Abstract
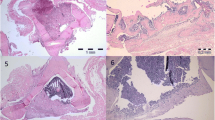
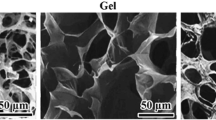
Fibrin-platelet glue (FPG) is a blood derivative, in which platelets and fibrinogen are concentrated in a small plasma volume, by differential centrifugation and precipitation. It can form a three-dimensional and biocompatible fibrin scaffold with a myriad of growth factors and proteins that are released progressively to the local environment and contribute to the accelerated postoperative bone healing. Gelatin (Gel) is a derivative of collagen and can promote cell adhesion and proliferation due to its unique sequence of amino acids, so it is suitable for bone tissue applications. This study examined the effects of Gel, FPG and their combinations as bone scaffold on the healing of surgically created critical-size defects in rat radius. Fifty critical size defects of 5 mm long were bilaterally created in the radial diaphysis of 25 rats. The animals were randomly divided into five equal groups as empty defect, autograft, Gel, FPG and Gel–FPG groups (n = 10 in each group). Radiographs of each forelimb were taken postoperatively on the 1st day and then at the 28th and 56th days post injury to evaluate bone formation, union and remodeling of the defect. After 56 days, the rats were euthanized and their harvested healing bone samples were evaluated by histopathology, scanning electron microscopy (SEM) and biomechanical testing. The results of present study showed that the Gel alone did not significantly affect bone healing and regeneration; however, the Gel treated defects promoted healing more than those that were left untreated (negative control). Furthermore, the FPG-enhanced grafts provided a good scaffold containing numerous growth factors for proliferation of osteoinduction and was effective in improving the structural and functional properties of the newly formed bone more than that of the untreated and also the Gel treated groups. Incorporation of Gel into the FPG scaffold improved healing potential of the FPG scaffold; however, it was still inferior to the autograft (positive control). Although the Gel–FPG scaffolds had best effectiveness during bone regeneration, it still needs to be further enhanced by incorporation of the ceramic and osteoinductive biomaterials.




Similar content being viewed by others
References
An YH, Freidman RJ (1998) Animal models in orthopaedic research. CRC Press, Boca Raton
Anitua E, Sánchez M, Nurden AT, Nurden P, Orive G, Andía I (2006) New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol 24:227–234
Bigham-Sadegh A, Oryan A, Mirshokraei P, Shadkhast M, Basiri E (2013) Bone tissue engineering with periosteal-free graft and pedicle omentum. ANZ J Surg 83:255–261
Burnouf T, Su CY, Radosevich M, Goubran H, El-Ekiaby M (2009) Blood-derived biomaterials: fibrin sealant, platelet gel and platelet fibrin glue. ISBT Sci Ser 4:136–142
Burnouf T, Goubran HA, Chen T-M, Ou K-L, El-Ekiaby M, Radosevic M (2013) Blood-derived biomaterials and platelet growth factors in regenerative medicine. Blood Rev 27:77–89
Butterfield KJ, Bennett J, Gronowicz G, Adams D (2005) Effect of platelet-rich plasma with autogenous bone graft for maxillary sinus augmentation in a rabbit model. J Oral Maxillofac Surg 63:370–376
Chen TM, Tsai J-C, Burnouf T (2008) Cranioplasty using osteoconductive scaffold and platelet glue. J Trauma Acute Care Surg 65:1321–1327
Emery SE, Brazinski MS, Koka A, Bensusan JS, Stevenson S (1994) The biological and biomechanical effects of irradiation on anterior spinal bone grafts in a canine model. J Bone Jt Surg Am 76:540–548
Findikcioglu K, Findikcioglu F, Yavuzer R, Elmas C, Atabay K (2009) Effect of platelet-rich plasma and fibrin glue on healing of critical-size calvarial bone defects. J Craniofac Surg 20:34–40
Fukui T, Ii M, Shoji T, Matsumoto T, Mifune Y, Kawakami Y, Akimaru H, Kawamoto A, Kuroda T, Saito T (2012) Therapeutic effect of local administration of low-dose simvastatin-conjugated gelatin hydrogel for fracture healing. J Bone Miner Res 27:1118–1131
Giovanini AF, Deliberador TM, Gonzaga CC, de Oliveira Filho MA, Göhringer I, Kuczera J, Zielak JC, de Andrade Urban C (2010) Platelet-rich plasma diminishes calvarial bone repair associated with alterations in collagen matrix composition and elevated CD34 + cell prevalence. Bone 46:1597–1603
Ito K, Yamada Y, Naiki T, Ueda M (2006) Simultaneous implant placement and bone regeneration around dental implants using tissue-engineered bone with fibrin glue, mesenchymal stem cells and platelet-rich plasma. Clin Oral Implant Res 17:579–586
Järvinen T, Sievänen H, Kannus P, Järvinen M (1998) Dual-energy X-ray absorptiometry in predicting mechanical characteristics of rat femur. Bone 22:551–558
Kakkar P, Verma S, Manjubala I, Madhan B (2014) Development of keratin–chitosan–gelatin composite scaffold for soft tissue engineering. Mater Sci Eng C 45:343–347
Khan MN, Islam JM, Khan MA (2012) Fabrication and characterization of gelatin-based biocompatible porous composite scaffold for bone tissue engineering. J Biomed Mater Res A 100:3020–3028
Lane JM, Sandhu H (1987) Current approaches to experimental bone grafting. Orthop Clin N Am 18:213–225
Lee H-J, Choi B-H, Jung J-H, Zhu S-J, Lee S-H, Huh J-Y, You T-M, Li J (2007) Maxillary sinus floor augmentation using autogenous bone grafts and platelet-enriched fibrin glue with simultaneous implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 103:329–333
Leppänen O, Sievänen H, Jokihaara J, Pajamäki I, Järvinen TL (2006) Three-point bending of rat femur in the mediolateral direction: introduction and validation of a novel biomechanical testing protocol. J Bone Miner Res 21:1231–1237
Liao H-T, Chen C-T, Chen C-H, Chen J-P, Tsai J-C (2011) Combination of guided osteogenesis with autologous platelet-rich fibrin glue and mesenchymal stem cell for mandibular reconstruction. J Trauma Acute Care Surg 70:228–237
Liu X, Smith LA, Hu J, Ma PX (2009a) Biomimetic nanofibrous gelatin/apatite composite scaffolds for bone tissue engineering. Biomaterials 30:2252–2258
Liu Y, Lu Y, Tian X, Cui G, Zhao Y, Yang Q, Yu S, Xing G, Zhang B (2009b) Segmental bone regeneration using an rhBMP-2-loaded gelatin/nanohydroxyapatite/fibrin scaffold in a rabbit model. Biomaterials 30:6276–6285
Meimandi-Parizi A, Oryan A, Moshiri A (2013) Role of tissue engineered collagen based tridimensional implant on the healing response of the experimentally induced large Achilles tendon defect model in rabbits: a long term study with high clinical relevance. J Biomed Sci 20:1
Moshiri A, Shahrezaee M, Shekarchi B, Oryan A, Azma K (2015) Three-dimensional porous gelapin–simvastatin scaffolds promoted bone defect healing in rabbits. Calcif Tissue Int 96:552–564
Mozafari M, Rabiee M, Azami M, Maleknia S (2010) Biomimetic formation of apatite on the surface of porous gelatin/bioactive glass nanocomposite scaffolds. Appl Surf Sci 257:1740–1749
Nagata MJ, Melo L, Messora MR, Bomfim SR, Fucini SE, Garcia VG, Bosco AF, Okamoto T (2009) Effect of platelet-rich plasma on bone healing of autogenous bone grafts in critical-size defects. J Clin Periodontol 36:775–783
NRC (2011) Guide for the care and use of laboratory animals. National Academies Press, Washington
Oryan A, Parizi AM, Shafiei-Sarvestani Z, Bigham A (2012) Effects of combined hydroxyapatite and human platelet rich plasma on bone healing in rabbit model: radiological, macroscopical, hidtopathological and biomechanical evaluation. Cell Tissue Bank 13:639–651
Oryan A, Alidadi S, Moshiri A, Maffulli N (2014a) Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res 9:1
Oryan A, Bigham-Sadegh A, Abbasi-Teshnizi F (2014b) Effects of osteogenic medium on healing of the experimental critical bone defect in a rabbit model. Bone 63:53–60
Oryan A, Alidadi S, Bigham-Sadegh A, Moshiri A (2016a) Comparative study on the role of gelatin, chitosan and their combination as tissue engineered scaffolds on healing and regeneration of critical sized bone defects: an in vivo study. J Mater Sci Mater Med 27:155
Oryan A, Alidadi S, Moshiri A (2016b) Platelet-rich plasma for bone healing and regeneration. Expert Opin Biol Ther 16:213–232
Öztürk A, Yetkin H, Memis L, Cila E, Bolukbasi S, Gemalmaz C (2006) Demineralized bone matrix and hydroxyapatite/tri-calcium phosphate mixture for bone healing in rats. Int Orthop 30:147–152
Parizi AM, Oryan A, Shafiei-Sarvestani Z, Bigham A (2012) Human platelet rich plasma plus Persian Gulf coral effects on experimental bone healing in rabbit model: radiological, histological, macroscopical and biomechanical evaluation. J Mater Sci Mater Med 23:473–483
Parizi AM, Oryan A, Shafiei-Sarvestani Z, Bigham-Sadegh A (2013) Effectiveness of synthetic hydroxyapatite versus Persian Gulf coral in an animal model of long bone defect reconstruction. J Orthop Traumatol 14:259–268
Peter M, Binulal N, Nair S, Selvamurugan N, Tamura H, Jayakumar R (2010) Novel biodegradable chitosan–gelatin/nano-bioactive glass ceramic composite scaffolds for alveolar bone tissue engineering. Chem Eng J 158:353–361
Ranly DM, Lohmann CH, Andreacchio D, Boyan BD, Schwartz Z (2007) Platelet-rich plasma inhibits demineralized bone matrix-induced bone formation in nude mice. J Bone Jt Surg 89:139–147
Ross R, Raines EW, Bowen-Pope DF (1986) The biology of platelet-derived growth factor. Cell 46:155–169
Sánchez AR, Sheridan PJ, Kupp LI (2003) Is platelet-rich plasma the perfect enhancement factor? A current review. Int J Oral Maxillofac Implants 18:1
Sellgren KL, Ma T (2012) Perfusion conditioning of hydroxyapatite–chitosan–gelatin scaffolds for bone tissue regeneration from human mesenchymal stem cells. J Tissue Eng Regen Med 6:49–59
Shafiei-Sarvestani Z, Oryan A, Bigham AS, Meimandi-Parizi A (2012) The effect of hydroxyapatite-hPRP, and coral-hPRP on bone healing in rabbits: radiological, biomechanical, macroscopic and histopathologic evaluation. Int J Surg 10:96–101
Sohn D-S, Moon J-W, Moon K-N, Cho S-C, Kang P-S (2010) New bone formation in the maxillary sinus using only absorbable gelatin sponge. J Oral Maxillofac Surg 68:1327–1333
Takahashi Y, Yamamoto M, Tabata Y (2005) Enhanced osteoinduction by controlled release of bone morphogenetic protein-2 from biodegradable sponge composed of gelatin and β-tricalcium phosphate. Biomaterials 26:4856–4865
Thorn J, Sørensen H, Weis-Fogh U, Andersen M (2004) Autologous fibrin glue with growth factors in reconstructive maxillofacial surgery. Int J Oral Maxillofac Surg 33:95–100
Trouillas M, Prat M, Doucet C, Ernou I, Laplace-Builhé C, Saint Blancard P, Holy X, Lataillade J-J (2013) A new platelet cryoprecipitate glue promoting bone formation after ectopic mesenchymal stromal cell-loaded biomaterial implantation in nude mice. Stem Cell Res Ther 4:1
Usta M, Piech D, MacCrone R, Hillig W (2003) Behavior and properties of neat and filled gelatins. Biomaterials 24:165–172
Yazdimamaghani M, Vashaee D, Assefa S, Walker K, Madihally S, Köhler G, Tayebi L (2014) Hybrid macroporous gelatin/bioactive-glass/nanosilver scaffolds with controlled degradation behavior and antimicrobial activity for bone tissue engineering. J Biomed Nanotechnol 10:911–931
You T-M, Choi B-H, Zhu S-J, Jung J-H, Lee S-H, Huh J-Y, Lee H-J, Li J (2007) Platelet-enriched fibrin glue and platelet-rich plasma in the repair of bone defects adjacent to titanium dental implants. Int J Oral Maxillofac Implants 22:1
Zhang S, Huang Y, Yang X, Mei F, Ma Q, Chen G, Ryu S, Deng X (2009) Gelatin nanofibrous membrane fabricated by electrospinning of aqueous gelatin solution for guided tissue regeneration. J Biomed Mater Res A 90:671–679
Zhu S-J, Choi B-H, Jung J-H, Lee S-H, Huh J-Y, You T-M, Lee H-J, Li J (2006) A comparative histologic analysis of tissue-engineered bone using platelet-rich plasma and platelet-enriched fibrin glue. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 102:175–179
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gholipour, H., Meimandi-Parizi, A., Oryan, A. et al. The effects of gelatin, fibrin-platelet glue and their combination on healing of the experimental critical bone defect in a rat model: radiological, histological, scanning ultrastructural and biomechanical evaluation. Cell Tissue Bank 19, 341–356 (2018). https://doi.org/10.1007/s10561-017-9679-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-017-9679-5