Abstract
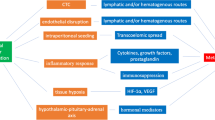
Surgery/anesthetic technique-stimulated immunosuppression in the perioperative period might cause an increase in cancer-related mortality. Whether anesthetic technique can affect the outcomes of cancer patients remains inconclusive. This review discusses data from the available literature on anesthetic techniques applied in oncologic surgery, the long-term outcomes of anesthetic technique, and their relation to survival and cancer recurrence. Searches of the PubMed database up to June 30, 2016, were conducted to identify publications with the terms “anesthetic technique and cancer recurrence,” “regional anesthesia and cancer recurrence,” “local anesthesia and cancer recurrence,” “anesthetic technique and immunosuppression,” and “anesthetic technique and oncologic surgery.” Surgery/anesthesia-stimulated activation of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS) provides immunosuppression through several soluble factors. Volatile anesthetics and opioids suppress cell-mediated immunity (CMI) and promote the proliferation of cancer cells and angiogenesis, whereas propofol does not suppress CMI and inhibits tumor angiogenesis. Regional anesthesia (RA) protects CMI and diminishes the surgical neuroendocrine stress response by blocking afferent neural transmission that stimulates the HPA axis and SNS, decreasing the requirement for opioids and volatile anesthetics and thereby decreasing cancer recurrence. Preclinical and retrospective studies highlight a potential benefit of anesthetic technique in reducing cancer-related mortality and recurrence by attenuating immunosuppression following surgical treatment in patients with specific types of cancer. Several well-planned, prospective, randomized controlled trials (RCTs) are underway that may provide more conclusive and definitive results regarding the benefits of anesthetic technique on survival in oncologic surgery.


Similar content being viewed by others
References
Heaney, A., & Buggy, D. J. (2012). Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis? British Journal of Anaesthesiology, 109(Suppl 1), i17–i28. doi:10.1093/bja/aes421.
Talmadge, J. E., & Fidler, I. J. (2010). AACR centennial series: the biology of cancer metastasis: historical perspective. Cancer Research, 70(14), 5649–5669. doi:10.1158/0008-5472.CAN-10-1040.
Alsina, E., Matute, E., Ruiz-Huerta, A. D., & Gilsanz, F. (2014). The effects of sevoflurane or remifentanil on the stress response to surgical stimulus. Current Pharmaceutical Design, 20(34), 5449–5468.
O’Dwyer, M. J., Owen, H. C., & Torrance, H. D. (2015). The perioperative immune response. Current Opinion in Critical Care, 21(4), 336–342. doi:10.1097/MCC.0000000000000213.
Bar-Yosef, S., Melamed, R., Page, G. G., Shakhar, G., Shakhar, K., & Ben-Eliyahu, S. (2001). Attenuation of the tumor-promoting effect of surgery by spinal blockade in rats. Anesthesiology, 94(6), 1066–1073.
Melamed, R., Bar-Yosef, S., Shakhar, G., Shakhar, K., & Ben-Eliyahu, S. (2003). Suppression of natural killer cell activity and promotion of tumor metastasis by ketamine, thiopental, and halothane, but not by propofol: mediating mechanisms and prophylactic measures. Anesthesiaa & Analgesia, 97(5), 1331–1339.
Snyder, G. L., & Greenberg, S. (2010). Effect of anaesthetic technique and other perioperative factors on cancer recurrence. British Journal Anaesthesiology, 105(2), 106–115. doi:10.1093/bja/aeq164.
Green, J. S., & Tsui, B. C. (2013). Impact of anesthesia for cancer surgery: continuing professional development. Canadian Journal Anaesthesia, 60(12), 1248–1269. doi:10.1007/s12630-013-0037-1.
Ash, S. A., & Buggy, D. J. (2013). Does regional anaesthesia and analgesia or opioid analgesia influence recurrence after primary cancer surgery? An update of available evidence. Best Practice & Research Clinical Anaesthesiology, 27(4), 441–456. doi:10.1016/j.bpa.2013.10.005.
Cassinello, F., Prieto, I., del Olmo, M., Rivas, S., & Strichartz, G. R. (2015). Cancer surgery: how may anesthesia influence outcome? Journal of Clinical Anesthesia, 27(3), 262–272. doi:10.1016/j.jclinane.2015.02.007.
Votta-Velis, E. G., Piegeler, T., Minshall, R. D., Aguirre, J., Beck-Schimmer, B., Schwartz, D. E., et al. (2013). Regional anaesthesia and cancer metastases: the implication of local anaesthetics. Acta Anaesthesiologica Scandinavica, 57(10), 1211–1229. doi:10.1111/aas.12210.
Byrne, K., Levins, K. J., & Buggy, D. J. (2016). Can anesthetic-analgesic technique during primary cancer surgery affect recurrence or metastasis? Canadian Journal Anaesthesia, 63(2), 184–192.
Meserve, J. R., Kaye, A. D., Prabhakar, A., & Urman, R. D. (2014). The role of analgesics in cancer propagation. Best Practice & Research Clinical Anaesthesiology, 28(2), 139–151. doi:10.1016/j.bpa.2014.04.004.
Bajwa, S. J., Anand, S., & Kaur, G. (2015). Anesthesia and cancer recurrences: the current knowledge and evidence. Journal Cancer Research and Therapeutics, 11(3), 528–534. doi:10.4103/0973-1482.157321.
Xuan, W., Hankin, J., Zhao, H., Yao, S., & Ma, D. (2015). The potential benefits of the use of regional anesthesia in cancer patients. International Journal of Cancer, 137(12), 2774–2784. doi:10.1002/ijc.29306.
Kim, R., Emi, M., Tanabe, K., & Arihiro, K. (2006). Tumor-driven evolution of immunosuppressive networks during malignant progression. Cancer Research, 66(11), 5527–5536.
Kavanagh, T., & Buggy, D. J. (2012). Can anaesthetic technique effect postoperative outcome? Current Opinion in Anaesthesiology, 25(2), 185–198. doi:10.1097/ACO.0b013e32834f6c4c.
Kurosawa, S., & Kato, M. (2008). Anesthetics, immune cells, and immune responses. Journal of Anesthesia, 22(3), 263–277. doi:10.1007/s00540-008-0626-2.
Lee, B. M., & Cata, J. P. (2015). Impact of anesthesia on cancer recurrence. Revista Española de Anestesiología y Reanimación, 62(10), 570–575. doi:10.1016/j.redar.2015.04.003.
Greenfeld, K., Avraham, R., Benish, M., Goldfarb, Y., Rosenne, E., Shapira, Y., et al. (2007). Immune suppression while awaiting surgery and following it: dissociations between plasma cytokine levels, their induced production, and NK cell cytotoxicity. Brain, Behavior, and Immunity, 21(4), 503–513.
Sood, A. K., Bhatty, R., Kamat, A. A., Landen, C. N., Han, L., Thaker, P. H., et al. (2006). Stress hormone-mediated invasion of ovarian cancer cells. Clinical Cancer Research, 12(2), 369–375.
Wong, H. P., Ho, J. W., Koo, M. W., Yu, L., Wu, W. K., Lam, E. K., et al. (2011). Effects of adrenaline in human colon adenocarcinoma HT-29 cells. Life Sciences, 88(25–26), 1108–1112. doi:10.1016/j.lfs.2011.04.007.
Bernabé, D. G., Tamae, A. C., Biasoli, É. R., & Oliveira, S. H. (2011). Stress hormones increase cell proliferation and regulates interleukin-6 secretion in human oral squamous cell carcinoma cells. Brain, Behavior, and Immunity, 25(3), 574–583. doi:10.1016/j.bbi.2010.12.012.
Yang, E. V., Kim, S. J., Donovan, E. L., Chen, M., Gross, A. C., Webster Marketon, J. I., et al. (2009). Norepinephrine upregulates VEGF, IL-8, and IL-6 expression in human melanoma tumor cell lines: implications for stress-related enhancement of tumor progression. Brain, Behavior, and Immunity, 23(2), 267–275. doi:10.1016/j.bbi.2008.10.005.
Calcagni, E., & Elenkov, I. (2006). Stress system activity, innate and T helper cytokines, and susceptibility to immune-related diseases. Annals of the New York Academy of Sciences, 1069, 62–76.
Marik, P. E., & Flemmer, M. (2012). Immunonutrition in the surgical patient. See comment in PubMed Commons below Minerva Anestesiologica, 78(3), 336–342.
Sica, A., Schioppa, T., Mantovani, A., & Allavena, P. (2006). Tumour-associated macrophages are a distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eurlopian Journal of Cancer, 42(6), 717–727.
Obermajer, N., Wong, J. L., Edwards, R. P., Odunsi, K., Moysich, K., & Kalinski, P. (2012). PGE2-driven induction and maintenance of cancer-associated myeloid-derived suppressor cells. Immunological Investigations, 41(6–7), 635–657. doi:10.3109/08820139.2012.695417.
Mao, Y., Sarhan, D., Steven, A., Seliger, B., Kiessling, R., & Lundqvist, A. (2014). Inhibition of tumor-derived prostaglandin-E2 blocks the induction of myeloid-derived suppressor cells and recovers natural killer cell activity. Clinical Cancer Research, 20(15), 4096–4106. doi:10.1158/1078-0432.CCR-14-0635.
Kitamura, T., Qian, B. Z., & Pollard, J. W. (2015). Immune cell promotion of metastasis. Nature Reviews Immunology, 15(2), 73–86. doi:10.1038/nri3789.
John, A., & Tuszynski, G. (2001). The role of matrix metalloproteinases in tumor angiogenesis and tumor metastasis. Pathology & Oncology Research, 7(1), 14–23.
Zappalà, G., McDonald, P. G., & Cole, S. W. (2013). Tumor dormancy and the neuroendocrine system: an undisclosed connection? Cancer and Metastasis Reviews, 32(1–2), 189–200. doi:10.1007/s10555-012-9400-x.
Folkman, J. (2002). Role of angiogenesis in tumor growth and metastasis. Seminars in Oncology, 29(6 Suppl 16), 15–18.
Exadaktylos, A. K., Buggy, D. J., Moriarty, D. C., Mascha, E., & Sessler, D. I. (2006). Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology, 105(4), 660–664.
Koonce, S. L., Mclaughlin, S. A., Eck, D. L., Porter, S., Bagaria, S., Clendenen, S. R., et al. (2014). Breast cancer recurrence in patients receiving epidural and paravertebral anesthesia: a retrospective, case-control study. Middle East Journal of Anesthesiology, 22(6), 567–571.
Starnes-Ott, K., Goravanchi, F., & Meininger, J. C. (2015). Anesthetic choices and breast cancer recurrence: a retrospective pilot study of patient, disease, and treatment factors. Critical Care Nursing Quarterly, 38(2), 200–210. doi:10.1097/CNQ.0000000000000062.
Tsigonis, A. M., Al-Hamadani, M., Linebarger, J. H., Vang, C. A., Krause, F. J., Johnson, J. M., et al. (2016). Are cure rates for breast cancer improved by local and regional anesthesia? Regional Anesthesia and Pain Medicine, 41(3), 339–347. doi:10.1097/AAP.0000000000000379.
Kairaluoma, P., Mattson, J., Heikkilä, P., Pere, P., & Leidenius, M. (2016). Perioperative paravertebral regional anaesthesia and breast cancer recurrence. Anticancer Research, 36(1), 415–418.
Lin, L., Liu, C., Tan, H., Ouyang, H., Zhang, Y., & Zeng, W. (2011). Anaesthetic technique may affect prognosis for ovarian serous adenocarcinoma: a retrospective analysis. British Journal of Anaesthesia, 106, 814–822. doi:10.1093/bja/aer055.
de Oliveira Jr., G. S., Ahmad, S., Schink, J. C., Singh, D. K., Fitzgerald, P. C., & McCarthy, R. J. (2011). Intraoperative neuraxial anesthesia but not postoperative neuraxial analgesia is associated with increased relapse-free survival in ovarian cancer patients after primary cytoreductive surgery. Regional Anesthesia and Pain Medicine, 36, 271–277. doi:10.1097/AAP.0b013e318217aada.
Capmas, P., Billard, V., Gouy, S., Lhommé, C., Pautier, P., Morice, P., et al. (2012). Impact of epidural analgesia on survival in patients undergoing complete cytoreductive surgery for ovarian cancer. Anticancer Research, 32(4), 1537–1542.
Elias, K. M., Kang, S., Liu, X., Horowitz, N. S., Berkowitz, R. S., & Frendl, G. (2015). Anesthetic selection and disease-free survival following optimal primary cytoreductive surgery for stage III epithelial ovarian cancer. Annals of Surgical Oncology, 22(4), 1341–1348. doi:10.1245/s10434-014-4112-9.
Lacassie, H. J., Cartagena, J., Brañes, J., Assel, M., & Echevarría, G. C. (2013). The relationship between neuraxial anesthesia and advanced ovarian cancer-related outcomes in the Chilean population. Anesthesia & Analgesia, 117(3), 653–660. doi:10.1213/ANE.0b013e3182a07046.
Christopherson, R., James, K. E., Tableman, M., Marshall, P., & Johnson, F. E. (2008). Long-term survival after colon cancer surgery: a variation associated with choice of anesthesia. Anesthesia & Analgesia, 107(1), 325–332. doi:10.1213/ane.0b013e3181770f55.
Holler, J. P., Ahlbrandt, J., Burkhardt, E., Gruss, M., Röhrig, R., Knapheide, J., et al. (2013). Peridural analgesia may affect long-term survival in patients with colorectal cancer after surgery (PACO-RAS-Study): an analysis of a cancer registry. Annals of Surgery, 258(6), 989–993. doi:10.1097/SLA.0b013e3182915f61.
Vogelaar, F. J., Abegg, R., van der Linden, J. C., Cornelisse, H. G., van Dorsten, F. R., Lemmens, V. E., et al. (2015). Epidural analgesia associated with better survival in colon cancer. International Journal of Colorectal Disease, 30(8), 1103–1107. doi:10.1007/s00384-015-2224-8.
Zimmitti, G., Soliz, J., Aloia, T. A., Gottumukkala, V., Cata, J. P., Tzeng, C. W., et al. (2016). Positive impact of epidural analgesia on oncologic outcomes in patients undergoing resection of colorectal liver metastases. Annals of Surgical Oncology, 23(3), 1003–1011. doi:10.1245/s10434-015-4933-1.
Gupta, A., Björnsson, A., Fredriksson, M., Hallböök, O., & Eintrei, C. (2011). Reduction in mortality after epidural anaesthesia and analgesia in patients undergoing rectal but not colonic cancer surgery: a retrospective analysis of data from 655 patients in central Sweden. British Journal of Anaesthesia, 107(2), 164–170. doi:10.1093/bja/aer100.
Cummings 3rd, K. C., Xu, F., Cummings, L. C., & Cooper, G. S. (2012). A comparison of epidural analgesia and traditional pain management effects on survival and cancer recurrence after colectomy: a population-based study. Anesthesiology, 116(4), 797–806. doi:10.1097/ALN.0b013e31824674f6.
Gottschalk, A., Ford, J. G., Regelin, C. C., You, J., Mascha, E. J., Sessler, D. I., et al. (2010). Association between epidural analgesia and cancer recurrence after colorectal cancer surgery. Anesthesiology, 113(1), 27–34. doi:10.1097/ALN.0b013e3181de6d0d.
Day, A., Smith, R., Jourdan, I., Fawcett, W., Scott, M., & Rockall, T. (2012). Retrospective analysis of the effect of postoperative analgesia on survival in patients after laparoscopic resection of colorectal cancer. British Journal of Anaesthesia, 109(2), 185–190. doi:10.1093/bja/aes106.
Merquiol, F., Montelimard, A. S., Nourissat, A., Molliex, S., & Zufferey, P. J. (2013). Cervical epidural anesthesia is associated with increased cancer-free survival in laryngeal and hypopharyngeal cancer surgery: a retrospective propensity-matched analysis. Regional Anesthesia and Pain Medicine, 38(5), 398–402. doi:10.1097/AAP.0b013e31829cc3fb.
Call, T. R., Pace, N. L., Thorup, D. B., Maxfield, D., Chortkoff, B., Christensen, J., et al. (2015). Factors associated with improved survival after resection of pancreatic adenocarcinoma: a multivariable model. Anesthesiology, 122(2), 317–324. doi:10.1097/ALN.0000000000000489.
Hiller, J. G., Hacking, M. B., Link, E. K., Wessels, K. L., & Riedel, B. J. (2014). Perioperative epidural analgesia reduces cancer recurrence after gastro-oesophageal surgery. Acta Anaesthesiologica Scandinavica, 58(3), 281–290. doi:10.1111/aas.12255.
Cao, L., Chang, Y., Lin, W., Zhou, J., Tan, H., Yuan, Y., et al. (2014). Long-term survival after resection of hepatocelluar carcinoma: a potential risk associated with the choice of postoperative analgesia. Anesthesia & Analgesia, 118(6), 1309–1316. doi:10.1213/ANE.0000000000000207.
Cummings 3rd, K. C., Patel, M., Htoo, P. T., Bakaki, P. M., Cummings, L. C., & Koroukian, S. (2014). A comparison of the effects of epidural analgesia versus traditional pain management on outcomes after gastric cancer resection: a population-based study. Regional Anesthesia and Pain Medicine, 39(3), 200–207. doi:10.1097/AAP.0000000000000079.
Heinrich, S., Janitz, K., Merkel, S., Klein, P., & Schmidt, J. (2015). Short- and long term effects of epidural analgesia on morbidity and mortality of esophageal cancer surgery. Langenbeck’s Archives of Surgery, 400(1), 19–26. doi:10.1007/s00423-014-1248-9.
Biki, B., Mascha, E., Moriarty, D. C., Fitzpatrick, J. M., Sessler, D. I., & Buggy, D. J. (2008). Anesthetic technique for radical prostatectomy surgery affects cancer recurrence: a retrospective analysis. Anesthesiology, 109, 180–187. doi:10.1097/ALN.0b013e31817f5b73.
Wuethrich, P. Y., Hsu Schmitz, S. F., Kessler, T. M., Thalmann, G. N., Studer, U. E., Stueber, F., et al. (2010). Potential influence of the anesthetic technique used during open radical prostatectomy on prostate cancer-related outcome: a retrospective study. Anesthesiology, 113(3), 570–576. doi:10.1097/ALN.0b013e3181e4f6ec.
Tsui, B. C., Rashiq, S., Schopflocher, D., Murtha, A., Broemling, S., Pillay, J., et al. (2010). Epidural anesthesia and cancer recurrence rates after radical prostatectomy. Canadian Journal of Anesthesia, 57(2), 107–112. doi:10.1007/s12630-009-9214-7.
Forget, P., Tombal, B., Scholtès, J. L., Nzimbala, J., Meulders, C., Legrand, C., et al. (2011). Do intraoperative analgesics influence oncological outcomes after radical prostatectomy for prostate cancer? European Journal of Anaesthesiology, 28(12), 830–835. doi:10.1097/EJA.0b013e32834b7d9a.
Wuethrich, P. Y., Thalmann, G. N., Studer, U. E., & Burkhard, F. C. (2013). Epidural analgesia during open radical prostatectomy does not improve long-term cancer-related outcome: a retrospective study in patients with advanced prostate cancer. PloS One, 8(8), e72873. doi:10.1371/journal.pone.0072873.
Sprung, J., Scavonetto, F., Yeoh, T. Y., Kramer, J. M., Karnes, R. J., Eisenach, J. H., et al. (2014). Outcomes after radical prostatectomy for cancer: a comparison between general anesthesia and epidural anesthesia with fentanyl analgesia: a matched cohort study. Anesthesia & Analgesia, 119(4), 859–866. doi:10.1213/ANE.0000000000000320.
Roiss, M., Schiffmann, J., Tennstedt, P., Kessler, T., Blanc, I., Goetz, A., et al. (2014). Oncological long-term outcome of 4772 patients with prostate cancer undergoing radical prostatectomy: does the anaesthetic technique matter? European Journal of Surgical Oncology, 40(12), 1686–1692. doi:10.1016/j.ejso.2014.02.223.
Scavonetto, F., Yeoh, T. Y., Umbreit, E. C., Weingarten, T. N., Gettman, M. T., Frank, I., et al. (2014). Association between neuraxial analgesia, cancer progression, and mortality after radical prostatectomy: a large, retrospective matched cohort study. British Journal of Anaesthesia, 113(Suppl 1), i95–102. doi:10.1093/bja/aet467.
Tseng, K. S., Kulkarni, S., Humphreys, E. B., Carter, H. B., Mostwin, J. L., Partin, A. W., et al. (2014). Spinal anesthesia does not impact prostate cancer recurrence in a cohort of men undergoing radical prostatectomy: an observational study. Regional Anesthesia and Pain Medicine, 39(4), 284–288. doi:10.1097/AAP.0000000000000108.
Ehdaie, B., Sjoberg, D. D., Dalecki, P. H., Scardino, P. T., Eastham, J. A., & Amar, D. (2014). Association of anesthesia technique for radical prostatectomy with biochemical recurrence: a retrospective cohort study. Canadian Journal of Anesthesia, 61(12), 1068–1074. doi:10.1007/s12630-014-0221-y.
Kamuf, J., Pospich, M., & Heid, F. (2014). Cancer-free or overall survival rate following radical prostatectomy is not influenced by perioperative pain management. Journal of Anesthesia & Clinical Research, 5, 7. doi:10.4172/2155-6148.1000422.
Jang, D., Lim, C. S., Shin, Y. S., Ko, Y. K., Park, S. I., Song, S. H., et al. (2016). A comparison of regional and general anesthesia effects on 5 year survival and cancer recurrence after transurethral resection of the bladder tumor: a retrospective analysis. BMC Anesthesiology, 16, 16. doi:10.1186/s12871-016-0181-6.
Weingarten, T. N., Taccolini, A. M., Ahle, S. T., Dietz, K. R., Dowd, S. S., Frank, I., et al. (2016). Perioperative management and oncological outcomes following radical cystectomy for bladder cancer: a matched retrospective cohort study. Canadian Journal of Anesthesia, 63(5), 584–595. doi:10.1007/s12630-016-0599-9.
Cata, J. P., Gottumukkala, V., Thakar, D., Keerty, D., Gebhardt, R., & Liu, D. D. (2014). Effects of postoperative epidural analgesia on recurrence-free and overall survival in patients with nonsmall cell lung cancer. See comment in PubMed Commons below Journal of Clinical Anesthesia, 26(1), 3–17. doi:10.1016/j.jclinane.2013.06.007.
Maher, D. P., Wong, W., White, P. F., McKenna Jr., R., Rosner, H., Shamloo, B., et al. (2014). Association of increased postoperative opioid administration with non-small-cell lung cancer recurrence: a retrospective analysis. British Journal of Anaesthesia, 113(Suppl 1), i88–i94. doi:10.1093/bja/aeu192.
Myles, P. S., Peyton, P., Silbert, B., Hunt, J., Rigg, J. R., Sessler, D. I., & ANZCA Trials Group Investigators (2011). Perioperative epidural analgesia for major abdominal surgery for cancer and recurrence-free survival: randomised trial. British Medical Journal, 342, d1491. doi:10.1136/bmj.d1491.
Binczak, M., Tournay, E., Billard, V., Rey, A., & Jayr, C. (2013). Major abdominal surgery for cancer: does epidural analgesia have a long-term effect on recurrence-free and overall survival? Annales Françaises d’Anesthésie et de Réanimation, 32(5), e81–e88. doi:10.1016/j.annfar.2013.02.027.
Schlagenhauff, B., Ellwanger, U., Breuninger, H., Stroebel, W., Rassner, G., & Garbe, C. (2000). Prognostic impact of the type of anaesthesia used during the excision of primary cutaneous melanoma. Melanoma Research, 10(2), 165–169.
Gottschalk, A., Brodner, G., Van Aken, H. K., Ellger, B., Althaus, S., & Schulze, H. J. (2012). Can regional anaesthesia for lymph-node dissection improve the prognosis in malignant melanoma? British Journal of Anaesthesia, 109(2), 253–259. doi:10.1093/bja/aes176.
Chen, W. K., & Miao, C. H. (2013). The effect of anesthetic technique on survival in human cancers: a meta-analysis of retrospective and prospective studies. PloS One, 8(2), e56540. doi:10.1371/journal.pone.0056540.
Cakmakkaya, O. S., Kolodzie, K., Apfel, C. C., & Pace, N. L. (2014). Anaesthetic techniques for risk of malignant tumour recurrence. Cochrane Database of Systematic Reviews, 11, CD008877. doi:10.1002/14651858.CD008877.pub2.
Pei, L., Tan, G., Wang, L., Guo, W., Xiao, B., Gao, X., et al. (2014). Comparison of combined general-epidural anesthesia with general anesthesia effects on survival and cancer recurrence: a meta-analysis of retrospective and prospective studies. PloS One, 9(12), e114667. doi:10.1371/journal.pone.0114667.
Sun, Y., Li, T., & Gan, T. J. (2015). The effects of perioperative regional anesthesia and analgesia on cancer recurrence and survival after oncology surgery: a systematic review and meta-analysis. Regional Anesthesia and Pain Medicine, 40(5), 589–598. doi:10.1097/AAP.0000000000000273.
Sun, X., Yang, C., Li, K., & Ding, S. (2015). The impact of anesthetic techniques on survival for patients with colorectal cancer: evidence based on six studies. Hepato-Gastroenterology, 62(138), 299–302.
Lee, B. M., Singh Ghotra, V., Karam, J. A., Hernandez, M., Pratt, G., & Cata, J. P. (2015). Regional anesthesia/analgesia and the risk of cancer recurrence and mortality after prostatectomy: a meta-analysis. Pain Management, 5(5), 387–595. doi:10.2217/pmt.15.30.
Weng, M., Chen, W., Hou, W., Li, L., Ding, M., & Miao, C. (2016). The effect of neuraxial anesthesia on cancer recurrence and survival after cancer surgery: an updated meta-analysis. Oncotarget, 7(12), 15262–15273. doi:10.18632/oncotarget.7683.
Enlund, M., Berglund, A., Andreasson, K., Cicek, C., Enlund, A., & Bergkvist, L. (2014). The choice of anaesthetic—sevoflurane or propofol—and outcome from cancer surgery: a retrospective analysis. Upsala Journal of Medical Sciences, 119(3), 251–261. doi:10.3109/03009734.2014.922649.
Lee, J. H., Kang, S. H., Kim, Y., Kim, H. A., & Kim, B. S. (2016). Effects of propofol-based total intravenous anesthesia on recurrence and overall survival in patients after modified radical mastectomy: a retrospective study. Korean Journal of Anesthesiology, 69(2), 126–132. doi:10.4097/kjae.2016.69.2.126.
Wigmore, T. J., Mohammed, K., & Jhanji, S. (2016). Long-term survival for patients undergoing volatile versus IV anesthesia for cancer surgery: a retrospective analysis. Anesthesiology, 124(1), 69–79. doi:10.1097/ALN.0000000000000936.
Sessler, D. I., Ben-Eliyahu, S., Mascha, E. J., Parat, M. O., & Buggy, D. J. (2008). Can regional analgesia reduce the risk of recurrence after breast cancer? Methodology of a multicenter randomized trial. Contemporary Clinical Trials, 29(4), 517–526. doi:10.1016/j.cct.2008.01.002.
Zetter, B. R. (1998). Angiogenesis and tumor metastasis. Annual Review of Medicine, 49, 407–424.
Antoni, M. H., Lutgendorf, S. K., Cole, S. W., Dhabhar, F. S., Sephton, S. E., McDonald, P. G., et al. (2006). The influence of bio-behavioural factors on tumour biology: pathways and mechanisms. Nature Reviews Cancer, 6(3), 240–248.
Kurosawa, S. (2012). Anesthesia in patients with cancer disorders. Current Opinion in Anesthesiology, 25(3), 376–384. doi:10.1097/ACO.0b013e328352b4a8.
Sacerdote, P., Bianchi, M., Gaspani, L., Manfredi, B., Maucione, A., Terno, G., et al. (2000). The effects of tramadol and morphine on immune responses and pain after surgery in cancer patients. Anesthesia & Analgesia, 90(6), 1411–1414.
Ben-Eliyahu, S., Page, G. G., Yirmiya, R., & Shakhar, G. (1999). Evidence that stress and surgical interventions promote tumor development by suppressing natural killer cell activity. International Journal of Cancer, 80(6), 880–888.
Chae, B. K., Lee, H. W., Sun, K., Choi, Y. H., & Kim, H. M. (1998). The effect of combined epidural and light general anesthesia on stress hormones in open heart surgery patients. Surgery Today, 28(7), 727–731.
Gupta, K., Kshirsagar, S., Chang, L., Schwartz, R., Law, P. Y., Yee, D., et al. (2002). Morphine stimulates angiogenesis by activating proangiogenic and survival-promoting signaling and promotes breast tumor growth. Cancer Research, 62(15), 4491–4498.
Singhal, P. C., Sharma, P., Kapasi, A. A., Reddy, K., Franki, N., & Gibbons, N. (1998). Morphine enhances macrophage apoptosis. Journal of Immunology, 160(4), 1886–1893.
Hatzoglou, A., Bakogeorgou, E., & Castanas, E. (1996). The antiproliferative effect of opioid receptor agonists on the T47D human breast cancer cell line, is partially mediated through opioid receptors. European Journal of Pharmacology, 296(2), 199–207.
Lin, X., Wang, Y. J., Li, Q., Hou, Y. Y., Hong, M. H., Cao, Y. L., et al. (2009). Chronic high-dose morphine treatment promotes SH-SY5Y cell apoptosis via c-Jun N-terminal kinase-mediated activation of mitochondria-dependent pathway. Federation of European Biochemical Societies Journal, 276(7), 2022–2036. doi:10.1111/j.1742-4658.2009.06938.x.
Singleton, P. A., Mirzapoiazova, T., Hasina, R., Salgia, R., & Moss, J. (2014). Increased μ-opioid receptor expression in metastatic lung cancer. British Journal of Anaesthesia, 113(Suppl 1), i103–i108. doi:10.1093/bja/aeu165.
Bimonte, S., Barbieri, A., Rea, D., Palma, G., Luciano, A., Cuomo, A., et al. (2015). Morphine promotes tumor angiogenesis and increases breast cancer progression. BioMed Research International, 2015, 161508. doi:10.1155/2015/161508.
Page, G. G., Ben-Eliyahu, S., Yirmiya, R., & Liebeskind, J. C. (1993). Morphine attenuates surgery-induced enhancement of metastatic colonization in rats. Pain, 54(1), 21–28.
Page, G. G., McDonald, J. S., & Ben-Eliyahu, S. (1998). Pre-operative versus postoperative administration of morphine: impact on the neuroendocrine, behavioural, and metastatic-enhancing effects of surgery. British Journal of Anaesthesia, 81(2), 216–223.
Li, A. X., Xin, W. Q., & Ma, C. G. (2015). Fentanyl inhibits the invasion and migration of colorectal cancer cells via inhibiting the negative regulation of Ets-1 on BANCR. Biochemical and Biophysical Research Communications, 465(3), 594–600. doi:10.1016/j.bbrc.2015.08.068.
Juneja, R. (2014). Opioids and cancer recurrence. Current Opinion in Supportive and Palliative Care, 8(2), 91–101. doi:10.1097/SPC.0000000000000056.
Chen, W. K., Ren, L., Wei, Y., Zhu, D. X., Miao, C. H., & Xu, J. M. (2015). General anesthesia combined with epidural anesthesia ameliorates the effect of fast-track surgery by mitigating immunosuppression and facilitating intestinal functional recovery in colon cancer patients. International Journal of Colorectal Disease, 30(4), 475–481. doi:10.1007/s00384-014-2098-1.
Xu, Y. J., Chen, W. K., Zhu, Y., Wang, S. L., & Miao, C. H. (2014). Effect of thoracic epidural anaesthesia on serum vascular endothelial growth factor C and cytokines in patients undergoing anaesthesia and surgery for colon cancer. British Journal of Anaesthesia, 113(Suppl 1), i49–i55. doi:10.1093/bja/aeu148.
Xu, Y. J., Li, S. Y., Cheng, Q., Chen, W. K., Wang, S. L., Ren, Y., et al. (2016). Effects of anaesthesia on proliferation, invasion and apoptosis of LoVo colon cancer cells in vitro. Anaesthesia, 71(2), 147–154. doi:10.1111/anae.13331.
Sultan, S. S. (2013). Paravertebral block can attenuate cytokine response when it replaces general anesthesia for cancer breast surgeries. Saudi Journal of Anaesthesia, 7(4), 373–377. doi:10.4103/1658-354X.121043.
Desmond, F., McCormack, J., Mulligan, N., Stokes, M., & Buggy, D. J. (2015). Effect of anaesthetic technique on immune cell infiltration in breast cancer: a follow-up pilot analysis of a prospective, randomised, investigator-masked study. Anticancer Research, 35(3), 1311–1319.
Jaura, A. I., Flood, G., Gallagher, H. C., & Buggy, D. J. (2014). Differential effects of serum from patients administered distinct anaesthetic techniques on apoptosis in breast cancer cells in vitro: a pilot study. British Journal of Anaesthesia, 113(Suppl 1), i63–i67. doi:10.1093/bja/aet581.
Buckley, A., McQuaid, S., Johnson, P., & Buggy, D. J. (2014). Effect of anaesthetic technique on the natural killer cell anti-tumour activity of serum from women undergoing breast cancer surgery: a pilot study. See comment in PubMed Commons below British Journal of Anaesthesia, 113(Suppl 1), i56–i62. doi:10.1093/bja/aeu200.
Acknowledgements
I would like to thank Prof. Daniel I. Sessler, Department of Outcomes Research, Cleveland Clinic, for providing fruitful comments regarding the ongoing trial of NCT00418457. I also thank Accixx Biomedical Consulting (www.Accixx.com) for the scientific editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding support
There was no funding support for this manuscript.
Conflict of interest
The author declares that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, R. Anesthetic technique and cancer recurrence in oncologic surgery: unraveling the puzzle. Cancer Metastasis Rev 36, 159–177 (2017). https://doi.org/10.1007/s10555-016-9647-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-016-9647-8