_{\frac{1}{2}}\) or \(\mathbf {F}_{M+\frac{1}{2}}\) according to Fig. 13. There are three possible modelling configurations for a lymphatic valve. It can be the leftmost or rightmost valve of a collector, or it can be interposed between two lymphangions. In every case, the flow across the lymphatic valve is calculated from (45), where the pressure difference \(\varDelta p\) in (39) is evaluated at the current time \(t^n\) using either of the two lymphangions, or one of the lymphangions and a prescribed time-varying pressure. Specifically, at \(t=t^n\) the pressure difference \(\varDelta p(t^n)\) is
where values \(p_u(t^n)\) and \(p_d(t^n)\) are

and

where pressures \(p_{M}^n\) and \(p_1^n\) refer to the upstream and downstream lymphangions, respectively, and \(P_\mathrm{in}\) and \(P_\mathrm{out}\) are prescribed functions of time. The three possible configurations are summarized here

Once we numerically solve system (45), the flow across the valve at the future time \(q_v^{n+1}\) is determined.
In the present paper, to find \(A^*\) and calculate the numerical flux at the boundary, we follow the numerical methodology proposed by Alastruey et al. (2008). This method has already been used in Müller and Toro (2014), Contarino et al. (2016). To find \(A^*\), we solve the following nonlinear algebraic equation based on the Riemann invariant
using the Newton-Raphson iterative method. \(A^n\) and \(u^n\) are the cross-sectional area and the velocity at the cell adjacent to the boundary at current time \(t=t^n\), \(q_v^{n+1}\) is the known flow rate across the valve, and

Then, the numerical flux at the boundary is
where
As shown in Fig. 14, when a valve is interposed between two lymphangions, then the nonlinear problem (67) has to be solved twice: one for the upstream lymphangion (\(\beta =1\)) and one for the downstream lymphangion (\(\beta =-1\)).
1.3 B.3 Imposed pressure at boundaries
The numerical procedure to impose a pressure in one of the extremities of a lymphatic vessel is similar to the coupling method for valves and lymphangions. Consider a time-varying pressure \(p_{I}\left( t\right) \) at a terminal interface. From pressure \(p_I\left( t\right) \), cross-sectional area \(A_{I}\left( t\right) \) can be calculated by using the inverse of the tube law (2). The flow rate \(q^*\) can be found by applying the Riemann invariants as described in B.2, and in this case it can be explicitly calculated as
where \(A^n\), \(u^n\), and \(\beta \) are the cross-sectional area and the velocity at the cell adjacent to the boundary at current time \(t=t^n\) and \(\beta \) is given by Eq. (68). As before, the numerical flux at the boundary is given by (69) with
1.4 B.4 Numerical method for the systems of ODEs
The systems of ODEs (45) and (17) were numerically solved with a second-order implicit Runge–Kutta method using the Lobatto IIIC method. The Butcher tableau is

In the next section, we present the coupling of the systems of PDEs and ODEs, through an algorithm description.
1.5 B.5 Complete algorithm
Here, we provide the complete algorithm to update the solution from time \(t^n\) to time \(t^{n+1}=t^n+\varDelta t\). When not specified, the initial conditions are: \(p(x,0)=P_\mathrm{in}(0)\), \(u(x,0)=0\), \(v(0)=0.1\), \(w(0)=s(0)=I(0)=0\), and \(q_v(0)=\xi (0)=0\).
-
1.
Assume data for all variables at \(t=t^n\).
-
2.
Calculate the time step \(\varDelta t\) as explained in Section B.1.
-
3.
Evolve the valve flow q and valve state \(\xi \) of each lymphatic valve from time \(t^n\) to \(t^{n+1}\) by applying a second-order implicit Runge–Kutta method to the system of ODEs (45) and assuming the pressure difference \(\varDelta p\) at time \(t^n\).
-
4.
Calculate the numerical fluxes at the boundaries \(\mathbf {F}_{\frac{1}{2}}\) and \(\mathbf {F}_{M+\frac{1}{2}}\) of each lymphangion, as described in Sections B.2 and B.3, using the lymphatic valve flow rates at time \(t^{n+1}\).
-
5.
Using the contraction state s at the current time \(t^n\), calculate the numerical fluxes \(\mathbf {F}_{i+\frac{1}{2}}\) within each domain of the lymphangions using the SLIC method (Section 14.5.3 of Toro (2009)).
-
6.
Using the contraction state s at the current time \(t^n\), calculate the numerical sources \(\mathbf {S}_{i}\) within each domain of the lymphangions using a second-order method in space and time (Chapter 19 of Toro (2009)).
-
7.
Update the conserved variables \(\mathbf {Q}\) of the PDEs of each lymphangion from time \(t^n\) to \(t^{n+1}\) according to finite volume formula (59).
-
8.
Evolve the variables of the EFMC model of each lymphangion from time \(t^n\) to \(t^{n+1}\) by applying a second-order implicit Runge–Kutta method to the system of ODEs (17) and using the space–time-averaged cross-sectional area and WSS at time \(t^{n+1}\).
The EFMC model and the system of PDEs are coupled through the contraction state s. The variable s gives the actual value of the coefficient K(t) in Eq. (5) to be used to calculate the physical flux in Eq. (12). Observe that even though we use second-order methods for every model, the accuracy of the global algorithm is formally of order one. This is caused by the coupling methods. As a matter of fact, we couple the set of ODEs and PDEs using only a first-order method. There are more sophisticated high-order coupling methods in the literature; see, for instance, Borsche and Kall (2016).
C Sensitivity Analysis
The method is divided into a local and global analysis. In the local analysis, we calculated N local sensitivity matrices \(S_{i,j}^k\), for \(k=1,\dots ,N\), as follows: starting from the reference value in Table 1, we randomly varied each parameter from \(70\%\) to \(130\% \) and obtained a new set of parameters. Here, the baseline value for \(k_{NO}\) was set to 0.5. With this varied set of parameters, we calculated the local sensitivity matrix as follows:
where \(\mathbf {X}=\left( x_1,x_2,\dots ,x_m\right) \) is the vector of the varied model parameters, \(\mathbf {P}=\left( P_1,P_2,\dots ,P_n\right) \) is the vector of the lymphatic indices, and \(\mathbf {S}^k=\left( S_{i,j}^k\right) _{i,j}\) is local sensitivity matrix. The value \(S_{i,j}^k\) represents the non-dimensional relative change in \(P_j\) to the relative change in parameter \(x_j\), expressed as a percentage. If the model parameter \(x_i\) does not influence index \(P_j\), then \(S_{i,j}^k\) will be zero. Vice versa, if there is a significant influence of \(x_i\) on \(P_j\), then the absolute value of \(S_{i,j}^k\) will be greater than zero. For instance, if \(1\%\) change in \(x_i\) leads to \(1\%\) change in \(P_j\), then \(S_{i,j}^k\) is \(100\%\). A positive sign of \(S_{i,j}^k\) indicates that an increase of parameter \(x_i\) induces an increase of index \(P_j\). Vice versa, a negative sign of \(S_{i,j}^k\) indicates that an increase of parameter \(x_i\) induces a decrease of index \(P_j\).
Subsequently, in the global analysis, we performed a statistical analysis of \(S_{i,j}^k\) by calculating its mean \(\bar{S}_{i,j}\) and its standard deviation \(\sigma _{i,j}\). A large standard deviation \(\sigma _{i,j}\) indicates a strong correlation of the studied parameter with the remaining parameters in determining the sensitivity index. To calculate \(\bar{S}_{i,j}\) and \(\sigma _{i,j}\), we removed possible outliers by discarding the data below the third percentile and above the 97th percentile.
The partial derivative in Eq. (73) was approximated using a second-order finite difference method based on a percentage change of the parameter as follows:
where \(\mathbf {X}^{i,\epsilon _{\pm }}=\left( x_1,\dots ,x_i\left( 1\pm \epsilon \right) ,\dots ,x_m\right) .\) The parameter \(\epsilon \) was chosen as \(\epsilon =0.05\). Compared to van Griensven et al. (2006), we did not construct a stratified sampling space, but rather a simple random variation in the considered range.
Rights and permissions
About this article
Cite this article
Contarino, C., Toro, E.F. A one-dimensional mathematical model of collecting lymphatics coupled with an electro-fluid-mechanical contraction model and valve dynamics. Biomech Model Mechanobiol 17, 1687–1714 (2018). https://doi.org/10.1007/s10237-018-1050-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-018-1050-7